Last Updated on October 21, 2025 by mcelik
Sickle Cell Disease: Understanding Causes and Treatment
Sickle cell disease affects millions worldwide, causing health issues like anemia and pain crises. In the United States, it’s estimated that sickle cell disease affects approximately 100,000 people, greatly impacting their quality of life.
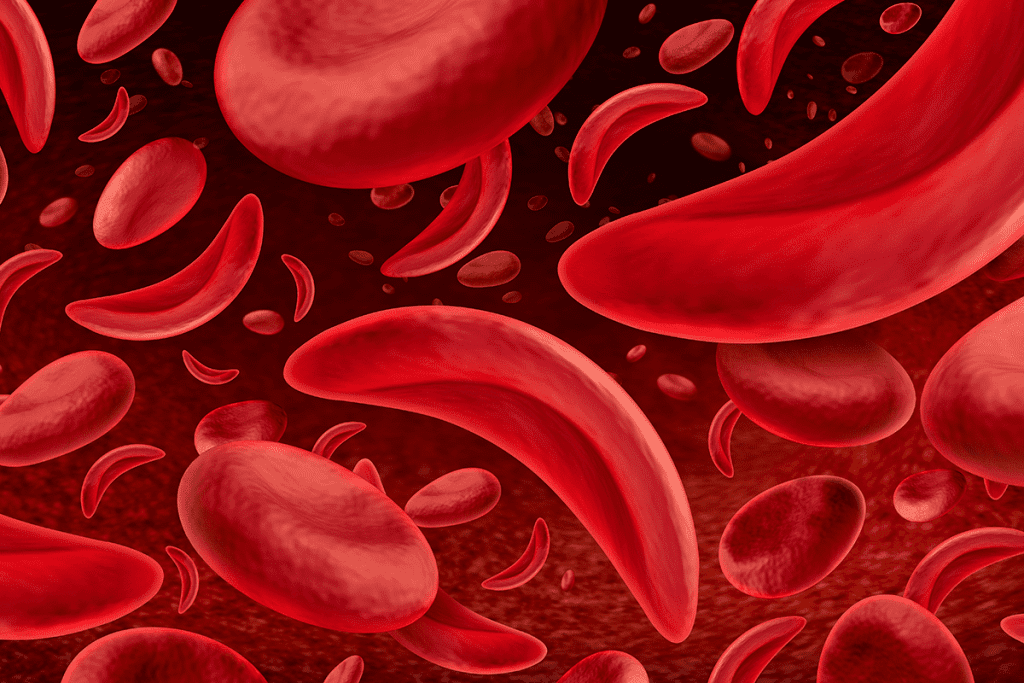
The condition is caused by abnormal hemoglobin production, which leads to distorted red blood cells. These can cause severe pain, organ damage, and other complications. Understanding this condition is key to developing effective sickle cell anemia treatment strategies that improve patients’ quality of life and long-term health outcomes.
It’s important to understand sickle cell disease to create good treatment plans. This group of genetic disorders affects how the body makes hemoglobin. It leads to health problems. “Sickle cell disease is a complex condition that requires a full management plan,” say doctors.
Sickle cell disease happens when the body makes abnormal hemoglobin, called sickle hemoglobin or hemoglobin S. This makes red blood cells bend into a sickle shape. They then break down early, causing health issues. The most common type is sickle cell anemia (HbSS). Other types include HbSC disease and HbS/β-thalassemia.
