Last Updated on November 26, 2025 by Bilal Hasdemir

Chemotherapy, or chemo, is a key treatment for many cancers. But, it can have side effects. Knowing how chemo affects the body is important, especially the lungs.
Chemo can harm different parts of the body. This includes the bone marrow, hair follicles, and the mouth and digestive tract. It can also hurt the heart, kidneys, bladder, and lungs in some cases. We’ll look at how chemo impacts the body, focusing on lung damage.
Key Takeaways
- Chemotherapy can cause various side effects due to its impact on normal cells.
- Different organs can be affected, including the lungs, heart, and kidneys.
- Lung damage is a significant concern for patients undergoing certain types of chemotherapy.
- Understanding the potential side effects can help patients prepare and manage their treatment.
- It’s crucial to discuss potential risks with your healthcare provider.
The Systemic Nature of Chemotherapy
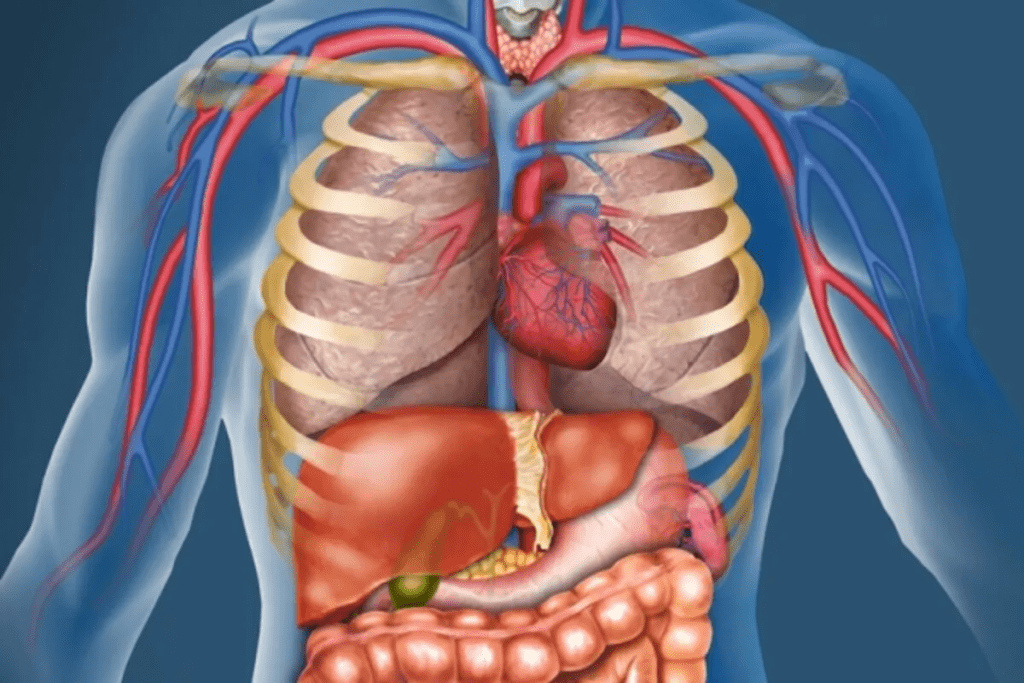
Chemotherapy targets fast-growing cells in the body. This includes both cancer cells and healthy ones. It’s a key way to fight cancer that has spread or might spread. We’ll look at how it works and its effects on the body.
How Chemotherapy Works in the Body
Chemotherapy drugs aim to kill fast-growing cells, like many cancer cells. But, they also harm some healthy cells. These are in the bone marrow, hair follicles, and the digestive tract’s lining.
This harm can cause side effects. For example, it can lower blood cell counts, leading to infections and anemia. Hair loss and digestive problems like nausea and mouth sores can also happen.
Why Chemotherapy Affects Multiple Organs
Chemotherapy affects many parts of the body because it’s systemic. Organs like the heart, lungs, liver, and kidneys can be hit hard. Some drugs can damage the heart or liver, while others might harm the kidneys.
Some organs and systems often get affected by chemotherapy include:
- The heart, potentially leading to cardiac complications
- The lungs, which can suffer from inflammation or fibrosis
- The liver, where toxicity can occur due to the metabolism of chemotherapy drugs
- The kidneys, which can be damaged by certain chemotherapy agents
It’s important for patients to understand how chemotherapy works and which organs are at risk. Knowing this helps them prepare for side effects and talk to their doctors about how to manage them.
