Last Updated on October 21, 2025 by mcelik

Nearly 900,000 Americans face blood clots each year. Many cases could be prevented or treated early if caught. It’s important to know the risks and signs to manage your health.Our ultimate guide on how to diagnose blood clots is essential reading. Discover the powerful, amazing tests doctors use for this critical task.
We’ll show you how to check for blood clots and when to get medical help. Being in tune with your body and knowing the signs of blood clots can save lives.
Early detection is key to avoiding serious problems. By knowing what to look for, you can take steps to keep yourself healthy.
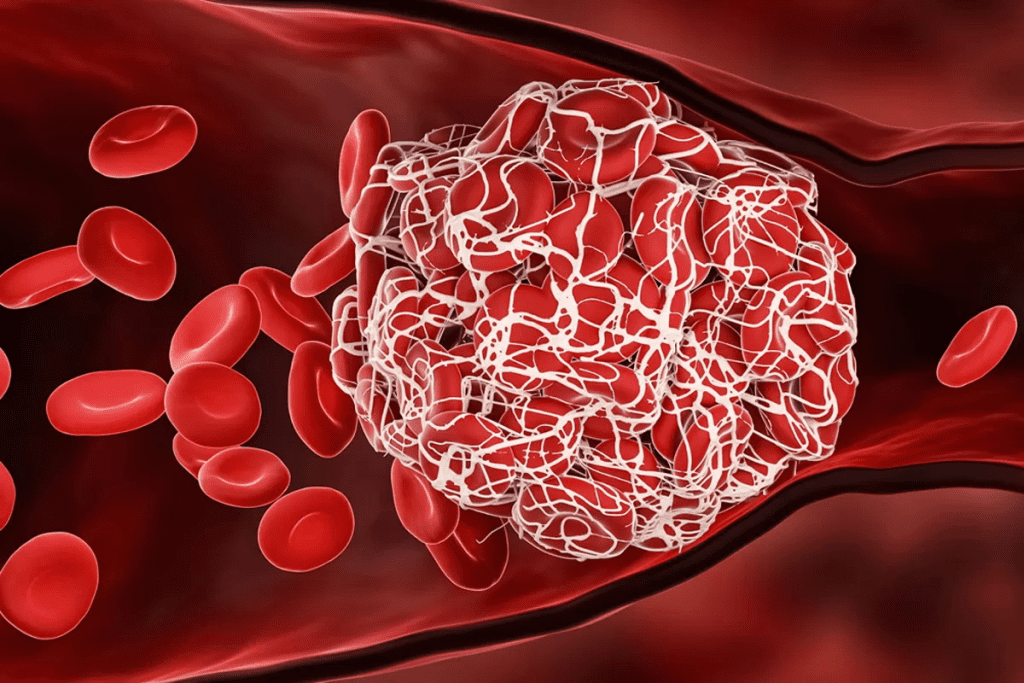
It’s important to know about blood clots to understand the risks they pose. They form as a natural response to injury, helping to stop too much bleeding. But, if they form in the wrong place or break loose, they can cause serious problems like deep vein thrombosis (DVT) or pulmonary embolism (PE).
The blood clotting process, or coagulation, is complex. It starts with platelets gathering at an injury site, forming a plug. Then, a series of chemical reactions leads to the creation of fibrin, which strengthens the plug and forms a clot.
The coagulation cascade has three main pathways: intrinsic, extrinsic, and common. The intrinsic pathway is triggered by damage inside the body. The extrinsic pathway is caused by external trauma. Both lead to the common pathway, where thrombin and fibrin are formed.
Not all blood clots are harmful. They are a natural response to injury, helping to stop bleeding. Once the injury heals, the body dissolves these clots, a process called fibrinolysis. But, abnormal clots can form without injury or not dissolve, posing serious risks.
Blood clots frequently occur in the legs and lungs.
Blood clots frequently occur in the legs and lungs.
| Condition | Description | Risks |
| Deep Vein Thrombosis (DVT) | Clot forms in the deep veins, typically in the legs. | Can lead to pulmonary embolism if the clot breaks loose. |
| Pulmonary Embolism (PE) | Clot travels to the lungs, obstructing blood flow. | Can be life-threatening, causing sudden death or serious injury. |
Understanding blood clots and their formation is key to recognizing risks and preventing them. Knowing how they form and when they’re dangerous helps individuals assess their risk and seek medical help when needed.
