Last Updated on October 21, 2025 by mcelik

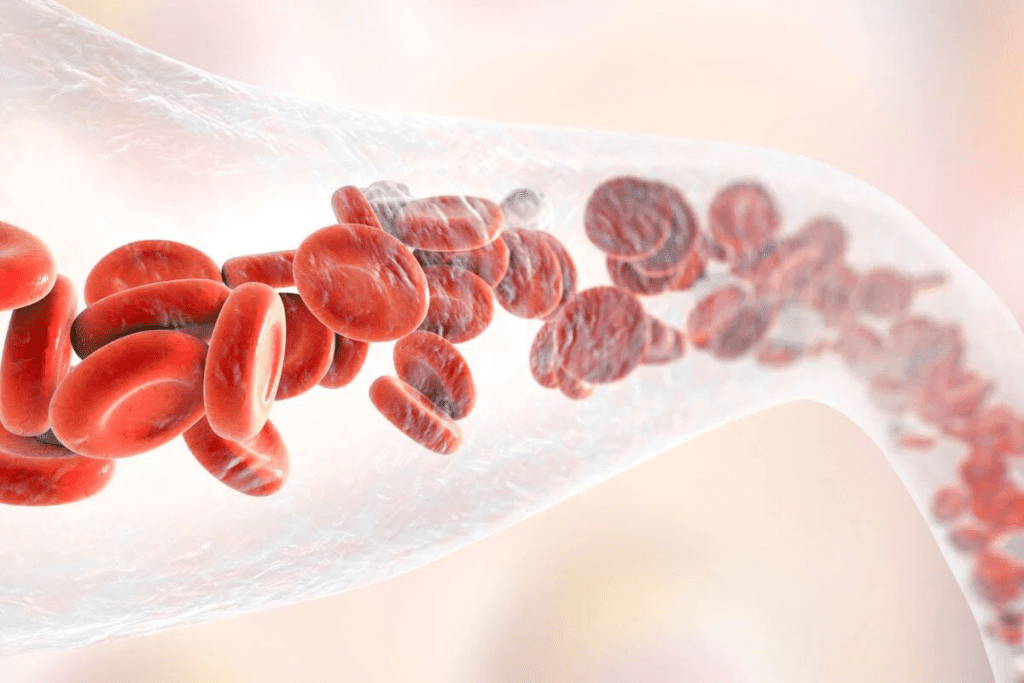
Nearly 250,000 cases of bacteremia happen every year in the United States. This leads to a lot of sickness and death.
Bloodstream infections, or bacteremia, occur when bacteria enter the bloodstream. If not treated right away, they can cause serious problems.
Understanding the most common types of blood infections is crucial for early detection and treatment by healthcare providers. This article will explain the different types, their causes, and how to treat them.
Bacteremia is when bacteria are found in the blood. It’s a serious issue that needs quick medical help. Bloodstream infections happen when harmful germs get into the blood, causing serious health problems.
These infections can come from many places. They might start in other body parts, happen during medical procedures, or come from dirty medical tools. Knowing about bacteremia helps us prevent, find, and treat it.
Bacteremia means there are live bacteria in the blood. It can be short-term or last a long time. Having bacteria in the blood can cause mild or serious health issues.
The term “bacteremia” is often mixed up with “septicemia.” But they mean different things in medicine. Knowing the difference is key for correct diagnosis and treatment.
| Term | Definition |
| Bacteremia | Presence of bacteria in the blood |
| Septicemia | Presence of pathogenic microorganisms or their toxins in the blood |
| Sepsis | Life-threatening organ dysfunction caused by a dysregulated host response to infection |
Germs can get into the blood in many ways. They might come from infections elsewhere in the body, like pneumonia or urinary tract infections. They can also get in through medical procedures, like those using catheters.
Other things can increase the risk of getting bacteremia. These include a weak immune system, long-term health issues, and having medical devices. Knowing these risks helps us avoid bloodstream infections.
The ways germs get into the blood are complex. Understanding these paths is vital for stopping and treating infections.
Bacteremia is when living bacteria are found in the blood. This can be very serious and lead to infections that are mild or life-threatening.
