Last Updated on October 21, 2025 by mcelik
Leukemia is a cancer that affects the bone marrow. It causes the production of abnormal blood cells. It’s a condition that impacts thousands worldwide, with various classifications that are key for diagnosis and treatment.
Understanding the different classifications is very important. This includes acute myeloid leukemia and chronic lymphocytic leukemia. Understanding these classifications enables healthcare professionals to customize treatments according to each individual’s needs.
Blood cancer starts with changes in the bone marrow. It happens when the bone marrow makes too many abnormal white blood cells. These cells take over, causing health problems.
Blood cancer is when the bone marrow makes too many bad white blood cells. Leukemia is a type of blood cancer. It can affect different types of cells and grow at different rates.
These bad cells can stop the bone marrow from making healthy blood cells. This includes red blood cells, platelets, and good white blood cells.
We will explore how these changes happen and how they affect the body.
The bone marrow is inside some bones, like the hips and thighbones. It makes blood cells. In leukemia, it makes bad white blood cells instead.
These bad cells fill up the bone marrow. They stop it from making healthy blood cells.
| Cell Type | Normal Function | Abnormal Function in Leukemia |
| White Blood Cells | Fight infections | Don’t function properly, leading to infections |
| Red Blood Cells | Carry oxygen | Reduced production can lead to anemia |
| Platelets | Help blood clot | Reduced production can lead to bleeding issues |
Knowing how blood cancer starts is key to treating it. Doctors can then find the best ways to fight the disease.
Understanding the different types of leukemia is key to treating it. Leukemia is divided based on the type of cell affected and how fast it grows.
Leukemia is mainly split into acute and chronic types. Acute leukemia grows quickly, leading to fast health decline without treatment. Chronic leukemia grows slower, giving more time before symptoms worsen.
Determining whether the leukemia is acute or chronic is essential for deciding the appropriate treatment approach. Acute leukemia needs quick, strong treatment. Chronic leukemia might start with a “watch and wait” approach or milder treatments.
Another important split is by cell lineage: myeloid or lymphocytic. Myeloid leukemia affects cells that make red blood cells, platelets, and some white blood cells. Lymphocytic leukemia impacts lymphocytes, key for fighting off infections.
Knowing if it’s myeloid or lymphocytic helps doctors find the exact type and plan treatment. For example, AML and CML are myeloid, while ALL and CLL are lymphocytic.
| Leukemia Type | Cell Lineage | Disease Progression |
| Acute Myeloid Leukemia (AML) | Myeloid | Acute |
| Chronic Myeloid Leukemia (CML) | Myeloid | Chronic |
| Acute Lymphoblastic Leukemia (ALL) | Lymphocytic | Acute |
| Chronic Lymphocytic Leukemia (CLL) | Lymphocytic | Chronic |
Classifying leukemia into these groups is vital for treatment. Each type has its own signs, outlook, and treatment plans. For instance, the WBC count at diagnosis can greatly affect treatment choices.
Leukemia staging is unique and needs a different approach than solid tumors. Unlike solid tumors, which are staged by size and spread, leukemia is a blood and bone marrow cancer. This makes its staging more complex.
Leukemia staging is different because it involves the blood and bone marrow, not a specific tumor site. This means the TNM (Tumor, Node, Metastasis) system used for solid tumors doesn’t apply. Instead, leukemia staging looks at the type of leukemia and its impact on the body. It considers white blood cell counts and genetic abnormalities.
Key factors in leukemia staging include:
There are several ways to classify leukemia, showing its complexity and variability. The main types are Acute Myeloid Leukemia (AML), Acute Lymphoblastic Leukemia (ALL), Chronic Myeloid Leukemia (CML), and Chronic Lymphocytic Leukemia (CLL). Each has its own staging or classification criteria.
For instance, CLL is often staged using the Rai or Binet systems. These systems help determine prognosis and guide treatment. Knowing these classification methods is key for healthcare providers to create effective treatment plans.