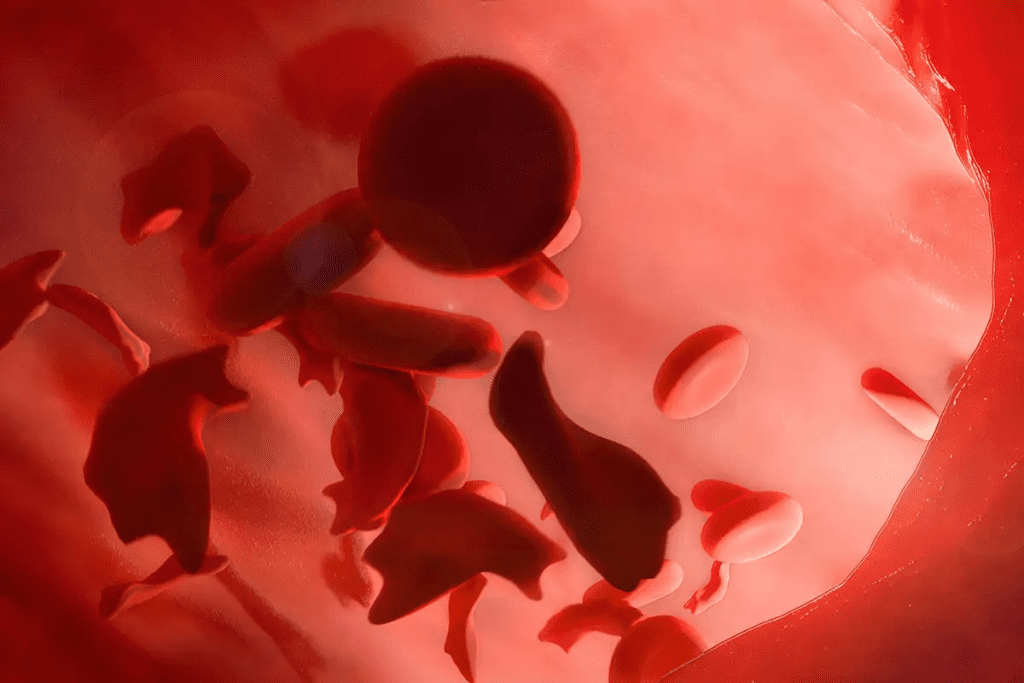
When red blood cells bend, they can block blood flow in small vessels. This leads to pain, organ damage, and serious health problems. Sickle cell disease affects many parts of the body. It can cause chronic issues like infections, stroke, and heart disease.
Sickle cell disease is not just one condition. It’s a range of disorders. The main types are:
A recent study found the Sickle Cell Disease market in the 6 major markets was worth about USD 650 million in 2023. This shows the big economic impact of this condition.
Sickle cell disease is caused by a mutation in the HBB gene. This gene codes for a part of hemoglobin. The mutation leads to abnormal hemoglobin, known as sickle hemoglobin or hemoglobin S.
The disease follows an autosomal recessive pattern of inheritance. This means a person needs two mutated HBB genes, one from each parent, to have the disease.
Understanding the inheritance pattern of sickle cell disease is key. When both parents carry the mutated gene, there’s a 25% chance their child will have the disease.
The mutation causing sickle cell disease is a point mutation in the HBB gene. It changes glutamic acid to valine at the sixth position of the β-globin chain. This leads to sickle hemoglobin production.
| Genetic Mutation | Effect on Hemoglobin | Result |
| Point mutation in HBB gene | Substitution of glutamic acid with valine | Production of sickle hemoglobin |
| Two mutated genes | Expression of sickle cell disease | Sickle cell disease manifestation |
It’s important to know the difference between sickle cell trait and sickle cell disease. People with sickle cell trait have one normal and one mutated HBB gene. They are carriers and usually don’t show symptoms but can pass the mutated gene to their children.
Carriers of the sickle cell trait are generally healthy but can pass the mutated gene to their children. Knowing someone’s genetic status is important for family planning and genetic counseling.
Sickle Cell Anemia Treatment: Key Steps to Manage the Condition
People with sickle cell anemia face many serious health challenges, including severe pain and long-term complications. This condition causes red blood cells to form a sickle shape, which blocks blood flow and reduces oxygen delivery to organs.
Sickle cell anemia treatment focuses on managing symptoms, preventing crises, and improving quality of life. Treatments may include medications like hydroxyurea, blood transfusions, and in some cases, bone marrow transplants. With proper medical care and regular monitoring, people with sickle cell anemia can lead healthier, more stable lives.
Acute pain crises, or sickle cell crises, happen when sickled red blood cells block blood vessels. This blockage causes tissue ischemia and severe pain. It’s the most common symptom for patients.
Triggers for Acute Pain Crises:
Chronic problems from sickle cell anemia include anemia, more infections, and organ damage. Anemia comes from red blood cells living shorter lives, causing fatigue and other issues.
The table below lists some chronic complications of sickle cell anemia:
| Complication | Description |
| Anemia | Reduced red blood cell count leading to fatigue |
| Increased Infection Risk | Damage to the spleen increases susceptibility to infections |
| Organ Damage | Sickling can cause damage to organs like the kidneys and heart |
Sickle cell anemia can harm many organs and systems. The spleen is often damaged because of sickling. Other organs, like the kidneys and heart, can also suffer, leading to long-term health problems.