Blood clots frequently occur in the legs and lungs.
DVT is when a blood clot forms in the deep veins, usually in the legs. It’s important to know the signs of DVT to stop it from getting worse.
A pulmonary embolism happens when a blood clot travels to the lungs. This is a serious condition that needs quick medical help.
Doctors use tests and checks to find pulmonary embolism.
Blood clots can also form in the brain, abdomen, and arms. Each place has its own problems and signs.
Knowing these different signs is important for quick diagnosis and treatment.
Many things, like your genes and lifestyle, can make you more likely to get blood clots. Knowing these risk factors helps you take steps to prevent them. It also helps you spot the signs early.
Some people are more likely to get blood clots because of their genes. Family history is a big factor; if your family has had blood clots, you might be at higher risk. Certain genetic conditions, like Factor V Leiden, can make blood clot more easily.
What you do every day can also affect your risk of blood clots. For example:
Some health issues can also up your risk of blood clots. These include:
Some medicines can also affect your blood’s clotting, raising your risk. These include:
Knowing these risk factors helps you and your doctor take steps to lower your risk of blood clots. If you’re worried, talk to your healthcare provider about your situation.
Deep Vein Thrombosis (DVT) often shows signs that are easy to miss. But knowing these signs can save lives. Spotting them early is key to avoiding serious problems.
One common sign of DVT is pain or tenderness in the leg. This pain can feel like cramping or soreness. It can be mild or very severe.
Swelling in the affected leg is another sign. This swelling can make the leg look bigger than usual.
Key areas to watch for pain and swelling include:
DVT can also change the skin of the affected leg. The skin may turn red or discolored. It might feel warm or hot.
Noting these changes can be critical:
In some cases, DVT makes veins in the affected leg more visible. You might also feel a heavy or aching feeling in the leg.
DVT usually affects one leg at a time. If you have symptoms in both legs, it might be something else. But if one leg is much more swollen or painful, it could be DVT.
Being aware of these differences can help in diagnosing DVT:
While doctors are the best for diagnosing blood clots, some self-checks can give clues. These methods are not a full replacement for a doctor’s check-up. But, they can help you know when to see a doctor.
The Homan’s Sign Test is easy. It involves lifting your foot up. Pull your toes back toward your shin gently. If your calf or knee behind it hurts, it might mean a blood clot. But, remember, this test is not always right and can sometimes be wrong.
Another way to check is by measuring your leg size. Swelling from a blood clot can make one leg bigger. Use a tape measure around the widest part of your calf or thigh. If one leg is more than 1 inch bigger, it could mean swelling from a blood clot.
Pain from blood clots can be different. For DVT, pain usually happens in one leg, in the calf or thigh. It might feel like cramping or soreness. Watching how long the pain lasts and if it changes can help.
If the pain is very bad, gets worse, or comes with swelling or redness, get medical help right away.
These self-checks can give hints, but they have big limits. Many blood clots don’t show symptoms until they’re serious. And, not having symptoms doesn’t mean there’s no clot.
If you think you might have a blood clot or are at risk, see a doctor. They can give the right diagnosis and treatment plan.
It’s important to know the signs of pulmonary embolism to get help fast. This condition happens when a blood clot blocks blood flow in the lungs. It can be very dangerous and even deadly if not treated right away.
Suddenly finding it hard to breathe is a common sign. You might also feel pain in your chest. This pain can get worse when you breathe deeply, cough, or move around a lot. If you have these symptoms, you should see a doctor right away.
A fast or irregular heartbeat can also be a sign. The heart tries to work harder because of the blockage. This can make your heart beat strangely or irregularly.
Coughing up blood or bloody sputum is another warning sign. It’s scary, but it’s a sign you need to see a doctor fast.
Feeling dizzy, sweating a lot, or feeling like you’re going to die can also be signs. In bad cases, you might pass out or turn blue because you’re not getting enough oxygen.
If you notice any of these symptoms, don’t wait. Getting help quickly is key to avoid serious problems, including death. Knowing these signs can help you get the care you need fast.
Blood clots frequently occur in the legs and lungs. But they can also form in other parts of the body. It’s important to know the signs of blood clots in these areas to get medical help quickly.