Bacteremia means bacteria are in the blood. It can be transient, meaning it’s short-lived and often goes away by itself. Or, it can be persistent, showing a serious infection that needs medical help.
The term “bacteremia” is sometimes mixed up with “septicemia.” But they mean different things in medicine. Knowing what bacteremia is helps doctors treat blood infections right.
Transient bacteremia is a short-term issue. It might happen when you brush your teeth or have a medical test. Healthy people usually can fight off these bacteria.
Persistent bacteremia means bacteria are stuck in the blood. This can cause serious infections and problems. It needs quick medical care to avoid big health issues.
Understanding the most common types of blood infections is crucial for early detection and treatment by healthcare providers.best treatment and lower the risk of serious problems.
Understanding the most common types of blood infections is crucial for early detection and treatment by healthcare providers.ys. Knowing how they get there helps doctors treat them better.
Primary bloodstream infections have no clear source outside the blood. They are often caused by bacteria or fungi that directly get into the blood. These infections are hard to diagnose because they don’t have a clear source.
A study in the Journal of Clinical Microbiology found these infections are serious. They can be deadly, mainly for people with weakened immune systems.
Secondary bloodstream infections start from an infection elsewhere in the body. They can come from the urinary tract, lungs, or skin. Turning from a local infection to a blood infection makes treatment harder.
The Centers for Disease Control and Prevention (CDC) says these infections are a big worry in hospitals.
Catheter-associated bloodstream infections (CABSIs) are a big problem in hospitals. They happen when bacteria or fungi on a catheter get into the blood. These infections can be stopped with good catheter care.
The CDC has rules to lower the number of CABSIs. They focus on clean insertion and watching the catheter closely.
This includes teaching, watching closely, and following best practices in catheter care.
“The prevention of catheter-associated bloodstream infections is a critical aspect of patient safety in healthcare settings.”
In summary, knowing about the different blood infections is key for doctors. It helps them find better ways to treat patients and save lives.
Bacteremia and sepsis are two related but different medical conditions. They both involve pathogens in the blood. But, they have different effects on the body and how it responds.
Bacteremia means bacteria are in the blood. It can last for a short time or longer, depending on the immune system’s action.
Sepsis is a serious condition where the body’s response to infection harms its own tissues and organs. It’s caused by an uncontrolled body response to infection, leading to organ failure.
| Condition | Definition | Clinical Implication |
| Bacteremia | Presence of bacteria in the blood | Can be transient or persistent; not all bacteremia leads to sepsis |
| Sepsis | Life-threatening organ dysfunction caused by a dysregulated response to infection | Requires immediate medical attention; high mortality risk if untreated |
The move from bacteremia to sepsis is complex. It involves the pathogen and the host’s immune response. Not every bacteremia turns into sepsis, but it can if it does, it’s very serious.
It’s key to know the difference between bacteremia and sepsis for quick and right action. Doctors must watch closely and act fast to avoid bad outcomes.
Bacteremia and septicemia are related but different. They both involve pathogens in the blood. It’s key for doctors and patients to know the difference.
Bacteremia means bacteria are in the blood. It can last a short time or longer, based on the cause and how the body reacts.
Septicemia is a more serious case. It happens when bacteria in the blood cause a widespread infection, possibly leading to sepsis.
“The terms bacteremia and septicemia are often used interchangeably, but they have different implications for patient care and treatment outcomes.”
| Condition | Definition | Clinical Implication |
| Bacteremia | Presence of bacteria in the blood | Can be transient or persistent; may or may not lead to sepsis |
| Septicemia | Systemic infection due to pathogens in the blood | Often associated with sepsis; requires immediate medical attention |
Bacteremia and septicemia have different effects. Bacteremia might go away with treatment or on its own. But septicemia is a sign of a serious infection that could turn into sepsis, a deadly condition.
It’s vital to know the difference between bacteremia and septicemia for the right treatment. Doctors must act fast to avoid serious problems.
Bacteremia happens when bacteria or fungi get into the blood. This can lead to serious infections. Knowing what causes bacteremia helps doctors treat and prevent it.
Gram-positive bacteria often cause bacteremia. Staphylococcus aureus is a top gram-positive bacterium that leads to infections in the blood. These bacteria can get into the blood through skin infections, medical devices, or contaminated catheters.