Regular monitoring and management are key to lessen the harm on organs and systems.
Managing sickle cell anemia involves many treatments. Each one is chosen based on the patient’s needs. The main goal is to control symptoms, prevent problems, and improve life quality.
Pain control is key in treating sickle cell anemia. Nonsteroidal anti-inflammatory drugs (NSAIDs) help with mild to moderate pain. For severe pain, opioids might be used during crises.
It’s also important to find and avoid pain triggers. Using methods like staying hydrated and relaxing can help too.
Hydroxyurea is a treatment that changes the disease’s course. It reduces pain crises and blood transfusion needs. It works by making more fetal hemoglobin, which stops red blood cells from sickling.
It’s vital to watch for side effects closely.
Blood transfusions lower the risk of serious problems by reducing sickling red blood cells. They’re used for those at high stroke risk or with severe complications. But, they can cause iron buildup, needing chelating agents to manage it.
In summary, treating sickle cell anemia needs a mix of pain management, hydroxyurea, and blood transfusions. Tailoring treatment to each patient improves their life quality and outcomes.
Treatment for sickle cell disease has made big strides with new FDA-approved meds. These drugs aim to cut down on pain crises, boost hemoglobin levels, and improve life quality for those affected.
Hydroxyurea is a key drug for sickle cell disease. It lowers the number of pain crises and blood transfusions needed. It does this by increasing fetal hemoglobin, which stops red blood cells from sickling.
Benefits of Hydroxyurea:
L-glutamine, known as Endari, is an oral drug. It cuts down on pain crises in sickle cell disease patients. It’s thought to work by reducing body stress.
Crizanlizumab, or Adakveo, is a monoclonal antibody. It targets P-selectin, a protein that makes sickled red blood cells stick to blood vessels. By blocking P-selectin, it lowers vaso-occlusive crises.
Voxelotor, or Oxbryta, boosts hemoglobin levels. It does this by stopping hemoglobin S polymerization. This means better oxygen delivery to tissues, reducing anemia severity.
New treatments like CASGEVY (exa-cel) and LYFGENIA (lovo-cel) are big steps forward. These gene-editing therapies are changing how we manage sickle cell disease.
| Medication | Mechanism of Action | Benefits |
| Hydroxyurea (Droxia, Siklos) | Increases fetal hemoglobin production | Reduces pain crises, decreases need for blood transfusions |
| L-glutamine (Endari) | Reduces oxidative stress | Reduces frequency of pain crises |
| Crizanlizumab (Adakveo) | Inhibits P-selectin | Reduces frequency of vaso-occlusive crises |
| Voxelotor (Oxbryta) | Inhibits hemoglobin S polymerization | Increases hemoglobin levels, improves oxygen delivery |
Bone marrow transplantation is currently the only widely recognized curative treatment for sickle cell disease. It replaces the patient’s bone marrow with healthy donor cells. Recent surveys show it’s a promising way to fix the genetic defect causing the disease.
The process replaces the patient’s bone marrow with healthy donor cells. This is a complex procedure that needs careful thought. It depends on the patient’s health and finding a compatible donor. It can cure sickle cell disease by removing the genetic defect.
“Bone marrow transplantation is a game-changer for patients with sickle cell disease,” say medical experts. It offers a chance at a normal life without the disease’s complications.
Finding a compatible donor is a big challenge. The transplant’s success depends on the genetic match between donor and recipient. Family members are often first choices, but unrelated donors may be needed. Finding a donor takes time and involves genetic testing.
While bone marrow transplantation offers a cure, it comes with risks. Complications like graft-versus-host disease (GVHD) can happen. The success rate varies, and patients must be evaluated to see if they’re a good match for the procedure.
| Success Factors | Risks |
| Genetic match between donor and recipient | Graft-versus-host disease (GVHD) |
| Patient’s overall health | Infection and other complications |
Choosing bone marrow transplantation is a big decision. It needs careful thought about the benefits and risks. For many with sickle cell disease, it’s a chance to improve their life quality.
To find out if there’s a cure for sickle cell anemia, we need to look at the latest research and treatments. A cure means fixing the genetic problem that causes the disease. This would make normal hemoglobin and get rid of symptoms.
