Last Updated on October 21, 2025 by mcelik
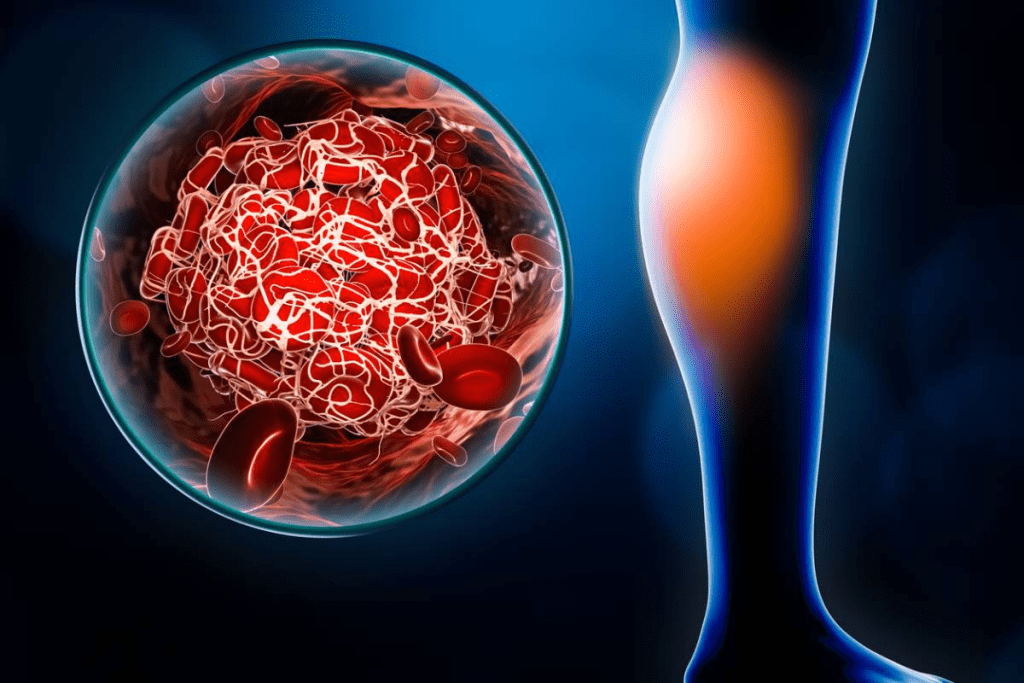
Blood coagulation disorders affect millions worldwide, putting them at risk for serious complications. Timely intervention is key to prevent these outcomes. Research, like the ACUMEN Trial on melatonin for neonatal encephalopathy, shows the need for effective blood clot treatment strategies.
This article examines various strategies for managing blood coagulation disorders. This includes blood clotting medication and making lifestyle changes. Knowing these options is vital for better patient care.

The body’s blood clotting system is complex. Disorders in this system can cause serious health problems. It’s important to understand these conditions.
Blood coagulation disorders affect how the body forms clots. Clots are key to stopping bleeding when a blood vessel is hurt.
Blood coagulation disorders make it hard for the body to form blood clots. These can be present at birth or develop later due to various reasons. “Coagulation disorders can significantly impact an individual’s quality of life, necessitating a thorough understanding for effective management,” say medical experts.
There are several common blood clotting disorders. These include:
Knowing these disorders is key to diagnosing and treating them.
The normal blood clotting process involves several steps. It starts with the blood vessel constricting to reduce blood flow. Then, platelets gather to form a plug.
The coagulation cascade follows, involving various clotting factors. This leads to fibrin formation, which stabilizes the clot. “The coagulation cascade is a finely tuned process, and any disruption can lead to either excessive bleeding or inappropriate clot formation,” showing the importance of a balanced clotting mechanism.
Understanding this process is essential to knowing how coagulation disorders occur and how to manage them.

It’s key to know the signs of blood clotting disorders to avoid serious health issues. These disorders can show up in different ways. This depends on whether there’s too much or too little clotting.
Too much clotting can cause dangerous blood clots. These can block blood flow to important organs. Symptoms may include:
Not enough clotting can lead to too much bleeding. Common symptoms include:
It’s important to spot these symptoms early to avoid worse problems.
