Last Updated on October 21, 2025 by mcelik
Impaired coagulation affects millions worldwide, leading to health issues. These include bleeding disorders and clotting disorders. Coagulation helps stop bleeding after injuries. But, when it’s disrupted, it can cause too much bleeding or unwanted clots.
A coagulation disease of blood can appear in many forms, depending on how the body’s clotting process is affected. Coagulopathy, a condition of impaired coagulation, shows in different ways. You might notice easy bruising, bleeding that won’t stop after cuts, or frequent nosebleeds. Knowing these signs is key for early diagnosis and treatment.
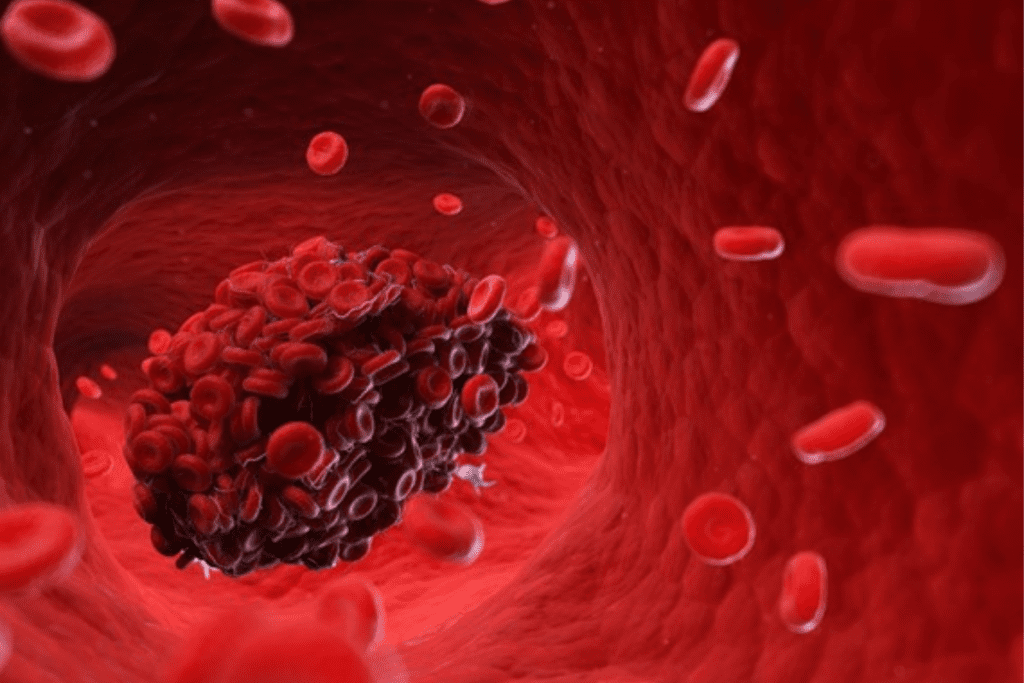
Blood coagulation is vital for stopping bleeding when a blood vessel is hurt. It involves many parts working together to make a clot. This clot is key for keeping blood inside our bodies.
When a blood vessel is damaged, the coagulation process starts. This damage exposes tissue under the blood vessel’s lining. It sets off a chain of chemical reactions. These reactions use clotting factors to create a fibrin clot.
The coagulation process has three main stages: starting, amplifying, and forming a fibrin clot. Knowing about these stages helps us understand how problems with coagulation can happen.
Platelets and clotting factors are key in coagulation. Platelets gather at the injury site. Clotting factors then work together in a cascade to form a stable clot.
Problems with these components can lead to too much bleeding or clotting. This is what happens in coagulation disorders.
Coagulation disorders affect how blood clots, leading to too much bleeding or clotting. These issues can be passed down or caused by other factors. They greatly impact a person’s life quality.