Understanding leukemia’s staging systems and classification methods helps patients and healthcare providers. It aids in making informed decisions about treatment and care.
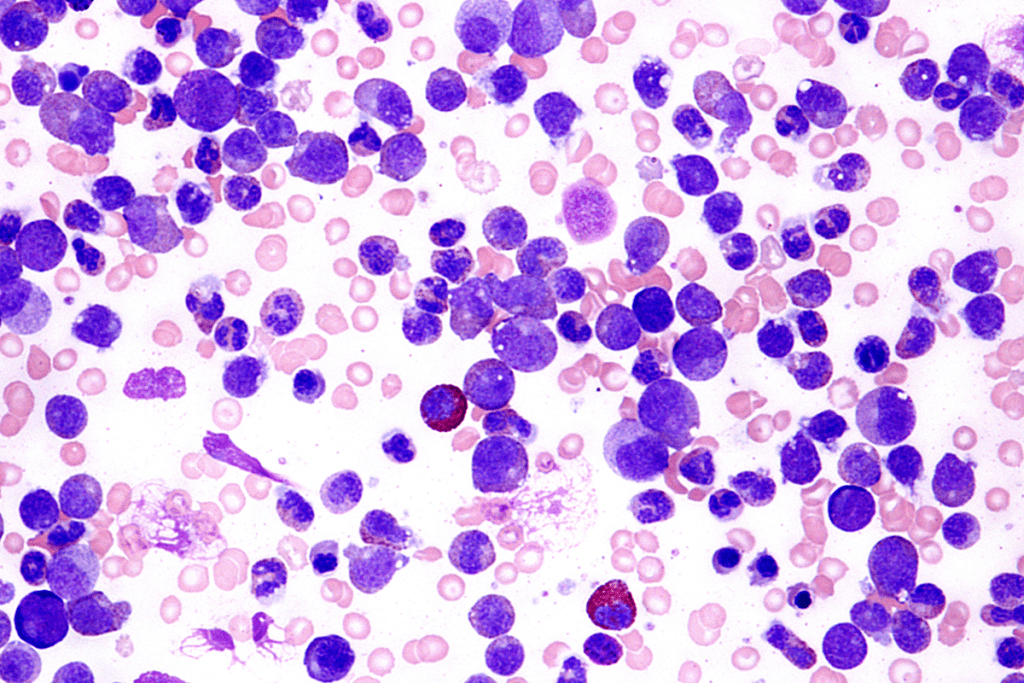
AML’s first stage shows early changes in cells. These changes are key to spotting and treating the disease. Acute Myeloid Leukemia is marked by fast-growing, abnormal cells in the bone marrow. These cells block the production of normal blood cells.
AML starts with genetic mutations in myeloid cells. This leads to their uncontrolled growth. As these cells build up, they push out normal cells in the bone marrow.
The bone marrow’s blast cell percentage is vital for AML diagnosis. A higher percentage means a more aggressive disease.
The World Health Organization (WHO) says AML is diagnosed when the bone marrow has 20% or more myeloid blasts. Catching it early is key for timely treatment.
| Blast Percentage | Diagnostic Implication |
| Less than 5% | Normal |
| 5-19% | Possible myelodysplastic syndrome |
| 20% or more | Determining whether the leukemia is acute or chronic is essential for deciding the appropriate treatment approach. |
Diagnosing AML requires blood tests, bone marrow biopsy, and genetic testing. Certain genetic abnormalities help confirm the diagnosis and guide treatment.
“The diagnosis of AML is based on the presence of at least 20% myeloblasts in the bone marrow or peripheral blood, along with evidence of myeloid lineage.”
Early diagnosis is vital for effective treatment. Treatments for AML include chemotherapy, targeted therapy, and sometimes bone marrow transplantation. The treatment choice depends on the patient’s health, the leukemia’s genetic traits, and the disease stage.