Certain symptoms need quick medical help. If you experience:
Go to the emergency room right away. Quick treatment can greatly improve your chances of recovery.
We stress the need to listen to your body and get medical help when needed. Catching and treating blood clotting disorders early can greatly help manage them.
Diagnosing blood coagulation disorders needs a detailed approach. We use many medical tests and evaluations. These tools help us find the causes of clotting disorders and create effective treatment plans.
Blood tests are key in finding clotting disorders. They check for problems in blood clotting factors, platelets, and other parts that affect coagulation.
Imaging studies also help diagnose blood clots and see their effects on the body.
Genetic testing is sometimes suggested for inherited clotting disorders.
By combining these diagnostic tests’ results, we can accurately diagnose blood coagulation problems. Then, we create personalized treatment plans.
We use many medical treatments for blood clots. These include anticoagulant medications and surgical options. The right treatment depends on the clot’s type and how severe it is.
First, we check the patient’s condition carefully. We look at the clot’s size, location, and the patient’s health. This helps us create a treatment plan just for them.
Anticoagulant drugs are key in treating blood clots. They stop new clots from forming and prevent existing ones from growing. Drugs like heparin, warfarin, and DOACs are common.
For serious clots, we might use thrombolytic therapy. This treatment breaks down clots with special drugs. It’s used in emergencies, like during a heart attack or stroke.
Sometimes, surgery is needed to remove a blood clot. This can include procedures like thrombectomy, where the clot is removed surgically.
| Treatment | Application | Benefits | Risks |
| Anticoagulant Medications | Prevent new clots and stop existing clots from growing | Effective in managing clotting disorders, reduces risk of complications | Bleeding risk, drug interactions |
| Thrombolytic Therapy | Dissolve clots in emergency situations | Can be lifesaving in acute situations like heart attack or stroke | High risk of bleeding, limited window for administration |
| Surgical Interventions | Remove clots directly | Immediate removal of clot, can be used when other treatments are not suitable | Surgical risks, recovery time |
Anticoagulant medications are key in managing blood clotting issues. They help prevent blood clots or stop them from growing. It’s important to know how they work, their benefits, and possible side effects.
Heparin has been used for many years to prevent blood clots. It works by activating a natural anticoagulant in the body. Low-molecular-weight heparins (LMWHs), like enoxaparin, are easier to manage because of their predictable effects.
“The use of LMWHs has made treating patients easier, even outside the hospital,” says a clinical expert. This change has helped patients and saved healthcare resources.
Warfarin is another long-used anticoagulant. It stops the liver from making certain clotting factors. But, it needs regular blood tests to work right. Its narrow range and many drug interactions make it tricky to manage.
DOACs, like dabigatran and rivaroxaban, are popular for their predictable effects. They directly block either thrombin or factor Xa. This makes them easier to use than warfarin.
Antiplatelet drugs, such as aspirin and clopidogrel, prevent arterial clots. They are used to prevent heart attacks and strokes. They work by stopping platelets from sticking together.
In summary, anticoagulant medications are vital for managing blood clotting disorders. Knowing the different types and how they work helps doctors choose the best treatment. This improves patient outcomes and quality of life.
Blood clotting medications save lives but also have risks and side effects. It’s key to know these to manage them well.
Bleeding is a big risk with these medications. Anticoagulants stop new clots and slow down old ones. But, they also make it harder for the body to stop bleeding. This can lead to:
Knowing these risks and when to get help is important. Severe bleeding that doesn’t stop after 10-15 minutes needs immediate care. Also, bleeding without a clear cause needs medical help right away.
Drug interactions are a big deal for those on blood clotting meds. Some meds can make bleeding risk higher or lower the drug’s effect. Common ones include:
| Interacting Medication | Potential Effect |
| NSAIDs (e.g., ibuprofen, naproxen) | Increased risk of bleeding |
| Certain antibiotics (e.g., clarithromycin, erythromycin) | Increased anticoagulant effect |
| Antifungal medications (e.g., ketoconazole) | Increased anticoagulant effect |
| Vitamin K supplements | Reduced anticoagulant effect (for warfarin) |
Tell your doctor about any new meds, including over-the-counter ones and supplements. This helps avoid bad interactions.
Regular checks are key for those on these meds. Blood tests check how well the blood clots. For warfarin users, the INR test is common. How often you need these tests depends on your meds and health.