Coagulation disorders mess with blood clotting. They fall into two main groups: bleeding and thrombotic disorders. Bleeding disorders, like hemophilia, make bleeding more likely. Thrombotic disorders, such as deep vein thrombosis, make clotting more likely.
| Disorder Type | Description | Examples |
| Bleeding Disorders | Conditions that lead to excessive bleeding | Hemophilia, Von Willebrand Disease |
| Thrombotic Disorders | Conditions that lead to excessive clotting | Deep Vein Thrombosis, Pulmonary Embolism |
Coagulation disorders are common worldwide. The number of people affected varies by condition. For example, hemophilia affects about 1 in 5,000 males globally. Deep vein thrombosis affects around 1 in 1,000 people yearly.
Many factors can lead to coagulation disorders. These include genetics, age, and certain health conditions. Knowing these risk factors helps in early diagnosis and treatment.
Bleeding disorders make it hard for blood to clot, leading to long or sudden bleeding. These issues can really impact someone’s life, causing lots of bruises and long bleeding after injuries or surgeries.
Hemophilia is a genetic issue that stops the body from making blood clots. This is needed to stop bleeding. It’s caused by a lack of either factor VIII (Hemophilia A) or factor IX (Hemophilia B). Symptoms include long bleeding after injuries, bleeding into joints or muscles, and easy bruising.
For example, a child with hemophilia might get frequent joint bleeds. This can cause chronic pain and make it hard to move if not treated right. Treatment usually involves replacing the missing clotting factor.
Von Willebrand disease is a bleeding disorder caused by a lack or problem with von Willebrand factor. This protein is key for blood clotting. Symptoms can be mild or severe, including heavy menstrual bleeding, nosebleeds, and easy bruising.
Someone with von Willebrand disease might bleed a lot after dental work or surgeries. This shows the need for careful management and possibly treatments before these procedures.
Platelet function disorders happen when platelets don’t work right, making it hard to clot blood. These can be inherited or get worse over time. Symptoms include easy bruising, long bleeding after injuries, and small spots on the skin from bleeding.
For instance, people with Glanzmann’s thrombasthenia, a rare platelet disorder, might have severe bleeding. They need special treatments to help their platelets work better or manage bleeding.
It’s key for healthcare providers to know about these bleeding disorders. By spotting signs like easy bruising, long bleeding, and sudden bleeding, they can give the right care. This helps improve life for those with these conditions.
It’s key to know about clotting disorders like thrombophilia and DIC to manage them well. These disorders happen when blood clotting goes wrong, causing too much clotting or bleeding. We’ll look at the main types, their causes, signs, and possible problems.
Thrombophilia means your blood clots too much. It can be due to genes, other conditions, or both. Genetic thrombophilia often comes from gene changes, like in Factor V Leiden or the prothrombin gene.
Other types of thrombophilia can come from being inactive for too long, having cancer, or taking certain medicines. Symptoms include frequent DVT or PE.
DIC is a serious issue where both clotting and bleeding happen. It starts when the body’s clotting system goes off everywhere, making lots of small clots. This uses up all the clotting factors, which can lead to serious bleeding.
DIC can be caused by many things, like severe infections, trauma, cancer, or pregnancy problems. Symptoms can be mild or severe, showing both clotting and bleeding signs, like bruises or even organ failure.
Antiphospholipid syndrome (APS) is an autoimmune disease that makes clotting more likely. It’s marked by antiphospholipid antibodies, causing clots in veins and arteries. APS can also harm pregnancies, leading to miscarriage or death of the baby.
APS symptoms vary a lot. Some people get clots often, while others might have other signs like skin changes or brain problems. Treatment usually involves medicines to stop clots from forming.
In summary, clotting disorders like thrombophilia, DIC, and APS are serious health threats. Knowing their causes, symptoms, and risks is vital for managing them. Quick medical help is key to avoiding serious heart problems.
The signs of impaired coagulation can be hard to spot at first. But catching them early is key to managing them well. We’ll cover the common symptoms of coagulation disorders. This will help you know when to get medical help.
Spotting coagulation disorder symptoms early can lead to quick medical help. Some early signs include:
These signs might mean there’s a coagulation problem. It’s important to see a doctor if you notice any of these.
As coagulation disorders get worse, symptoms can get more serious. Signs of worsening include:
Spotting these signs is key to avoiding big problems. If you or someone you know has these symptoms, get medical help right away.