A cure for sickle cell disease means fixing the genetic cause. This stops sickled red blood cells from being made. Treatments that change or lessen the genetic mutation are key.
Current understanding shows a cure is more than just treating symptoms. It changes the disease’s cause. Gene therapy and gene editing are new ways to treat SCD, showing promise.
“Gene therapy and gene editing are emerging as potentially curative approaches for SCD,” recent insights from DelveInsight reveal.
There are several ways to cure sickle cell disease:
These treatments are in different stages of development. Bone marrow transplantation is the most known, but it’s limited by donor availability and other issues.
Getting access to SCD treatments is hard because of:
There are efforts to make these treatments more available. This includes finding new donors and making treatments cheaper.
Gene therapy is a new way to treat sickle cell anemia. It changes or replaces the bad HBB gene that causes the disease. This method involves editing a patient’s stem cells outside the body and then putting them back in.
Many gene therapy products are being tested in clinical trials. One example is CTX001, a CRISPR/Cas9 gene-edited therapy. These treatments aim to fix the genetic problem that leads to sickle cell disease, helping hemoglobin production return to normal.
Key approaches include:
Clinical trials have shown great promise for gene therapy in sickle cell disease. Some patients have seen their hemoglobin levels return to normal and have fewer symptoms. For example, CTX001 trials have shown that CRISPR/Cas9 gene editing can cure sickle cell disease.
Notable results include:
Despite the encouraging results, gene therapy for sickle cell disease has its hurdles. These include:
Overcoming these challenges is key to making gene therapy a common treatment for sickle cell disease.
CRISPR gene editing is a new hope for sickle cell disease. It could be a cure. This tech makes precise changes to the genome, fixing the disease’s cause.
The CRISPR/Cas9 system finds and fixes the HBB gene. This gene makes a part of hemoglobin. By fixing it in stem cells, CRISPR aims to cure sickle cell disease.
Studies show CRISPR can precisely fix the SCD genetic defect. This is a big step forward.
Many trials are testing CRISPR for SCD. They use autologous hematopoietic stem cell transplantation. This means using a patient’s own edited stem cells.
First results are good, showing safety and efficacy. But, more research is needed to fully understand CRISPR’s benefits and challenges.
The future of CRISPR for SCD is bright. Gene editing is getting better. We’ll see safer, more effective, and accessible treatments soon.
CRISPR’s success in SCD might lead to new treatments for other genetic diseases. This could change gene therapy forever.
The treatment for sickle cell disease is changing fast. New breakthroughs and FDA approvals are leading this change. These advances come from gene editing and new ways to treat the disease.
New treatments for sickle cell disease have emerged, including gene-editing therapies. CRISPR-Cas9 gene editing is one of the most promising. It has shown great promise in clinical trials, possibly curing the disease.
“The advent of gene editing represents a paradigm shift in the treatment of genetic diseases like SCD,” leading researchers say.
The FDA has approved new SCD treatments like CASGEVY (exa-cel) and LYFGENIA (lovo-cel). These approvals are big steps forward. They give patients and doctors new options.
While these new treatments are promising, access is a big issue. It’s important that patients can get these therapies to improve their health. We need to work on insurance, cost, and availability.
These breakthrough treatments have a big impact on patients. They can reduce pain crises and possibly cure the disease. Studies will help us understand the long-term effects.
Managing sickle cell disease means taking many steps to prevent problems and ease symptoms. It’s about using preventive actions, making lifestyle changes, and getting quick medical help.
Stopping pain crises is key in managing sickle cell disease. This can be done with medicine, lifestyle changes, and avoiding certain things. Hydroxyurea is a medicine that helps lower the number of pain crises.
Drinking enough water and eating well are very important for sickle cell disease patients. Drinking lots of water and eating a balanced diet helps prevent dehydration and lowers the risk of serious problems.
Hydration is very important because dehydration can cause pain crises. Patients should drink at least eight glasses of water a day.
Staying away from things that can trigger sickle cell disease is also important. Things like extreme temperatures, high altitudes, and stress can be triggers. Patients should know what triggers them and try to avoid them.
Even with prevention, pain crises can happen. It’s important for patients to know when to go to the emergency room. Signs that mean you need to go right away include very bad pain, trouble breathing, and a fever over 101.5 °F.
By following these steps, patients with sickle cell disease can manage their symptoms better. They can also reduce pain crises and improve their life quality.