Understanding AML’s first stage is key for healthcare providers to plan effective treatment. Recognizing early signs and symptoms helps patients get medical help quickly. This improves their treatment chances.
Knowing about the first stage of Acute Lymphoblastic Leukemia (ALL) is key for early detection and treatment. ALL is marked by the quick growth of immature white blood cells, called lymphoblasts. These cells fill the bone marrow and stop it from making normal blood cells.
The start of ALL shows early cell problems. Genetic changes in lymphoid cells cause them to grow out of control. This leads to a buildup of lymphoblasts in the bone marrow.
This buildup can cause the bone marrow to fail. It then makes fewer normal blood cells, like red and white blood cells, and platelets.
Key characteristics of initial cellular abnormalities in ALL include:
ALL is more common in kids, but it can also hit adults. There are big differences in how often it happens, how well it’s treated, and how well it responds to treatment between kids and adults. Kids usually do better and have higher cure rates because they can handle stronger treatments.
The main differences between adult and childhood ALL include:
| Characteristics | Childhood ALL | Adult ALL |
| Incidence Peak | Between 2-5 years | Any age, increasing after 60 |
| Prognosis | Generally better, higher cure rates | Generally poorer, lower cure rates |
| Treatment Response | Better tolerance to intensive chemotherapy | Poorer tolerance, more treatment-resistant |
It’s important to know these differences. They help doctors create treatment plans that fit each patient’s needs.
CML starts with a special change in chromosomes 9 and 22, making the Philadelphia chromosome. This change is key to understanding and diagnosing CML.
In the chronic phase, patients might not feel sick at all. The disease makes more white blood cells, called granulocytes. It’s important to catch it early to treat it well.
We’ll look closer at this phase. We’ll talk about blood count changes and the Philadelphia chromosome.
The Philadelphia chromosome comes from a swap between chromosomes 9 and 22. This swap makes a BCR-ABL1 gene. This gene is key in CML’s growth.
Knowing about the Philadelphia chromosome is vital for diagnosing CML. It helps pick the best treatment.
To diagnose CML, doctors look for the Philadelphia chromosome. Finding it confirms the disease. It also helps track how the disease is doing.
| Characteristics | Chronic Phase CML |
| Symptoms | Mild or none |
| White Blood Cell Count | Elevated |
| Philadelphia Chromosome | Present |
CLL is often diagnosed early. Knowing how it starts is key to managing it well. CLL is a cancer that affects the blood and bone marrow. It makes too many immature white blood cells, called lymphocytes.
Staging CLL is important for knowing what to expect and how to treat it. The Rai and Binet systems are two main ways to stage CLL. Rai Stage 0 means the disease is just in the blood, with no other signs. Binet Stage A shows the disease is not widespread, with less than three areas affected.
These systems help doctors understand how far the disease has spread. Knowing this is vital for patients to understand their diagnosis and treatment plan.
| Staging System | Stage | Characteristics |
| Rai | 0 | High lymphocyte count in blood |
| Binet | A | Fewer than three areas of lymphoid involvement |
Many CLL patients are asymptomatic, meaning they don’t show symptoms. In these cases, treatment might not be needed right away. Instead, a watchful waiting or active surveillance approach is used. This involves regular checks through blood tests and physical exams.
Monitoring for asymptomatic CLL includes:
Early detection and monitoring help doctors act quickly. This can lead to better outcomes for CLL patients.
Abnormal blood counts can be an early sign of leukemia. They lead to more tests to check for the disease. A complete blood count (CBC) is key in finding these signs.
We’ll look at how leukemia changes blood counts. This includes white blood cell patterns and other CBC changes.
The white blood cell count (WBC) is important in the CBC. It changes in different leukemia types:
Other CBC changes can also happen early in leukemia:
These CBC changes may lead to more tests, like a bone marrow biopsy. They help confirm leukemia’s presence and type.
It’s important to spot the early signs of leukemia to get timely treatment. We’ll look at common warning signs for different leukemia types. We’ll also talk about subtle symptoms that are often missed.