Staphylococcus aureus infections in the blood are very serious. They can make people very sick and even kill them.
Gram-negative bacteria also cause bacteremia. Escherichia coli (E. coli) is a common gram-negative bacterium that can get into the blood. It often comes from urinary tract infections or abdominal infections.
Other gram-negative bacteria, like Klebsiella pneumoniae and Pseudomonas aeruginosa, can also cause infections in the blood. These infections are very serious and need quick treatment with antibiotics.
Fungal infections in the blood are less common but serious. Candida species are the main cause of fungal bacteremia. They often happen in people with weakened immune systems, due to things like central venous catheters, broad-spectrum antibiotics, or immunosuppressive therapy.
Fungal infections in the blood are hard to diagnose and treat. They need antifungal therapy and managing the risk factors.
In summary, bacteremia can come from many bacteria and fungi. Knowing the causes is key to managing and treating these infections.
Understanding the most common types of blood infections is crucial for early detection and treatment by healthcare providers.mild to serious. Knowing these signs helps you get the right care.
The first signs of bacteremia can be hard to spot. They might look like other infections. Common early signs include:
These symptoms can be like those of other infections. If they don’t go away or get worse, see a doctor.
Some cases of bacteremia can get very serious. These symptoms mean you need to see a doctor right away. Severe symptoms include:
If you or someone you know has these symptoms, get help fast.
Bacteremia can show up differently in different people. For example:
| Population | Typical Symptoms |
| Elderly | Often present with confusion, altered mental status, or falls. Fever may be absent. |
| Immunocompromised | May have subtle or atypical symptoms, such as mild fever or malaise, without clear signs of infection. |
| Children | Can present with fever, irritability, and lethargy. Infants may have nonspecific signs like poor feeding or vomiting. |
Knowing these differences helps doctors treat bacteremia better in all kinds of patients.
Several factors can increase the risk of getting blood infections. These include medical conditions, invasive procedures, and lifestyle choices. Knowing these risks helps identify who is more likely to get bacteremia and other bloodstream infections.
Some medical conditions make it more likely to get blood infections. These include:
| Medical Condition | Increased Risk Due To |
| Diabetes | Compromised immune response |
| Immunosuppression | Weakened immune system |
| Cancer | Chemotherapy, disease progression |
| Chronic Kidney Disease | Dialysis, reduced immune function |
Some medical procedures can also raise the risk of blood infections. These include:
Lifestyle and environmental factors also play a role in the risk of blood infections. These include:
Understanding these risk factors helps healthcare providers take steps to prevent blood infections. This includes proper catheter care, following hygiene protocols, and managing medical conditions well.

Diagnosing bacteremia involves both clinical evaluation and lab tests. Doctors look at symptoms, medical history, and risk factors to choose the right tests.
Blood culture is the top choice for finding bacteremia. It takes a blood sample and grows any microorganisms in a special medium. A positive blood culture shows bacteria or fungi in the blood, helping doctors pick the right treatment.
Getting a blood culture right is key. It must be done carefully to avoid contamination. Labs use machines to watch the cultures, helping find microorganisms faster.
Even though blood culture is key, other tests are important too. These include:
These tests help doctors understand what’s going on. They work together with clinical judgment to diagnose and treat bacteremia.
New rapid diagnostic technologies have changed microbiology. Tools like PCR and MALDI-TOF mass spectrometry quickly identify pathogens from blood cultures. This means doctors can start treatment sooner.
These quick tests also include checking how bacteria react to antibiotics. This is key for choosing the right treatment. Using these technologies can lead to better patient care by speeding up diagnosis and treatment.
Understanding the most common types of blood infections is crucial for early detection and treatment by healthcare providers. immune systems. They need special care because they get sick more easily.
Blood infections in kids are tough because their immune systems are not fully grown. Spotting symptoms early is key to avoid serious problems. Kids can get these infections from birth, respiratory issues, or catheters.
Quick action with the right antibiotics is vital for kids. The antibiotic choice depends on the infection source and local resistance.
The elderly face a higher risk of blood infections. This is because their immune systems weaken with age, and they often have other health issues. Identifying signs of bacteremia in seniors can be hard because of their chronic conditions.