Lung Damage Chemotherapy: A Primary Concern
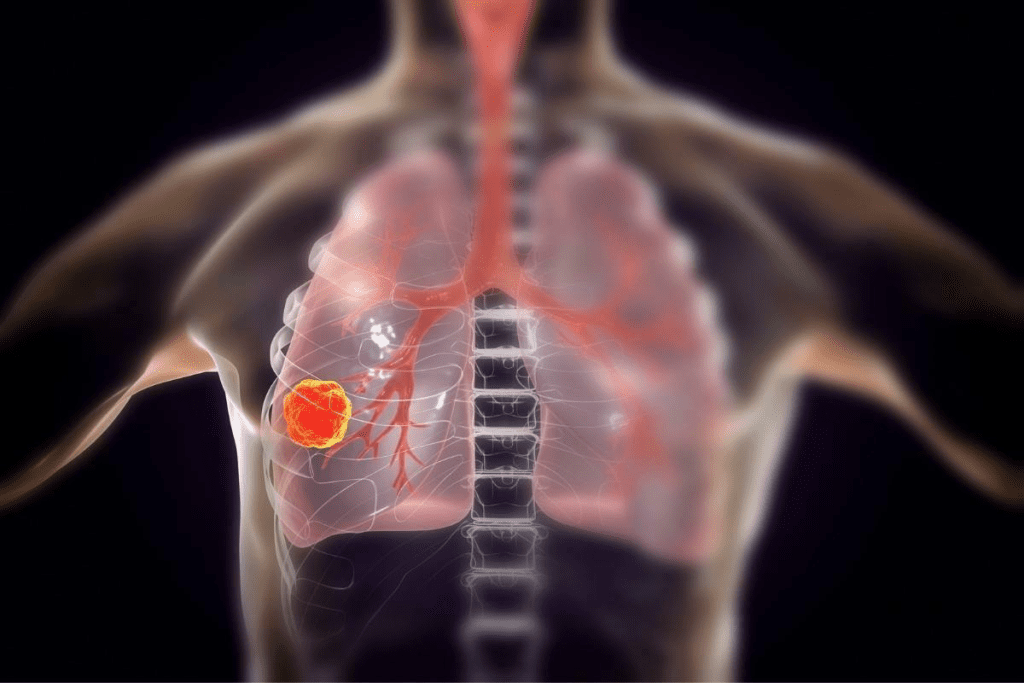
It’s important for patients and doctors to know about lung damage risks from chemotherapy. Chemotherapy is key in fighting cancer but can harm vital organs like the lungs.
Chemotherapy drugs can damage lungs in many ways. This can lead to mild to severe problems. We’ll look at the types of lung damage, who’s at higher risk, and which drugs can harm lungs.
Types of Lung Damage from Chemotherapy
Chemotherapy can lead to several lung problems, including:
- Pneumonitis: inflammation of the lung tissue
- Pulmonary fibrosis: scarring of the lungs
- Chronic obstructive pulmonary disease (COPD): a progressive lung disease
These issues can cause symptoms like shortness of breath, cough, and tiredness. They can really affect a patient’s life quality.
Risk Factors for Developing Pulmonary Complications
Some factors can make patients more likely to get lung problems from chemotherapy:
- Pre-existing lung disease
- Age: older patients are more susceptible
- Smoking history
- Previous radiation therapy to the chest
- Concurrent use of other medications that can cause lung damage
Knowing these risk factors helps doctors prevent and closely watch patients.
Common Chemotherapy Drugs Associated with Lung Toxicity
Some chemotherapy drugs are more likely to harm lungs:
- Bleomycin: often used to treat testicular cancer, Hodgkin’s lymphoma, and certain types of germ cell tumors
- Busulfan: used in conditioning regimens for hematopoietic stem cell transplantation
- Cyclophosphamide: used in various chemotherapy regimens
Knowing which drugs can harm lungs helps in planning treatment and monitoring.
Recognizing Symptoms of Chemotherapy-Induced Lung Injury
Spotting early signs of lung damage from chemo can really help patients. This serious issue can show up in many ways. It’s key for both patients and doctors to watch out for these signs.
Early Warning Signs
Look out for shortness of breath, cough, and fever as early signs. These symptoms can be tricky to spot because they can look like other health issues.
Some people might have a dry cough or a cough that won’t go away. Feeling out of breath, especially when you’re active, is another warning sign.
When to Seek Medical Attention
If you’re having trouble breathing, get help right away. For serious breathing problems, call 911.
Other signs that need a doctor’s check-up include a cough that gets worse or a fever.
Diagnostic Procedures for Lung Damage
Figuring out if chemo has hurt your lungs involves tests and doctor checks. Here’s a list of common tests:
| Diagnostic Procedure | Description |
| Pulmonary Function Tests (PFTs) | Checks how well your lungs work |
| Chest X-ray or CT Scan | Looks at lung damage with pictures |
| Blood Tests | Checks oxygen levels and health |
| Bronchoscopy | Looks directly at airways |
Getting a diagnosis early can help manage lung damage better. This can lead to better health outcomes for patients.
Cardiac Toxicity: Chemo Heart Damage
It’s important to know how chemotherapy affects the heart. While it fights cancer, it can harm the heart. This harm is called cardiac toxicity.
Acute vs. Chronic Cardiac Effects
Chemotherapy can harm the heart in two main ways. Acute effects happen right after treatment. They can cause arrhythmias, heart failure, and pericarditis. Chronic effects take months or years to show up and can cause lasting heart damage.
Knowing the difference helps us give better care. We need to watch for acute effects right away and chronic effects over time.
Cardiotoxic Chemotherapy Agents
Some chemotherapy drugs are more likely to harm the heart. These include:
- Anthracyclines (e.g., doxorubicin)
- Trastuzumab
- Alkylating agents
It’s key to know which drugs can harm the heart. This helps us manage risks better.
