Last Updated on October 21, 2025 by mcelik

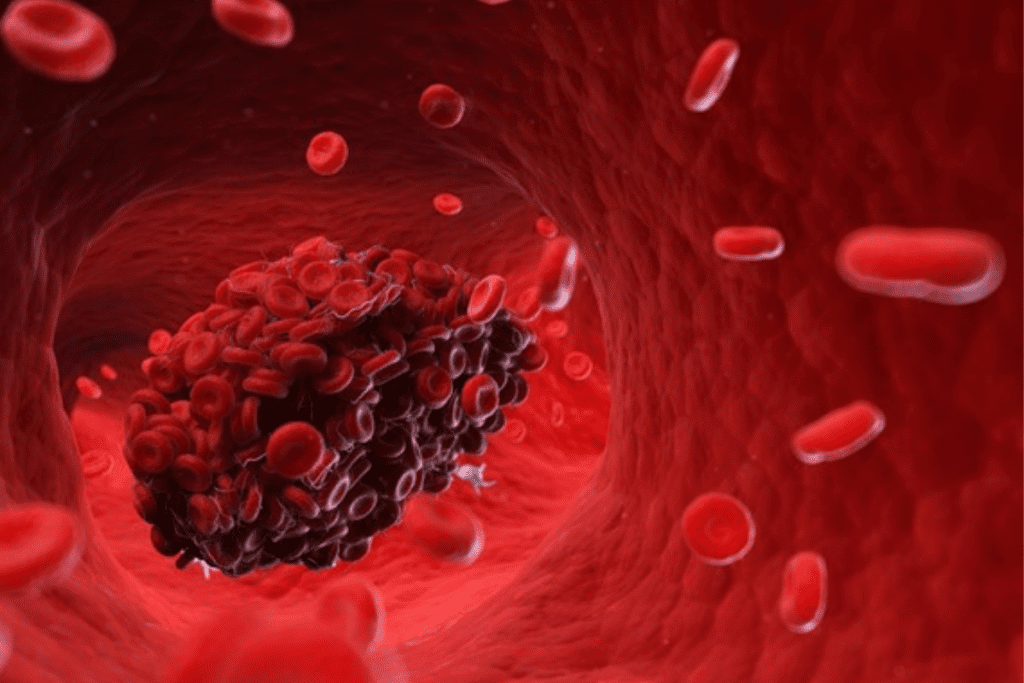
Did you know that millions of people worldwide deal with issues that mess up blood clotting? A blood clotting disorder, or coagulation disease of blood, can cause too much bleeding or unwanted clots. Both can be deadly if not treated right.
We’ll look into the various clotting disorders and their signs. This will help you grasp how complex these conditions are. It also shows why getting medical help is key.
Grasping the process of the coagulation cascade is critical for effectively treating blood clotting issues.
The process of blood clotting has several steps. First, the injured blood vessel narrows to slow down blood flow. Then, platelets stick to the injury, creating a weak plug.
This plug needs more support to become strong. The coagulation cascade, a series of chemical reactions, provides this support. It uses clotting factors, proteins in blood plasma, to make a fibrin clot.
Grasping the process of the coagulation cascade is critical for effectively treating blood clotting issues.
Grasping the process of the coagulation cascade is critical for effectively treating blood clotting issues. The right balance between clotting and dissolving is vital. Any imbalance can cause problems like blood clots or excessive bleeding.

A blood clotting disorder happens when the body’s clotting system goes wrong. This can cause too much or too little clotting. It can lead to health problems like too much bleeding or dangerous clots.
Blood clotting disorders fall into two main types: hypercoagulable states (thrombophilia) and hypocoagulable states (bleeding disorders). Hypercoagulable states make blood clot too easily, which can be harmful. Hypocoagulable states make blood hard to clot, leading to too much bleeding.
Knowing which type you have is key to finding the right treatment. Thrombophilia can be inherited or acquired. Inherited thrombophilia comes from genes, while acquired thrombophilia can be caused by many things like medicine or lifestyle.
The number of people with blood clotting disorders varies. For example, Factor V Leiden is more common in people of European descent.
Some groups are at higher risk for blood clotting disorders. For instance, VTE is more common in older people and those with a family history of blood clots.
Knowing who is at risk is important for preventing blood clotting disorders.
Grasping the process of the coagulation cascade is critical for effectively treating blood clotting issues.
Hypercoagulable states, or thrombophilia, make it easier for blood clots to form. These clots can block blood flow and cause serious problems like deep vein thrombosis (DVT) and pulmonary embolism (PE).