Abdominal blood clots can cause a lot of pain, nausea, and vomiting. These symptoms might look like other health issues. If you have severe and ongoing abdominal pain, get medical help right away.
Blood clots in the brain can lead to a stroke. Symptoms include sudden weakness, trouble speaking, or vision changes. Get help fast if you or someone else shows these signs.
Arm blood clots can cause swelling, pain, and color changes. They are less common than leg clots but are serious. If you notice these signs, see a doctor, even after surgery or when you’re not moving much.
Renal vein thrombosis is a blood clot in the veins that drain the kidneys. Symptoms include flank pain, blood in the urine, and kidney problems. This needs quick medical attention.
Knowing about these unusual locations and their symptoms can help in early detection and treatment of blood clots. If you notice any of these signs, don’t wait to get medical care.
Knowing when to seek medical help for blood clots is key. Blood clots can be deadly if not treated fast. We’ll cover the urgent situations that need medical care right away.
Certain symptoms mean you need to act fast. Severe breathing trouble, chest pain, or coughing up blood could mean a pulmonary embolism. Severe leg pain or swelling might be a sign of deep vein thrombosis (DVT). If you see these signs, don’t wait.
Other symptoms need quick medical help. Sudden confusion, trouble speaking, or weakness could be a stroke. Severe abdominal pain or vomiting blood are also urgent signs.
When calling for help, share all you can about your symptoms. Tell them when your symptoms started, how bad they are, and what makes them better or worse. This info helps responders a lot.
Before going to the emergency room, collect any important medical info. List your medications, allergies, and medical history. This helps doctors make quick, informed decisions.
Doctors stress that quick action with blood clots can save lives. Knowing the emergency signs and how to act can be life-saving.
Diagnosing blood clots needs a mix of medical skills and advanced tests. When symptoms suggest a blood clot, doctors use different methods. These help confirm the clot’s presence, location, and how serious it is.
Ultrasound is a key tool for finding blood clots in the legs. It uses sound waves to show blood vessel images. Doppler ultrasound checks blood flow to spot clots and see their effect on blood movement.
“Ultrasound is great for finding deep vein thrombosis (DVT),” says experts. It lets doctors see the clot’s size and where it is.
The D-dimer test checks for a protein fragment called D-dimer in the blood. This protein is made when a clot breaks down. But, a high D-dimer level can mean many things, not just clots.
So, doctors use D-dimer tests with other methods. This helps figure out if a clot is there or not.
For tricky spots like the lungs or brain, doctors use CT scans and MRIs. CT scans give detailed images and are good for lung clots. MRIs show clots in the brain and other areas.
These tests are very good at showing what’s going on. They give doctors a lot of information about the clot and the area around it.
Some cases need special tests. Venography uses dye to see veins on an X-ray. It gives clear pictures of veins and can spot clots.
Other tests, like pulmonary angiography for lung clots or cerebral angiography for brain clots, are also used. These tests help doctors make the right treatment plans.
This information enhances your understanding of how medical professionals diagnose blood clots.
Learning about the steps to find blood clots can make you feel less worried. The process is detailed, with many steps to find and locate blood clots accurately.
When you see your doctor, they will start with a physical check-up. Your doctor will look at your overall health, searching for signs like swelling, redness, or warmth in your limbs. This helps spot areas that might need more tests.
Talking about your medical history is key to finding blood clots. Your doctor will ask about your symptoms, lifestyle, and health background. They want to know about recent surgeries, long periods of sitting, or if your family has blood clot issues. This info helps figure out your risk and guides the tests.
After the first check-up and talking about your health, your doctor might suggest more tests. Tests like ultrasound, D-dimer blood tests, and CT scans are common. They help see the blood clot, where it is, and how big it is.
After the tests, your doctor will talk about the results with you. Understanding your test results is important for planning your treatment. They will explain what the tests show, how serious the clot is, and what treatment you need.
Knowing about the steps to find blood clots can help you feel more prepared for your doctor’s visit. This information enhances your understanding of how medical professionals diagnose blood clots.
Blood tests are key in finding blood clots. Knowing how they work is vital for good medical care. Tests on blood are essential for spotting and handling blood clots.
D-dimer testing is a common blood test for finding blood clots. It checks for D-dimer, a protein piece made when a clot breaks down. High D-dimer levels suggest a blood clot, but this test isn’t perfect on its own.