Knowing the symptoms of impaired coagulation helps you take care of your health. Being aware of early signs and severity indicators lets you get medical help fast. This can stop serious problems before they start.
It’s key to know the symptoms of bleeding disorders early. These conditions affect how blood clots, causing too much bleeding. We’ll look at common symptoms and what patients face.
Easy bruising is a big sign of bleeding disorders. Even small bumps can cause big bruises. These can hurt and look bad.
Prolonged bleeding after injuries or surgery is also common. For example, someone with a bleeding disorder might bleed a lot after a tooth extraction or surgery.
Real-life Example: A young girl got a bleeding disorder after a minor cut caused severe bleeding. She needed quick medical help and treatment.
Some disorders cause bleeding without any reason or injury. This can be scary and may hurt a lot. It can also make joints or muscles swell.
Spontaneous bleeding can really affect someone’s life. It can happen anytime and might need fast medical help.
Some bleeding disorders, like hemophilia, can cause bleeding in joints and muscles. This can lead to long-term pain, swelling, and trouble moving. Muscle bleeding can also hurt a lot and may cause serious problems if not treated right.
Early diagnosis and right treatment are vital for bleeding disorders. They help avoid long-term problems and improve life quality. Knowing the symptoms helps doctors give better care and support.
Excessive clotting disorders can cause serious health problems. These include deep vein thrombosis, pulmonary embolism, and arterial thrombosis. It’s important to know the symptoms to get medical help quickly.
Deep vein thrombosis happens when a blood clot forms in a deep vein, usually in the legs. You might notice swelling, pain, or tenderness.
Pulmonary embolism is a serious condition. It happens when a blood clot travels to the lungs. Look out for sudden shortness of breath, chest pain, and coughing up blood.
Arterial thrombosis is when a blood clot forms in an artery. This can lead to a heart attack or stroke. You might feel severe chest pain, numbness, or weakness in your face or limbs.
Coagulation disorders can affect different parts of the body. They can impact various organs and systems. It’s important to know how they affect each part.
Gastrointestinal symptoms of coagulation disorders can be hard to spot. Patients might have:
These signs can come from bleeding or clotting disorders. A detailed check-up is key.
| Symptom | Bleeding Disorders | Clotting Disorders |
| Gastrointestinal Bleeding | Common in hemophilia and other bleeding disorders | Less common, but can occur in conditions like mesenteric vein thrombosis |
| Abdominal Pain | Can result from bleeding into the intestinal wall or peritoneum | May be caused by ischemia due to thrombosis |
Coagulation disorders can deeply affect the brain and nervous system. Symptoms may include:
Coagulation disorders can also show up in the kidneys and urinary system. Signs include:
Knowing these signs is key to diagnosing and treating coagulation disorders.
By spotting these symptoms, doctors can act fast. This helps patients get better sooner.
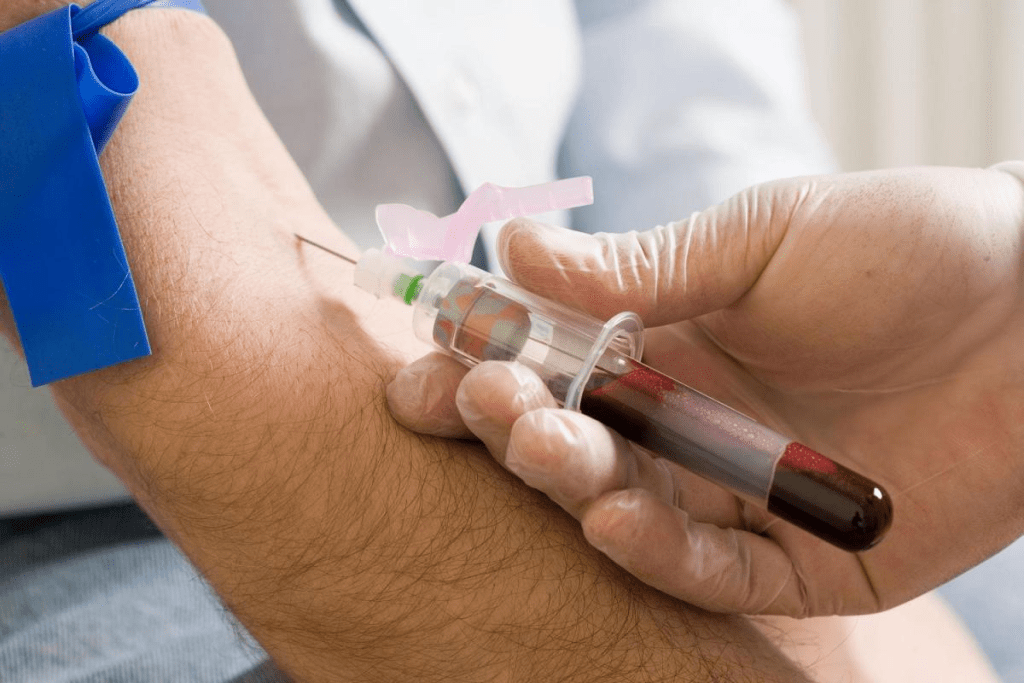
Diagnosing coagulation disorders needs a detailed approach. We use many tests and studies to understand blood clotting. This helps us find any disorders.