These conditions can be caused by genetics or other factors. Genetic causes include mutations in genes that control clotting, like Factor V Leiden. Other causes include being bedridden for too long, having cancer, or taking certain medicines.
Hypocoagulable states, or bleeding disorders, make it harder for blood to clot. This can lead to easy bruising and bleeding. These disorders can be caused by a lack or malfunction of clotting factors or platelets.
Examples of bleeding disorders include hemophilia A and B, von Willebrand disease, and platelet function disorders. Symptoms can range from simple bruising and nosebleeds to severe bleeding that can be dangerous if not treated right.
To understand the differences between hypercoagulable and hypocoagulable states, let’s look at their main features in the table below:
| Characteristics | Hypercoagulable States | Hypocoagulable States |
| Causes | Genetic mutations, prolonged immobilization, cancer | Deficiencies or dysfunction of clotting factors or platelets |
| Symptoms | Deep vein thrombosis, pulmonary embolism | Easy bruising, nosebleeds, severe bleeding episodes |
| Treatment Approach | Anticoagulant medications, lifestyle modifications | Replacement therapy, clotting factor concentrates, desmopressin |
Knowing these differences helps doctors create the right treatment plans for patients with blood clotting disorders.
Blood clotting disorders can be passed down through families. It’s important to know about these conditions to manage them well. These disorders happen because of genetic changes that affect how blood clots. This can cause too much clotting or bleeding.
Factor V Leiden is a common inherited blood clotting disorder. It’s caused by a gene mutation in the factor V gene. This makes the blood more likely to form deep vein thrombosis (DVT) and pulmonary embolism.
The prothrombin gene mutation affects how prothrombin is made. Prothrombin is key for blood clotting. People with this mutation are at higher risk of venous thromboembolism.
Proteins C and S, and antithrombin, are also important. They help control blood clotting. Without enough of these proteins, the risk of thrombosis goes up.
It’s key to understand these inherited disorders to diagnose and manage them. Genetic tests and family history help find who needs preventive care or treatment.
Acquired blood clotting disorders are not passed down through genes. Instead, they come from outside factors like medicines, health issues, or not getting enough nutrients. These can mess up how blood clots, causing too much bleeding or clots where they shouldn’t be.
Some medicines can change how our body clots blood. For example, drugs meant to stop clots can cause bleeding if not used right. On the flip side, some drugs might make it more likely to get blood clots.
Here are some examples:
Different diseases can mess with our body’s clotting. For instance, liver problems can stop the production of clotting factors, leading to bleeding. Some cancers and their treatments can also mess with clotting, raising the risk of bleeding or clotting.
These disorders can show up in many ways, like:
Vitamin K is key for making clotting factors in the liver. Not enough vitamin K can make bleeding more likely because clotting doesn’t work right. This can happen if you don’t eat enough vitamin K, can’t absorb it well, or take certain medicines that mess with how your body uses vitamin K.
To deal with vitamin K deficiency, you should:
In summary, acquired blood clotting disorders are complex and need a detailed approach to handle. By knowing the causes and symptoms of blood clot disorders, doctors can make better treatment plans. This helps lower risks and improves how patients do.
Blood clotting disorders can show up in different ways. It’s important to know the signs. These disorders can cause too much or too little clotting, each with its own symptoms.
Thrombophilia, or excessive clotting, can lead to unwanted blood clots. This can cause:
Seek medical help if these symptoms don’t go away or get worse.
On the other hand, not enough clotting can cause bleeding disorders. These include:
These symptoms can really affect your daily life. You should see a doctor to find out why.
Grasping the process of the coagulation cascade is critical for effectively treating blood clotting issues.
Many factors can increase the chance of getting a blood clotting disorder. Knowing these can help manage the condition. It’s key for prevention and treatment.
Genetics are a big part of blood clotting disorders. If your family has a history of these disorders, you’re at higher risk. Certain genes, like Factor V Leiden and prothrombin gene mutation, make clotting more likely.
Lifestyle choices also play a role. Sitting for long periods, like on long trips or after surgery, raises clot risk. Smoking and obesity are also risk factors.
Some health issues and treatments can mess with blood clotting. Cancer, heart disease, and autoimmune disorders up the risk. Also, some hormonal therapies and chemotherapy drugs can affect clotting.
Knowing these risks helps you take steps to lower your chance of a blood clotting disorder. This might mean changing your lifestyle, managing health conditions, and being aware of treatment risks.
Untreated blood clotting disorders can cause serious problems. These include life-threatening conditions that need quick medical help. They can affect many parts of our health and well-being.
Deep Vein Thrombosis is when a blood clot forms in deep veins, usually in the legs. Symptoms include swelling, pain, and redness in the affected limb. If not treated, DVT can lead to more serious problems like pulmonary embolism.