This test is great for ruling out blood clots in people who are unlikely to have them. It’s very sensitive but not very specific. This means it can show positive results for things other than blood clots, like recent injuries or cancer.
There are other blood markers that help understand blood clotting. These include:
Even though blood tests are helpful, they have downsides. D-dimer testing can give false positives, causing extra tests and worry for patients. Also, blood tests can’t confirm blood clots by themselves. They need to be looked at with symptoms and imaging results.
Blood tests are best used wisely, based on how likely a clot is. For example, a negative D-dimer test can clear out DVT or PE in people with low risk.
In summary, blood tests, like D-dimer, are key in finding blood clots. Knowing their good and bad points helps doctors make better choices.
It’s important to know the difference between blood clots and other conditions that look similar. Blood clots can be mistaken for many other health problems. Knowing the unique signs of blood clots is key to getting the right treatment.
It can be hard to tell if you have a muscle strain or Deep Vein Thrombosis (DVT). Both can cause pain and swelling in your legs. But, muscle strains usually come from overexertion and get worse with movement.
DVT, on the other hand, starts slowly and may cause swelling, warmth, and redness. Seeking medical help is vital if you’re not sure, as DVT can be deadly if not treated quickly.
Heart attacks and pulmonary embolisms (PE) can also be confused. Both can cause sudden chest pain and trouble breathing. But, they need different urgent care.
A heart attack blocks blood to the heart, while a PE blocks blood in the lungs. Signs like sudden pain and trouble breathing mean you need to see a doctor right away.
Cellulitis, a skin infection, can look like DVT because of similar symptoms like redness and swelling. But, cellulitis usually has more skin changes and might make you feel feverish. Knowing the difference is important because you need antibiotics for cellulitis and blood thinners for DVT.
Other things that might look like blood clots include superficial thrombophlebitis, varicose veins, and some muscle problems. Each has its own signs and treatments. For example, superficial thrombophlebitis is a vein issue near the skin’s surface and can cause pain and redness.
Getting a correct diagnosis from a doctor is essential to choose the right treatment.
To lower your risk of blood clots, taking action is key. This means making lifestyle changes and sometimes using medicine.
Exercise is a must to prevent blood clots. It boosts blood flow, which helps avoid clots. Try to do moderate activities like brisk walking, cycling, or swimming for 30 minutes daily.
Tips for adding movement to your day:
Drinking enough water and eating right are also important. Water keeps blood flowing smoothly. Eating foods like fruits, veggies, and whole grains helps your blood vessels stay healthy.
Nutritional tips for blood clot prevention:
| Nutritional Element | Benefit for Blood Clot Prevention | Food Sources |
| Omega-3 Fatty Acids | Reduces inflammation | Salmon, Walnuts, Flaxseeds |
| Vitamin K | Essential for blood clotting regulation | Leafy Greens (Spinach, Kale), Broccoli |
| Fiber | Supports overall vascular health | Whole Grains, Fruits, Vegetables |
Compression stockings are great for those at risk of blood clots, like when traveling or sitting for a long time. They help keep blood flowing in your legs, which lowers clot risk.
Guidelines for using compression stockings:
For some, medicine is needed to stop blood clots. Anticoagulant drugs can cut down clot risk, mainly for those with DVT or pulmonary embolism history.
Considerations for anticoagulant therapy:
Treating blood clots depends on the clot’s size, where it is, and the patient’s health. Knowing these options is key to managing the condition well.
Anticoagulants are often the first treatment for blood clots. They don’t dissolve the clot but stop it from growing and prevent new ones. Drugs like heparin and warfarin are common, with newer options like rivaroxaban and apixaban also available.
Key Considerations:
Thrombolytic therapy is for severe cases, like large clots causing serious symptoms. This treatment uses drugs to dissolve the clot. It’s for patients at high risk of complications from the clot.
“Thrombolytic therapy can be lifesaving for patients with massive pulmonary embolism or severe deep vein thrombosis.” –
AHA Journal
In some cases, surgery is needed. This includes procedures like thrombectomy, where the clot is removed surgically. Surgery is considered when other treatments fail or are not viable.
| Treatment Option | Description | Typical Use Case |
| Anticoagulant Medications | Prevent clot growth and new clot formation | First-line treatment for most blood clots |
| Thrombolytic Therapy | Dissolve the clot | Severe cases, high-risk patients |
| Surgical Interventions | Surgically remove the clot | When other treatments are not viable |
Recovering from a blood clot means treating the clot and preventing future ones. Patients are often advised on lifestyle changes, like moving more, eating right, and using compression stockings.