Monitoring makes sure the dose is right. This lowers the risk of clots and bleeding.
Handling side effects needs a proactive plan. Learn to:
Knowing the risks and side effects helps manage your condition better. This improves your life quality.
This article examines various strategies for managing blood coagulation disorders.
Factor replacement therapy is key for treating bleeding disorders like hemophilia A and B. It involves giving a clotting factor that’s missing. This helps the body clot blood properly, reducing bleeding risks.
The treatment’s frequency and amount depend on the disorder’s severity, the patient’s weight, and activity level. Regular treatment can prevent joint damage and other bleeding complications.
Desmopressin, or DDAVP, is a hormone used for mild hemophilia A and some von Willebrand disease. It boosts the levels of clotting factors in the blood. This is done by releasing stored factors into the bloodstream.
DDAVP is given through an IV or a nasal spray. It’s a convenient option for mild bleeding disorders. But, it doesn’t work for all bleeding disorders.
Antifibrinolytic medications, like tranexamic acid and epsilon-aminocaproic acid, help keep clots stable. They prevent clots from breaking down too soon. These drugs are often used with other treatments to improve their results.
By stopping the fibrinolytic process, these medications keep clots strong. This reduces the chance of bleeding again. They’re helpful during surgeries or dental work.
Hemophilia, a genetic disorder, needs specific treatments. Treatments include factor replacement therapy and other strategies. These include preventing bleeding, keeping joints mobile, and genetic counseling for families.
New treatments for hemophilia, like extended half-life clotting factors and gene therapy, offer hope. They aim to improve management and possibly cure the condition in the future.
Knowing what to do in a severe blood clot situation is key. These are medical emergencies that need quick action.
It’s important to spot the signs of a clotting emergency. Look for sudden severe pain, swelling, or color changes in a limb. Chest pain or trouble breathing could mean a pulmonary embolism or heart attack.
If you see these signs, get medical help fast. Waiting too long can cause serious harm or even death.
At the hospital, patients get a quick check-up. The treatments might include:
These steps are key to managing severe blood clots and avoiding long-term damage.
After the emergency, ongoing care is vital for healing. This care might include:
Follow-up care is critical to ensure treatment works and to handle side effects. Patients should work with their doctors to plan for the long term.
Understanding emergency treatments for severe blood clots and the importance of ongoing care helps patients handle these critical situations better.
Learning how to prevent blood clots is key to avoiding serious health issues. Blood clots can cause deep vein thrombosis (DVT), pulmonary embolism, and stroke. To prevent these, it’s important to assess risk, use medications, and use mechanical methods. Also, take extra care during high-risk times.
First, figure out your risk of getting blood clots. Risk factors include clotting disorders, recent surgery, long periods of sitting, cancer, and genetic issues like Factor V Leiden. “Knowing who’s at high risk helps target prevention,” says a top hematology expert.
People with clotting history or high risk should get regular checks. Look at their medical history, lifestyle, and genes to find the best prevention plan.
Medicines are key in stopping blood clots. Anticoagulants like heparin, warfarin, and DOACs are used. They stop clots from forming by slowing down the clotting process.
There are also mechanical ways to prevent blood clots. Compression stockings help blood flow in the legs, lowering DVT risk. IPC devices are also used in hospitals for those at high risk.
Times like surgery or long sitting increase blood clot risk. It’s vital to take preventive steps during these times. We suggest using both medicines and mechanical methods to lower risk.
For example, surgery patients might get anticoagulant meds before and after. Wearing compression stockings or using IPC devices can also help.
By knowing how to prevent blood clots, you can lower your risk of clotting disorders. Always talk to your doctor to find the best prevention plan for you.
Managing blood clotting disorders during pregnancy is a big challenge. Pregnancy increases the risk of blood clots. So, we need a careful plan that looks at both the mother’s and baby’s health.
Pregnant women with blood clotting disorders need specialized care. We must adjust treatment plans because pregnancy changes blood clotting.
The risk of blood clots in the veins is higher for pregnant women. So, it’s important to check for this risk and take steps to prevent it.
| Risk Factor | Preventive Measure |
| History of VTE | Anticoagulant therapy |
| Family history of VTE | Close monitoring |
| Known thrombophilia | Anticoagulant therapy |
Choosing the right medication for blood clots during pregnancy is key. Low molecular weight heparin (LMWH) is often safe because it doesn’t pass through the placenta much.