Laboratory tests are key in finding bleeding disorders. Some important tests are:
For clotting disorders, we use different tests. These include:
Imaging studies are also vital for diagnosing coagulation disorders. They help spot thrombi or emboli. Common imaging methods are:
By mixing lab tests with imaging, we can accurately find coagulation disorders. Then, we can plan effective treatments.
Ignoring coagulation disorders can lead to serious complications. These can greatly affect your quality of life. Untreated, these conditions can cause long-term health problems, impacting many areas of your wellbeing.
Bleeding disorders, if untreated, can cause chronic health issues. For example, people with hemophilia may have joint bleeding over and over. This can lead to chronic joint disease and disability. Severe bleeding episodes can even be life-threatening if not treated quickly.
Some long-term effects include:
Thrombotic disorders, like deep vein thrombosis (DVT) and pulmonary embolism (PE), can be severe. If not treated, they can be life-threatening. Some complications include:
| Complication | Description |
| Pulmonary Embolism | A blockage of an artery in the lungs that can be fatal |
| Post-Thrombotic Syndrome | Chronic pain, swelling, and skin discoloration in the affected limb |
| Recurrent DVT | Repeated episodes of deep vein thrombosis, increasing the risk of complications |
Bleeding and thrombotic disorders can greatly affect your quality of life. The fear of bleeding or clotting episodes can cause anxiety and depression. This can limit your daily activities and social interactions.
Key impacts include:
Understanding the complications of untreated coagulation disorders is key. Seeking timely medical intervention can improve your quality of life. It can also reduce the risk of long-term health consequences.
Treating bleeding disorders requires a mix of methods to stop and prevent bleeding. Each person’s treatment plan is unique, based on their specific condition and needs.
Replacement therapy is key for some bleeding disorders, like hemophilia. It involves adding missing clotting factors to the blood. For example, people with hemophilia A get Factor VIII, and those with hemophilia B get Factor IX. These can come from human plasma or be made in a lab.
| Clotting Factor | Condition Treated | Source of Concentrate |
| Factor VIII | Hemophilia A | Human plasma or recombinant |
| Factor IX | Hemophilia B | Human plasma or recombinant |
The World Federation of Hemophilia says, “Replacement therapy has changed hemophilia treatment, making life better for patients.” Regular treatment can stop bleeding and protect joints from damage.
Medicines can also help with bleeding disorders. Antifibrinolytic agents, like tranexamic acid, keep clots stable. They’re good for stopping bleeding in the nose or after dental work.
Key Medications:
Surgery might be needed for bleeding disorder complications or uncontrolled bleeding. Surgeries can be simple, like dental extractions, or complex, like joint replacements.
For severe joint damage, surgery can help a lot. It can reduce pain and improve movement, making life better.
Living with a bleeding disorder is tough, but the right treatment can make a big difference. Our healthcare team creates personalized plans to meet each patient’s needs.
Clotting disorders need a detailed treatment plan to manage and prevent problems. The main goal is to stop harmful clots from forming and lower the risk of blood clots.