Understanding blood clot treatment options helps patients take charge of their recovery. By working with healthcare providers, individuals can find the best treatment for their situation.
High-risk groups should know they are more likely to get blood clots. This is because of their health, lifestyle, or other factors. It’s important for them to take steps to prevent this.
Pregnant women face a higher risk of blood clots. This is because of changes in their blood and increased pressure in veins. The risk is higher in the third trimester and after giving birth.
To lower this risk, pregnant women should drink plenty of water. They should also avoid sitting for long periods. Wearing compression stockings, if advised by a doctor, can also help.
Cancer patients are more likely to get blood clots. This is because tumors can make substances that trigger clotting. Some cancers, like pancreatic cancer, increase this risk even more.
Cancer patients should talk to their doctor about their risk. They might need to take medicines to prevent blood clots or use devices to help prevent them.
People who have had surgery are at risk of blood clots. This risk is higher if they had major surgery or have been sitting for a long time. This is true for surgeries like hip or knee replacements.
To lower this risk, post-surgical patients should move around as much as they can. They should wear compression stockings if told to. They might also need to take medicines to prevent blood clots.
Travelers on long trips, like flights or car rides over four hours, are at higher risk. Sitting for a long time and cramped spaces can increase this risk.
To reduce this risk, travelers should drink plenty of water. They should also get up and move around regularly. Wearing compression stockings can also help.
| High-Risk Group | Risk Factors | Preventive Measures |
| Pregnant Women | Changes in blood clotting factors, venous pressure | Stay hydrated, avoid prolonged immobility, compression stockings |
| Cancer Patients | Tumor-produced substances activating clotting system | Anticoagulant medications, mechanical compression devices |
| Post-Surgical Patients | Major surgery, prolonged immobility | Mobilization, compression stockings, anticoagulant prophylaxis |
| Long-Distance Travelers | Prolonged immobility, cramped seating | Stay hydrated, regular breaks to move, compression stockings |
Getting a correct diagnosis is key to managing blood clots well. We’ve talked about how to check yourself, but seeing a doctor is vital. They can spot and treat blood clots accurately.
It’s important to see a doctor fast. Quick action can greatly help your health. Doctors use tests like ultrasound, D-dimer blood tests, and CT scans to find blood clots.
This information enhances your understanding of how medical professionals diagnose blood clots.
We stress the need to see doctors for blood clot diagnosis. This ensures people get the right care and treatment. Together, we can aim for better health results.
Signs include leg pain or swelling, skin changes, and visible veins. For pulmonary embolism, look out for breathing difficulties, chest pain, and heart rate changes.
Try the Homan’s Sign Test, measure leg circumference, and watch for pain patterns. But, these methods aren’t perfect. A doctor’s diagnosis is best.
Risks include genetic factors, lifestyle choices, medical conditions, and some medications. Knowing these can help prevent blood clots.
Yes, tests like D-dimer can detect blood clots. But, they’re most useful with other tests.
Treatments include anticoagulant meds, thrombolytic therapy, and surgery. The right treatment depends on the clot’s location and severity.
Move and exercise, stay hydrated and eat well, wear compression stockings, and consider medications. Knowing your risks helps prevent blood clots.
Symptoms include breathing trouble, chest pain, and heart rate changes. Also, coughing and blood in sputum are signs. Recognizing these can save lives.
Get help fast for severe chest pain, breathing trouble, or leg pain. Also, seek help for sudden swelling, redness, or warmth in a limb.
Doctors use ultrasound, D-dimer tests, CT scans, and venography. These tests help diagnose blood clots accurately.
Pregnant women, cancer patients, post-surgical people, and long-distance travelers are at higher risk. They need extra care and monitoring to prevent blood clots.
Yes, blood clots can be mistaken for muscle strains or cellulitis. A detailed diagnostic process is key to correct diagnosis.
RadiologyInfo. (2024, March 10). Blood clots – Diagnosis, evaluation and treatment. https://www.radiologyinfo.org/en/info/bloodclot
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!