Seniors might need stronger treatments and closer watch because of their higher risk of serious problems and death. Thinking carefully about kidney function and drug interactions is key when picking antibiotics for them.
People with weakened immune systems, like those with HIV/AIDS, cancer, or taking immunosuppressants, are very prone to blood infections. Handling bacteremia in these folks means using the right antibiotics and boosting their immune system.
Preventive steps might be taken for those at high risk. This could include using antibiotics to prevent infections and avoiding things that could cause infections.
Managing bacteremia well means starting the right treatment quickly. This includes empiric antibiotic therapy and targeted antimicrobial treatment. The choice depends on the likely cause, how severe the infection is, and the patient’s health.
Empiric antibiotic therapy starts when a blood infection is suspected. It uses broad-spectrum antibiotics to cover many possible bacteria. This is before knowing the exact cause.
Choosing the right antibiotics is based on local resistance patterns, allergies, and the likely source of infection. For example, those with catheter infections might need antibiotics for Staphylococcus aureus and other common bacteria.
After finding the cause through blood tests, targeted antimicrobial treatment begins. This treatment is more specific, aimed at the exact pathogen. It helps avoid resistance and side effects.
Targeted therapy is customized for each patient. It considers the pathogen’s resistance, the infection site, and how the patient responds. For Staphylococcus aureus infections, for example, vancomycin or daptomycin might be used based on the test results.
Along with antibiotics, source control measures are key. These steps find and fix the infection’s source. This could mean removing infected devices or draining abscesses.
Supportive care interventions are also essential. They include fluids, blood pressure support, and managing organ problems. Patients with severe infections might need ICU care.
Supportive care also watches for complications and prevents long-term damage. Good supportive care can greatly improve survival rates for bacteremia patients.
The time it takes to recover from bacteremia depends on several things. These include the type of bacteria, the patient’s health, and how quickly and well treatment works. Knowing these factors is key to managing the condition and helping patients get better.
Bacteremia can vary in its course. Some cases are short-lived and linked to minor infections or procedures. These usually clear up quickly with little treatment needed. But, persistent bacteremia is a sign of a serious infection that needs urgent care.
Prompt treatment is essential to avoid serious issues and improve chances of recovery. The severity of the bacteria and the patient’s immune system also play a role in how the infection progresses.
Several things can impact how long it takes to recover from bacteremia. These include:
A study in a medical journal found that “The recovery time from bacteremia can be significantly influenced by the appropriateness of initial antibiotic therapy.”
“Early and appropriate antibiotic therapy is key to the outcome of bacteremia.”
It’s important to keep an eye on patients after they’ve had bacteremia. This ensures the infection is gone and manages any long-term effects. This might mean regular doctor visits, more tests, and sometimes longer antibiotic use.
People who’ve had bacteremia should watch for signs of relapse or complications. These include fever, chills, or other infection signs. If these symptoms show up, they should get medical help right away.
Good management and follow-up care can greatly improve the outlook for patients with bacteremia.
If left untreated, bacteremia can lead to serious and life-threatening conditions. These complications can significantly affect patient outcomes. They may also cause long-term health issues or even death.
Septic shock is a critical complication of untreated bacteremia. It happens when the body’s response to an infection gets out of control. This causes widespread inflammation and a drop in blood pressure.
Septic shock can progress quickly. This makes early detection and treatment essential. Patients often need intensive care, like mechanical ventilation and vasopressor support, to manage their condition.
Untreated bacteremia can also cause organ dysfunction. This happens when the infection spreads and damages various body systems. The way organ dysfunction shows up depends on the organs affected.
| Organ/System | Potential Dysfunction |
| Kidneys | Acute Kidney Injury (AKI) |
| Lungs | Acute Respiratory Distress Syndrome (ARDS) |
| Liver | Hepatic Dysfunction |
Organ dysfunction makes patient care more complex and worsens the prognosis. Early treatment of bacteremia is key to preventing these complications.
Survivors of severe bacteremia and sepsis may face long-term health issues. These include cognitive impairment, physical disability, and psychological distress. These issues can greatly affect their quality of life and require ongoing medical care.