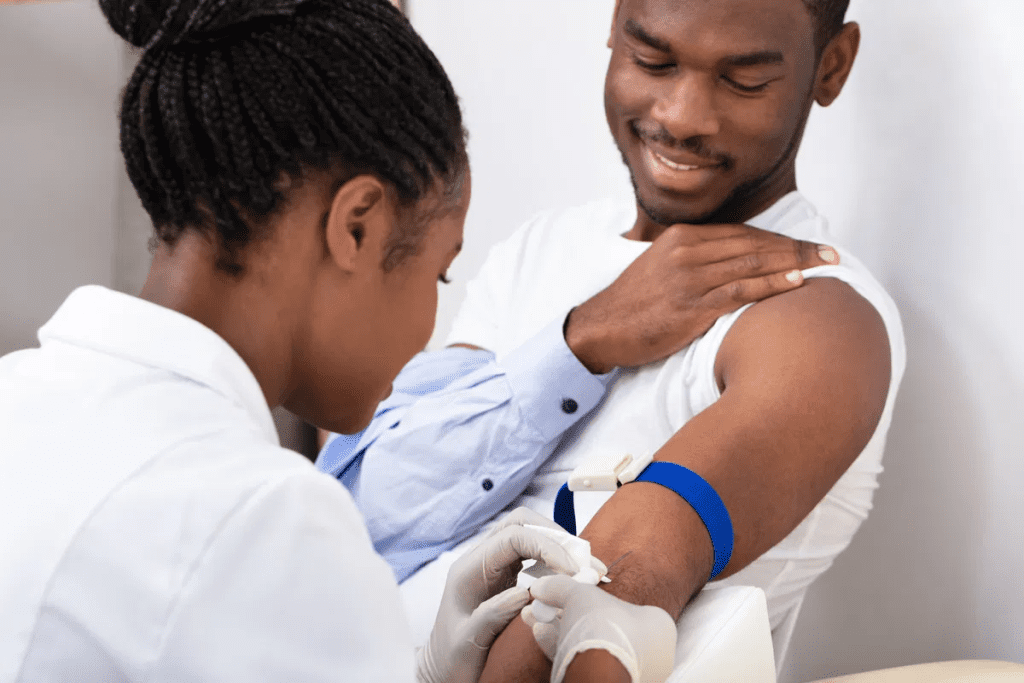
Getting the right care is key for SCD patients to live better lives. It’s about managing the disease’s tough side effects. A team effort is needed to meet all the patient’s needs.
A team of experts is vital for SCD care. This team has doctors, nurses, and more. They work together to handle the disease.
Key members of the care team include:
Regular checks are key for SCD care. They catch problems early, so they can be fixed fast.
| Screening Type | Frequency | Purpose |
| Blood tests | Regularly scheduled | Monitor hemoglobin levels and detect complications |
| Imaging studies (e.g., ultrasound) | As needed | Assess organ damage or other complications |
| Ophthalmologic exams | Annually | Detect retinopathy and other eye complications |
Special centers offer focused care for SCD patients. They provide medical help, education, and support.
Benefits of specialized centers include:
Holistic care improves SCD patients’ lives. It covers their physical, emotional, and social needs.
Components of holistic care include:
Living with sickle cell anemia is a complex journey. It involves medical treatment and lifestyle changes. Patients face many challenges that affect their health, mental well-being, and social life.
Managing sickle cell disease (SCD) requires a full approach. Quality of life considerations are key. They help patients live active and fulfilling lives. Chronic pain, fatigue, and frequent hospital stays can greatly impact their lives.
DelveInsight’s data shows SCD patients often struggle with quality of life. They face chronic pain and psychological distress. Effective management strategies are vital to reduce these effects.
Mental health support is critical for SCD patients. The disease’s chronic nature and unpredictable pain can cause anxiety and depression. Mental health professionals and support groups offer emotional support and coping strategies.
Education and employment are important for SCD patients. Accommodations and understanding from schools and employers are key. Patients need to know their rights and available resources, like disability benefits and vocational programs.
| Support Resources | Description | Benefits |
| Support Groups | Connecting patients with others who share similar experiences | Emotional support, coping strategies |
| Mental Health Services | Professional help for anxiety, depression, and other mental health issues | Improved mental well-being, stress management |
| Patient Assistance Programs | Financial and logistical support for managing SCD | Reduced financial burden, access to necessary treatments |
Support groups and resources are vital for SCD patients. They offer a place to share experiences, get emotional support, and find information and services. These resources can improve quality of life.