We must think about the benefits and risks of these medications. We need to make sure they help the mother without harming the baby.
It’s important to keep a close eye on pregnant women with blood clotting disorders. We need to check their clotting status and the baby’s health often.
Planning for delivery is a team effort. We work together to make sure the mother’s blood clotting disorder is managed during and after delivery.
To manage blood clots well, making lifestyle changes is key. These changes can help your medical treatments work better and improve your health.
Being active is important for those with blood clotting issues. Exercise boosts blood flow, which lowers clot risk. Try walking, swimming, or cycling, as they’re easy on the body and fit all fitness levels.
Avoid sitting or lying down for too long, like on long flights or in bed. Jobs that keep you sitting all day need breaks to stretch and move.
Eating right is also key in managing blood clots. Foods like salmon and sardines, full of omega-3s, help your heart and reduce inflammation. Eating more fruits, veggies, and whole grains is good for your heart too.
Watch what you eat, as some foods can affect clotting. Foods high in vitamin K, like leafy greens, can fight the effects of some blood thinners. Talk to a doctor or dietitian to make a diet plan that’s right for you.
Drinking enough water is vital for healthy blood flow and avoiding dehydration. Dehydration can make blood thicker and clot more easily. Drink at least eight glasses of water a day.
Keeping a healthy weight is also important for managing blood clots. Being overweight can strain your body and increase clot risk. Eating well and exercising regularly can help you stay at a healthy weight.
| Lifestyle Modification | Benefits for Blood Clot Management |
| Regular Exercise | Improves circulation, reduces clot risk |
| Balanced Diet | Supports heart health, reduces inflammation |
| Adequate Hydration | Maintains healthy blood flow, prevents dehydration |
| Healthy Weight | Reduces strain on the body, lowers clot risk |
Natural and alternative therapies are becoming more popular for treating blood clots. People are looking for ways to complement traditional medical treatments.
Some natural remedies show promise in managing blood clots. These include:
Certain supplements can influence blood clotting, either by promoting or preventing it. It’s essential to understand their effects:
| Supplement | Effect on Clotting |
| Vitamin E | May prevent clotting due to its anticoagulant properties. |
| Ginkgo Biloba | Can thin blood and prevent clotting. |
| Garlic | May help prevent clot formation due to its antiplatelet activity. |
While natural remedies and supplements can be beneficial, it’s important to use them with traditional medical treatment. A healthcare provider should guide this integration. This ensures any interactions or adverse effects are managed well.
We recommend discussing the following with your healthcare provider:
By combining natural and conventional approaches, patients can benefit from a well-rounded treatment plan. This plan is tailored to their specific needs.
For those on long-term anticoagulation therapy, daily life is a balance. It involves medication, lifestyle, and staying alert. Managing this condition well means looking at all parts of patient care.
Sticking to anticoagulant medication is key for long-term therapy patients. Ways to stay on track include reminders, pill boxes, and refills on the same day each month. Knowing your medication and its effects is also important.
Doctors can help by giving clear instructions and regular check-ups. Teaching patients about their condition boosts their commitment to taking their medication.
Making lifestyle changes is important for managing long-term anticoagulation therapy. Eating a healthy diet with lots of fruits, veggies, and whole grains is advised. Avoid foods high in vitamin K, as they can affect your medication.
Staying active is good too, as it lowers blood clot risk. But, talk to your doctor before starting new exercises, like high-impact ones.
Having a medical ID card or alert device is crucial for anticoagulation therapy patients. It helps emergency doctors know your treatment.
Be ready for emergencies by having a plan. Know when to call for help and have emergency numbers handy.
Dealing with long-term anticoagulation therapy can be tough. Having support from groups, counseling, and educational materials helps a lot.
Doctors can connect you to these resources. This helps you better understand and manage your condition.
When patients on anticoagulation therapy need surgery or dental work, we must be careful. We need to avoid bleeding risks. Managing their anticoagulation therapy is key to keeping them safe.
We start by checking how much anticoagulation therapy the patient is on. Then, we decide how to adjust their medications for the procedure. This might mean stopping their anticoagulants or changing the dose to lower bleeding risks.