Each type of leukemia shows different early symptoms. For example, Acute Myeloid Leukemia (AML) often causes fatigue, infections, and bleeding. On the other hand, Chronic Lymphocytic Leukemia (CLL) might not show symptoms early or might show swollen lymph nodes.
| Leukemia Type | Common Early Symptoms |
| Acute Myeloid Leukemia (AML) | Fatigue, infections, bleeding |
| Acute Lymphoblastic Leukemia (ALL) | Fever, fatigue, bone pain |
| Chronic Myeloid Leukemia (CML) | Fatigue, weight loss, abdominal fullness |
| Chronic Lymphocytic Leukemia (CLL) | Lymphadenopathy, fatigue, infections |
Some early leukemia symptoms are very subtle and can be mistaken for other things. For instance, slight weight loss, night sweats, or mild fever might hint at leukemia, if other symptoms are present.
“Early detection of leukemia requires a high index of suspicion, even for nonspecific symptoms.”
Knowing about these subtle symptoms can help in catching leukemia early. It’s key to see a doctor if you keep getting unusual or persistent symptoms.
Diagnosing leukemia early needs a detailed look at several key steps. We use a mix of first checks and advanced tests to find out if and what type of leukemia is present.
The first step is to do blood tests. These tests show the patient’s health and look for any blood cell count issues.
Blood Count Abnormalities: A complete blood count (CBC) is key. It spots odd white blood cell, red blood cell, and platelet counts. In leukemia, a CBC might show too many white blood cells, anemia, or low platelets.
| Blood Component | Normal Range | Abnormal Finding in Leukemia |
| White Blood Cells (WBC) | 4,500 – 11,000 cells/μL | Elevated or abnormal cells |
| Red Blood Cells (RBC) | 4.32 – 5.72 million cells/μL (varies by gender) | Anemia (low RBC count) |
| Platelets | 150,000 – 450,000 cells/μL | Thrombocytopenia (low platelet count) |
After blood tests, a bone marrow biopsy is done to confirm the diagnosis. This involves taking a bone marrow sample for examination.
Advanced Diagnostic Techniques: We also use advanced tests like flow cytometry, cytogenetic analysis, and molecular testing. These help us find out the leukemia’s specific traits. They guide us in choosing the right treatment.
By combining blood tests, bone marrow biopsy, and advanced diagnostics, we can accurately diagnose early-stage leukemia. This lets us create a treatment plan that fits the patient’s needs.
Knowing the best ways to treat the first stage of leukemia is key to better patient results. The treatment for the first stage of blood cancer can change a lot. It depends on the type of leukemia, the patient’s health, and other factors.
Each type of leukemia needs its own treatment plan. For example, Acute Myeloid Leukemia (AML) needs quick action because it’s aggressive. AML treatment often includes chemotherapy or targeted therapy, or both.
Chronic Lymphocytic Leukemia (CLL) might not need treatment right away if caught early. Instead, doctors might choose a “watch and wait” approach.
Acute Lymphoblastic Leukemia (ALL) treatment is usually intense chemotherapy. This works better in kids than adults. Chronic Myeloid Leukemia (CML) has seen big improvements thanks to targeted therapies that target the disease’s cause.
Some patients with early-stage CLL might get a “watch and wait” or “active surveillance” plan. This means watching the disease closely with blood tests and doctor visits, without starting treatment right away.
Choosing this approach depends on many things. These include the patient’s age, health, and the leukemia’s details. It’s picked when the risks of treatment are too high, or when the leukemia isn’t causing symptoms.
Being told you have leukemia can feel scary. But, with the right treatment, many people can live well with their condition. It’s important for patients to talk closely with their doctors to find the best treatment for them.
Leukemia’s prognosis and life expectancy depend on many factors. Each patient’s situation is unique. It’s important for both patients and doctors to understand these factors.