A pulmonary embolism happens when a blood clot travels to the lungs and blocks blood flow. This is a life-threatening condition that needs immediate medical care. Symptoms include trouble breathing, chest pain, and a fast heart rate.
Blood clotting disorders can also raise the risk of stroke and heart attack. A stroke is when a clot blocks blood to the brain, and a heart attack is when a clot blocks blood to the heart. Both are emergencies, with symptoms like sudden weakness, confusion, and severe chest pain.
The table below shows the main complications of untreated blood clotting disorders:
| Complication | Symptoms | Consequences |
| Deep Vein Thrombosis (DVT) | Swelling, pain, redness in the affected limb | Pulmonary Embolism |
| Pulmonary Embolism | Difficulty breathing, chest pain, rapid heart rate | Life-threatening, requires immediate medical attention |
| Stroke | Sudden weakness, confusion, difficulty speaking | Permanent brain damage, death |
| Heart Attack | Severe chest pain, shortness of breath, lightheadedness | Heart damage, death |
Knowing these complications shows why we must seek medical help if symptoms get worse. We must take blood clotting disorders seriously and manage them well to avoid these severe outcomes.
To find out if someone has a blood clotting disorder, doctors use many steps. They look at symptoms, medical history, and lab tests. They also use imaging studies.
First, doctors do a detailed check-up. They look at symptoms and medical history. They check family history and past problems with blood clots or bleeding.
Lab tests are key in finding blood clotting disorders. They check blood for clotting problems. Tests include:
These tests show how well blood clots. They help doctors decide what to do next.
Imaging tests are used for some disorders. They check for blood clots in veins or lungs. Tests include:
These tests show where clots are. They help doctors plan treatment.
Doctors use all these steps to find and treat blood clotting disorders. They make a plan based on what they find.
Managing blood clotting disorders well needs a deep understanding of treatment choices. The right treatment depends on the disorder’s type and how severe it is. It also depends on the patient’s unique situation.
Anticoagulant drugs are key in treating blood clotting disorders, mainly for those at risk of harmful clots. These drugs stop the body’s clotting process. This reduces the chance of blood clots forming.
Popular anticoagulants include warfarin, apixaban, rivaroxaban, and dabigatran. The choice depends on the patient’s condition, possible drug interactions, and if monitoring is needed.
Thrombolytic therapy is for emergencies to dissolve clots causing serious health problems. This includes acute ischemic stroke or severe pulmonary embolism. It involves drugs that break down clots.
Surgery might be needed to handle blood clotting disorder complications or to remove a clot. Surgical options include thrombectomy, where a clot is physically taken out.
| Treatment Option | Use Case | Key Benefits |
| Anticoagulant Medications | Prevention of clot formation | Reduces risk of thrombosis, available in various formulations |
| Thrombolytic Therapy | Emergency clot dissolution | Can rapidly restore blood flow, lifesaving in acute situations |
| Surgical Interventions | Removal of clots or managing complications | Can be definitive treatment for certain conditions, allows for direct clot removal |
We’ve looked at the main treatments for blood clotting disorders. It’s vital for patients to team up with their healthcare providers. Together, they can figure out the best treatment plan.
Managing blood clotting disorders requires both medical treatment and lifestyle changes. People with these conditions must take an active role in their care. This helps prevent complications and improves their quality of life.
Grasping the process of the coagulation cascade is critical for effectively treating blood clotting issues.
Compliance is key to avoid both clotting and bleeding issues. Missing doses or taking medication wrong can lessen its effectiveness.
Diet is also important in managing blood clotting disorders. Some foods can affect how well anticoagulant medications work.
While exercise is good for health, people with blood clotting disorders may need to adjust their activities. This is to lower the risk of injury or bleeding.
By making smart lifestyle choices and working with healthcare providers, people with blood clotting disorders can manage their condition well. They can live active and fulfilling lives.
Managing blood clotting disorders in special groups is complex. This includes pregnant women and children. They need specific care to reduce risks.
Pregnancy changes the body’s clotting system, raising the risk of blood clots. Women with blood clotting issues face higher risks. We must manage these conditions carefully to avoid serious problems like deep vein thrombosis (DVT) and pulmonary embolism.
A study found that pregnancy increases the risk of blood clots, more so in women with inherited clotting disorders.