It’s important to assess the risks carefully. We look at the chance of blood clots and the risk of bleeding during the procedure.
| Procedure Type | Recommended Anticoagulation Management |
| Low-risk procedures (e.g., dental extractions) | Continue anticoagulation therapy with close monitoring |
| High-risk procedures (e.g., major surgery) | Temporarily discontinue anticoagulation therapy |
Bridging therapy uses short-acting anticoagulants like heparin. It’s for patients at high risk of blood clots. This is when they’re not taking their usual anticoagulant.
“The decision to use bridging therapy should be based on a careful assessment of the patient’s thromboembolic risk versus the risk of procedural bleeding.”
” Guidelines on Perioperative Anticoagulation
After the procedure, we watch for bleeding signs. We also restart anticoagulants when it’s safe. The timing depends on the procedure and the patient’s risk factors.
Good care also means teaching patients about bleeding signs. They should know what to do if they see unusual bleeding or bruising.
By managing anticoagulation therapy well before, during, and after procedures, we can reduce bleeding risks. This ensures the best outcomes for our patients.
We stress the importance of follow-up care and monitoring for blood clotting disorders. It ensures the treatment plan is effective. It also allows for timely adjustments if needed.
Regular blood tests are key in managing blood clotting disorders. These tests check if the treatment is working. They help avoid clotting and bleeding problems. The test frequency varies based on the medication and patient factors.
Technology has made home monitoring easier for patients with blood clotting disorders. Home devices offer convenience and can improve outcomes by allowing more frequent tests.
Benefits of home monitoring include:
It’s important to know the signs of successful treatment and complications for blood clot treatment. Success means preventing new clots and resolving existing ones without major bleeding.
Signs that treatment may not be working as intended include:
Treatment plans for blood clotting disorders need to be flexible. They often require changes based on health status, lifestyle, or medication side effects. Regular check-ups with healthcare providers are key to making these adjustments.
Factors that may necessitate treatment adjustments include:
Managing blood clotting disorders needs a full approach. This includes medical treatment, lifestyle changes, and regular checks. We’ve looked at different parts of blood clot treatment, from finding out you have one to stopping them from happening.
It’s a big job that needs doctors, nurses, and patients working together. Knowing the risks and signs of blood clots helps people avoid serious problems.
New research is bringing hope for better blood clot care. As we learn more, patients will get better results. This is good news for people all over the world.
With the help of doctors and staying up-to-date, people with blood clotting disorders can live well. We aim to give the support and info needed for the best care.
Symptoms include swelling, pain, or discoloration in the affected limb. You might also experience shortness of breath or chest pain. If clotting is too low, you could see easy bruising, prolonged bleeding, or frequent nosebleeds.
Doctors use blood tests to check clotting factors. They also do imaging studies to see clots. Sometimes, genetic testing is needed to find inherited disorders.
Treatment options include anticoagulant medications to stop new clots. There’s also thrombolytic therapy to dissolve clots. In severe cases, surgery might be needed.
Anticoagulants prevent new blood clots or stop them from growing. They work by blocking the body’s clotting process.
The main risk is bleeding, as these drugs stop the body from forming clots. Other risks include drug interactions and needing regular monitoring.
Yes, changes like regular exercise and a balanced diet can help. Staying hydrated and maintaining a healthy weight also support medical treatments.
Some natural remedies and supplements might affect clotting. But, it’s important to talk to a healthcare provider first. They can interact with medications.
Management during pregnancy includes safe medication options and close monitoring. This ensures the health of both mother and fetus.
Before surgery or dental procedures, planning is key. This might include bridging therapy. Post-procedure care is also important to reduce bleeding risks.
Regular testing and home monitoring are important. Recognizing signs of treatment success or failure helps manage the condition effectively.
While some risks can’t be changed, preventive strategies exist. These include risk assessment, preventive medications, and mechanical prevention methods, mainly during high-risk periods.
Support includes healthcare providers, patient education materials, and support groups. These are for patients on long-term anticoagulation therapy.
National Bleeding Disorders Foundation. (2004). Understanding current bleeding disorder treatments. https://www.bleeding.org/bleeding-disorders-a-z/treatment/current-treatments
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!