Anticoagulant medications are key in treating clotting disorders. They stop the body from making clotting factors or prevent blood clots from forming. Common ones include warfarin, rivaroxaban, and apixaban.
Anticoagulant medications help stop new clots from forming and prevent existing ones from growing. They are often given to people who have had deep vein thrombosis (DVT) or pulmonary embolism (PE).
Thrombolytic therapy is used in urgent situations to break up clots that have already formed. It’s mainly for serious conditions like acute ischemic stroke or severe pulmonary embolism.
| Treatment Approach | Description | Example |
| Anticoagulant Medications | Prevents the formation of new clots and stops existing clots from getting bigger | Warfarin, Rivaroxaban |
| Thrombolytic Therapy | Dissolves clots that have already formed | Alteplase |
Living with coagulation disorders means managing daily life carefully. It involves strategies, lifestyle choices, and nutrition. We’re here to help you understand and manage these challenges.
Managing your condition every day is key. This includes:
By focusing on these tasks, you can control your condition better. This helps avoid serious problems.
Staying active is good for your health. But, people with coagulation disorders must be careful. We suggest:
Eating right is important for managing your condition. Focus on:
| Nutrient | Importance | Food Sources |
| Vitamin K | Crucial for blood clotting | Leafy greens, fish, and meat |
| Iron | Essential for healthy red blood cells | Red meat, beans, and fortified cereals |
| Omega-3 Fatty Acids | Helps reduce inflammation | Fatty fish, nuts, and seeds |
Keeping your diet balanced and drinking plenty of water is key. It helps manage your condition well.
Knowing when to get medical help can save lives. Coagulation disorders can cause serious problems if not treated quickly.
Some symptoms mean you need to see a doctor right away. These include:
Immediate action is required if you have any of these symptoms. A medical expert once said,
“Prompt recognition and treatment of emergency warning signs can significantly reduce morbidity and mortality in patients with coagulation disorders.”
Some symptoms are not life-threatening but need urgent medical help. These include:
We suggest getting medical care within 24 hours if you notice these symptoms.
After treatment, regular check-ups are key for managing coagulation disorders. This includes:
Effective follow-up care can significantly improve your quality of life. By following these guidelines, you can manage your condition better and lower the risk of complications.
Coagulation disorders are complex and can be life-threatening. We’ve looked at different types, like hemophilia and von Willebrand disease. We also talked about clotting disorders such as thrombophilia and antiphospholipid syndrome.
It’s important to understand symptoms, diagnosis, and treatment for these conditions. This knowledge helps manage them effectively.
Knowing about coagulation disease of blood can greatly improve life for those affected. Spotting early signs and getting medical help quickly is key. This can prevent serious problems and ensure the right care is given.
In short, managing coagulation disorders needs a team effort. This includes medical treatment, lifestyle changes, and regular check-ups. A team approach is vital to help patients with bleeding or clotting disorders live well.
Coagulopathy is a condition that makes blood clotting hard. This can cause too much bleeding or clotting. Symptoms include easy bruising and dangerous blood clots.
Bleeding disorders can cause easy bruising and long bleeding after injuries. They can also lead to spontaneous bleeding and joint pain. These symptoms need quick medical help.
Excessive clotting disorders show as deep vein thrombosis, pulmonary embolism, and arterial thrombosis. These are serious and need immediate care.
Doctors use tests like clotting time tests and platelet count to diagnose. They also use imaging to find blood clots.
Treatments include replacing clotting factors and using medications. Sometimes, surgery is needed to fix complications.
Treatment for clotting disorders includes anticoagulant medications. They also use thrombolytic therapy and lifestyle changes to prevent clots.
Yes, with the right treatment and lifestyle changes, many manage their condition well. Regular monitoring is key.
Untreated disorders can cause chronic pain and disability. They also increase the risk of serious clots. Effective management is vital.
Seek medical help right away for severe bleeding or signs of clots. Early treatment is critical.
Yes, making dietary changes and avoiding certain medications can help. Also, staying active is important.
These disorders can affect various organs and systems. Symptoms vary based on whether it’s bleeding or clotting issues.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!