“The risk of venous thromboembolism is increased during pregnancy, particularlly in women with inherited thrombophilias.”
| Condition | Risk During Pregnancy | Management Strategy |
| Factor V Leiden | High | Anticoagulant therapy |
| Prothrombin Gene Mutation | Moderate to High | Close monitoring and anticoagulation |
| Protein C, S, and Antithrombin Deficiencies | High | Replacement therapy and anticoagulation |
Children with blood clotting disorders face unique challenges. Diagnosing these conditions in kids requires a different method than adults. This is because coagulation test ranges change with age.
Key considerations in managing pediatric blood clotting disorders include:
We must take a thorough and caring approach to manage blood clotting disorders in special populations. This ensures we meet their unique needs and circumstances.
It’s important to know when to get medical help if you have a blood clotting disorder. People with these conditions should watch for signs that mean they need to see a doctor right away. This can help avoid serious problems.
Emergency signs are severe symptoms that could mean a serious problem. They include:
These symptoms need immediate medical attention.
Some symptoms are not as urgent but should be checked by a doctor soon. These include:
If you notice any of these, it’s important to talk to your doctor.
| Symptom Category | Specific Symptoms | Action Required |
| Emergency Warning Signs | Severe bleeding, chest pain, difficulty breathing, severe headache, confusion, weakness or numbness | Immediate Medical Attention |
| Symptoms Requiring Prompt Evaluation | Unusual bruising, prolonged bleeding, frequent nosebleeds, blood in urine or stool | Prompt Evaluation by Healthcare Provider |
Grasping the process of the coagulation cascade is critical for effectively treating blood clotting issues.
We’re moving towards more effective and personalized treatment options. This shift is making a big difference in how we care for our patients.
Novel anticoagulants are a big step forward in preventing and treating blood clots. They are safer and easier to dose than older treatments. For example, DOACs like rivaroxaban and apixaban are popular because they work well and don’t need as much monitoring.
| Novel Anticoagulant | Mechanism of Action | Clinical Use |
| Rivaroxaban | Direct Factor Xa inhibitor | Prevention of stroke in atrial fibrillation, treatment of DVT/PE |
| Apixaban | Direct Factor Xa inhibitor | Prevention of stroke in atrial fibrillation, treatment of DVT/PE |
| Edoxaban | Direct Factor Xa inhibitor | Prevention of stroke in atrial fibrillation, treatment of DVT/PE |
Gene therapy is a promising treatment for bleeding disorders like hemophilia A and B. It aims to fix the genetic defect causing the condition. This could potentially cure it. Early clinical trials show promising results, with some patients achieving normal clotting function after just one treatment.
Key Benefits of Gene Therapy:
Personalized medicine is changing how we manage blood clotting disorders. It tailors treatment to each person’s genetic and clinical profile. This means doctors can predict and prevent blood clots or bleeding more accurately.
Genetic testing and data analysis are driving this trend. They help us find the best treatment for each patient. This approach is making care more precise and effective.
The integration of new treatments and research is transforming blood clotting disorder management. As we learn more, we can provide better care for our patients.
Grasping the process of the coagulation cascade is critical for effectively treating blood clotting issues.
These conditions need a full care plan. Knowing the signs helps people get help fast. With the right treatment, they can live active lives.
New treatments and ways to manage these disorders are being found. It’s important to keep up with these advances for both patients and doctors.
To manage blood clotting disorders well, awareness and proper care are needed. Working with healthcare teams helps people control their condition. This improves their life quality.
A blood clotting disorder, also known as a coagulation disorder, affects how blood clots. It can cause too much bleeding or clotting.
Symptoms vary by disorder type. For those who clot too much, you might see pain, swelling, and redness in a limb. Those who bleed too much might notice easy bruising, frequent nosebleeds, and heavy periods.
These disorders can come from genetics, lifestyle, or medical conditions. Some are inherited, while others are not.
Diagnosis involves clinical checks, lab tests, and imaging. Lab tests might include clotting factor assays, genetic tests, and blood counts.
Treatment varies by disorder type and severity. It might include anticoagulant meds, thrombolytic therapy, or surgery.
Managing it might mean taking meds, watching your diet, and adjusting your activities. Working with a healthcare provider is key to a good plan.
Certain foods and supplements can affect clotting or interact with meds. Always talk to a healthcare provider about your diet.
Some can be managed well with treatment, but a cure isn’t always possible. Ongoing care and monitoring are often needed.
Untreated disorders can lead to serious issues like deep vein thrombosis, pulmonary embolism, stroke, and heart attack.
Yes, research and new treatments are emerging. This includes novel anticoagulants, gene therapy, and personalized medicine.
These disorders can have unique effects on special groups. Pregnant women and children need careful management to avoid risks.
Seek immediate medical help for emergency signs like severe pain, trouble breathing, or severe bleeding.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!