By using these resources and a full management plan, SCD patients can lead more fulfilling lives. Despite the challenges, they can overcome them.
The cost of sickle cell disease treatment is a big worry for patients and their families. It includes many expenses like medicines, hospital stays, and ongoing care.
Insurance is key to making SCD treatment affordable. Most plans help cover the costs of treatments like hydroxyurea and blood transfusions. But, how much they cover can differ a lot.
Understanding insurance coverage is vital for managing costs. Patients should check their policies and talk to doctors to find the best options.
Patient assistance programs (PAPs) help patients get treatments at a lower cost or for free. Many drug companies offer PAPs for SCD medicines like hydroxyurea and crizanlizumab.
The Patient Access Network Foundation helps SCD patients with financial aid. They cover copays, deductibles, and other costs.
The financial effect of SCD on families is huge. A study by Survey Reports LLC shows the treatment costs a lot. It puts a big economic burden on patients and their families.
“The economic burden of sickle cell disease is not just a financial issue; it affects the overall quality of life for patients and their families.”
Advocacy is key to getting treatments and coverage. Groups like the Sickle Cell Disease Association of America push for better policies. They aim to improve insurance and care access for SCD patients.
Patients and families can also advocate. They can share their stories with policymakers and insurance companies.
Sickle cell disease research is on the verge of a major breakthrough. This is thanks to new gene therapy and editing technologies. New therapies, like gene editing and therapy, could change how we treat SCD.
Researchers are working hard to find new treatments for SCD. They want to fix the genetic problem at its source. Gene therapy is leading this effort, aiming to correct the genetic defect.
Gene editing technologies, like CRISPR, are also being looked into. They could edit the genes causing SCD, which could lead to a cure. These new methods are being tested in clinical trials, showing great promise.
The future of SCD research will likely see more progress in gene therapy. Researchers will also explore new targets for treatment. As they do, these new treatments could greatly improve patients’ lives.
Recent studies suggest that new treatments, including gene editing and therapy, will change SCD treatment. These advances highlight the need for continued research and investment in SCD treatments.
Advances in sickle cell disease (SCD) treatment have greatly improved patient outcomes. Yet, challenges persist. Ongoing research and new therapies offer hope for better SCD management and a possible cure.
A complete care approach is key for managing SCD. This includes medical treatment, lifestyle changes, and support. The future of SCD management is bright, thanks to research into gene therapy and CRISPR gene editing.
It’s vital to keep investing in SCD research and development. This will help us find a lasting solution for SCD. The progress in SCD care is leading to better patient outcomes and a higher quality of life.
Sickle cell disease is a genetic disorder that affects how red blood cells are made. It causes these cells to become rigid and sickle-shaped.
Yes, treatments like bone marrow transplantation and gene therapies can cure sickle cell anemia. But, these treatments are not available to everyone.
Symptoms include severe pain, chronic anemia, and damage to organs. People with sickle cell anemia also face a higher risk of infections and other problems.
Sickle cell disease is inherited in a specific way. A person needs to get two mutated HBB genes, one from each parent, to have the disease.
People with sickle cell trait have one normal and one mutated gene. Those with sickle cell disease have two mutated genes, leading to full symptoms.
Treatments include managing pain, hydroxyurea therapy, blood transfusions, and FDA-approved drugs like L-glutamine and voxelotor.
Gene therapy might cure sickle cell disease by fixing or replacing the faulty HBB gene. It’s an emerging treatment with ongoing trials.
CRISPR/Cas9 is a tool that can fix the genetic mutation causing sickle cell disease. Trials are checking if it’s safe and effective.
Managing symptoms requires a few steps. This includes preventive measures, lifestyle changes, and quick medical help. Staying hydrated and avoiding triggers is key.
Treating sickle cell disease is expensive. It includes costs for medications, hospital stays, and ongoing care. Insurance, patient programs, and advocacy can help with costs.
Yes, new treatments like gene-editing therapies and small molecules are being tested. They aim to improve patient outcomes.
Complete care involves a team approach. It includes regular check-ups, monitoring, and holistic care. You can find this care at specialized centers and with healthcare providers.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!