Long-term consequences may include:
Understanding the long-term health consequences of untreated bacteremia is vital. It shows the importance of prompt and effective treatment. Survivors often need ongoing care to manage these issues.
Stopping blood infections is a team effort. It involves steps taken in healthcare settings and personal actions. We need to follow infection control rules, teach patients, and make sure healthcare workers know what to do.
Keeping healthcare areas clean can cut down on infections. Proper hand hygiene is key. Healthcare workers must wash their hands before and after touching patients or devices.
“Hand hygiene is the cornerstone of infection prevention. It’s simple yet highly effective in reducing the transmission of pathogens.”
Using personal protective equipment (PPE) is also important. PPE like gloves, gowns, and masks stops germs from spreading.
| Infection Control Measure | Description | Benefit |
| Hand Hygiene | Washing hands with soap and water or using alcohol-based hand rubs | Reduces transmission of pathogens |
| Use of PPE | Wearing gloves, gowns, and masks | Prevents spread of infectious agents |
| Sterilization of Equipment | Ensuring medical instruments are properly sterilized | Eliminates pathogens from medical equipment |
Central venous catheters can lead to infections. Keeping them clean is vital. Use sterile methods when putting them in, check for signs of infection, and remove them when not needed.
Healthcare places should use catheter bundles. These include hand washing, careful insertion, and skin cleaning with chlorhexidine.
Patients can help prevent infections too. Knowing your risks and taking steps to lower them is important. This means managing health conditions well and avoiding risky behaviors.
By working together, we can lower blood infection rates. This improves health outcomes and the quality of care.
Bacteremia and blood infections are serious issues that need quick action and treatment. It’s important to know the causes, symptoms, diagnosis, and treatment options. This knowledge helps in managing and preventing these conditions.
Understanding bacteremia shows it can be caused by different pathogens, like bacteria and fungi. If not treated, it can lead to severe complications. Knowing the risk factors helps identify who is at high risk.
Preventing blood infections is possible through effective strategies. Proper care and maintenance of catheters are key. By understanding bacteremia and blood infections, healthcare professionals and individuals can work together. This teamwork improves patient outcomes.
Bacteremia is when bacteria get into the bloodstream. This can cause serious problems if not treated right away.
Transient bacteremia is short-lived and often goes away by itself. But, persistent bacteremia can lead to serious infections and problems.
Blood infections can be primary, secondary, or linked to catheters. Each type has its own causes and risks.
Bacteremia means bacteria are in the blood. Sepsis is a serious condition where the body’s response to an infection harms its own tissues and organs.
Both refer to pathogens in the blood. But, septicemia is more severe and often means the condition is worse.
Bacteremia can be caused by many things. This includes infections from gram-positive and gram-negative bacteria, and even fungal infections.
Symptoms can vary. Early signs include fever, chills, and feeling very tired. Severe symptoms like trouble breathing or severe pain need immediate help.
Some people are more at risk. This includes those with diabetes or weakened immune systems. Also, certain medical procedures and lifestyle choices can increase risk.
Doctors use blood cultures to diagnose bacteremia. They also use other tests and quick diagnostic tools.
Treatment includes starting antibiotics right away. Doctors also focus on finding and treating the source of the infection. Supportive care is also important.
If left untreated, blood infections can cause serious problems. This includes septic shock, organ failure, and long-term health issues.
Preventing blood infections requires several steps. This includes good infection control, proper care of medical devices, and educating patients.
The outcome depends on many factors. This includes the type of bacteria and the patient’s overall health.
Recovery time varies. It depends on how severe the infection is and how well treatment works.
Yes, positive blood cultures mean you have bacteremia. It’s important to treat it quickly to avoid serious problems.
Yes, antibiotics are the main treatment for bacteremia. The choice of antibiotic depends on the bacteria causing the infection and how severe it is.
Edris, Y., et al. (2025). Epidemiology of Community-acquired Bacteremia Among Children in Eastern Ethiopia: High Mortality and Antimicrobial Resistance Patterns. Wolters Kluwer Health. Retrieved from
Bearman, G. M. L. (2005). Bacteremias: A Leading Cause of Death. Revista Española de Enfermedades Infecciosas y MicrobiologÃa ClÃnica (English Edition). Retrieved from
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!