Several key factors impact early-stage leukemia survival rates. These include the leukemia type, the patient’s age, overall health, and how well the leukemia responds to treatment.
Age is a big factor. Older patients often face a tougher prognosis because of weaker health and other health problems.
The leukemia type also matters a lot. For example, acute leukemia needs quick treatment, while chronic leukemia progresses more slowly.
| Factor | Impact on Prognosis |
| Age | Older patients generally have a poorer prognosis |
| Leukemia Type | Acute leukemia requires immediate treatment; chronic leukemia progresses slower |
| Overall Health | Patients with other health issues may have a poorer prognosis |
| Response to Treatment | Patients who respond well to initial treatment have a better prognosis |
Leukemia prognosis varies by type. For instance, patients with Acute Lymphoblastic Leukemia (ALL) face different survival rates than those with Acute Myeloid Leukemia (AML).
It’s key to understand these differences. This helps manage expectations and make better treatment choices. We’ll keep looking into these differences and their impact on patient care.
Living with early-stage blood cancer means having a plan that covers medical care, emotional support, and lifestyle changes. It’s important to understand all parts of care to improve life quality.
Dealing with early-stage blood cancer is more than just treatment. It’s about taking care of your mind and heart too. Support groups are key, letting patients share and connect with others. Counseling services also offer emotional help, supporting patients and their families.
It’s also important to have the right information. Patients should talk to their doctors to make smart choices. Educational resources from trusted sources can help patients understand their situation better.
Making lifestyle adjustments is key when living with early-stage blood cancer. This includes eating right, staying active, and avoiding harmful things. A healthy diet helps your body during treatment.
Monitoring is also vital. Regular doctor visits help track the disease and adjust treatments. It’s important to notice any changes in your body and tell your doctor.
Being proactive in your care can help manage early-stage blood cancer better. This improves your overall health and well-being.
Understanding leukemia is key for early detection and effective treatment. Leukemia is a blood cancer with different types, like AML, ALL, CML, and CLL. Each type needs a specific approach for diagnosis and treatment.
Early detection is vital for better treatment results. Thanks to blood tests and bone marrow biopsies, doctors can catch leukemia early. This has led to new treatment options, from targeted therapies to watchful waiting, based on the disease’s type and stage.
In summary, knowing about blood cancer and its types is critical. Patients and doctors need to stay informed about diagnosis and treatment. This knowledge helps guide care and improves health outcomes.
Leukemia includes Acute Myeloid Leukemia (AML), Acute Lymphoblastic Leukemia (ALL), and Chronic Myeloid Leukemia (CML). It also includes Chronic Lymphocytic Leukemia (CLL).
Staging leukemia is different from solid tumors. It uses specific systems for each type, like Rai and Binet for CLL.
Early signs are fatigue, weight loss, and frequent infections. You might also notice easy bruising and pale skin.
First, blood tests are done. Then, a bone marrow biopsy is taken. These help find abnormal cells and the leukemia type.
Treatment depends on the leukemia type. It might be chemotherapy, targeted therapy, or watching and waiting, like for CLL.
Leukemia changes white blood cell counts. It also affects red blood cells and platelets. A CBC test can show these changes.
Prognosis varies by leukemia type and individual factors. Genetic abnormalities and treatment response play a big role.
Cure chances depend on leukemia type and early diagnosis. Some types, like ALL, have a high cure rate if treated quickly.
Blood transfusion needs vary by leukemia type, disease stage, and treatment.
Patients should eat healthy, avoid infections, and manage stress. Regular monitoring and follow-up care are also key.
Yes, there are many resources. These include counseling, support groups, and educational materials to help patients cope.
Wang, Y., et al. (2025). Statistical analysis of incidence, mortality, and disease burden of leukemia. Frontiers in Public Health, 13, 1560003.
https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1560003/full
Lee, S., & Kumar, R. (2024). Understanding the first stage of acute myeloid leukemia (AML): Molecular markers and diagnostic criteria. Blood Reviews.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!