Monitoring Heart Function During Treatment
Watching the heart during chemotherapy is very important. It helps us catch heart problems early. This includes:
| Monitoring Method | Description | Frequency |
| Echocardiogram | Checks heart function and structure | Baseline, after 3-6 cycles, and at end of treatment |
| MUGA Scan | Looks at left ventricular ejection fraction (LVEF) | Baseline and periodically during treatment |
| Biomarkers (e.g., troponin) | Finds cardiac injury | Baseline, during, and after treatment |
Regular checks let us act fast and adjust treatments. This helps lower heart risks.
Liver Damage from Chemotherapy
The liver is key for detox and metabolism. It can get hurt by chemotherapy. We must know how these drugs affect the liver.
How Chemotherapy Affects Liver Function
Chemotherapy targets fast-growing cancer cells. But, it can also harm fast-growing cells in the liver. The liver breaks down these drugs, which can change liver function tests.
Some drugs can cause liver toxicity. This leads to high liver enzymes and serious problems.
We must watch the liver closely during treatment. The liver might not process drugs well, causing toxin buildup.
Signs of Liver Toxicity
It’s important to spot liver toxicity early. Look out for:
- Jaundice (yellowing of the skin and eyes)
- Fatigue
- Nausea and vomiting
- Abdominal pain or swelling
- Dark urine or pale stools
These signs mean the liver might not be working right. Tell your doctor right away. Early action can prevent serious liver damage.
Liver Function Tests During Treatment
Liver function tests (LFTs) are key during chemotherapy. They check enzymes and proteins in the blood. This shows how the liver is doing.
- Alanine transaminase (ALT)
- Aspartate transaminase (AST)
- Alkaline phosphatase (ALP)
- Bilirubin levels
Regular LFTs help doctors see how the liver is doing. They can decide if treatment needs to change. If the liver shows big problems, they might adjust the treatment to protect it.
By watching the liver closely, we can lessen damage from chemotherapy. This helps patients get better results.
Kidney Toxicity from Chemotherapy
Chemotherapy is a lifesaver but can harm organs like the kidneys. Some chemotherapy drugs can damage the kidneys. Knowing these risks helps in preventing kidney damage.
Mechanisms of Renal Damage
Chemotherapy can harm the kidneys in several ways. Some drugs directly damage kidney cells. Others cause inflammation or harm blood vessels in the kidneys. The kidneys filter waste, making them vulnerable to chemotherapy’s toxic effects.
Key mechanisms include:
- Direct cytotoxic effects on renal cells
- Induction of oxidative stress
- Inflammation within the kidney
- Damage to renal blood vessels
Risk Factors for Kidney Injury
Several factors can increase the risk of kidney injury during chemotherapy. Kidney disease, dehydration, and certain medications can raise this risk. The type and dose of chemotherapy also play a big role.
| Risk Factor | Description |
| Pre-existing Kidney Disease | Patients with chronic kidney disease are more susceptible to further kidney damage. |
| Dehydration | Adequate hydration is crucial to help the kidneys process chemotherapy drugs. |
| Concomitant Medications | Certain drugs can increase the risk of kidney damage when used alongside chemotherapy. |
Protecting Kidney Function During Treatment
Protecting kidney function during chemotherapy requires a few steps. Keeping well-hydrated, checking kidney function with blood tests, and adjusting drug doses are key. Sometimes, medications to protect the kidneys are given.
By understanding the risks and taking proactive steps, we can reduce chemotherapy’s impact on kidney function. This helps in providing better care for patients with cancer.
Chemo Brain: Cognitive and Neurological Effects
Many patients face “chemo brain” as a side effect of chemotherapy. This condition makes it hard to remember things, focus, and process information.
Understanding Cognitive Impairment During Treatment
“Chemo brain” can be caused by the treatment itself, the body’s reaction to cancer, and stress. Research shows that some chemotherapy drugs can harm the brain, causing cognitive changes. Patients might struggle with:
- Memory recall
- Concentration and focus
- Processing speed
- Multitasking
These issues can be tough, but they often get better once treatment ends.
Long-term Neurological Consequences
Some patients may see lasting effects on their brain after chemotherapy. Research indicates that some chemotherapy can permanently affect the brain, leading to ongoing cognitive problems. The risk depends on:
- The type and dose of chemotherapy
- The patient’s age and overall health
- The presence of other medical conditions
Experts say understanding the impact of chemotherapy on the brain is complex. They stress the need for more research.
“Chemotherapy-induced cognitive impairment is a significant concern for cancer survivors, affecting their quality of life and ability to return to normal activities.”
Strategies for Managing Cognitive Changes
There are ways to manage cognitive changes during and after chemotherapy. These include:
- Cognitive training and rehabilitation programs
- Mindfulness and relaxation techniques
- Physical exercise and activity
- Organizational tools and memory aids
Using these strategies can help patients deal with “chemo brain.” It’s important for them to talk to their healthcare team. This way, they can create a plan tailored to their needs.
Bone Marrow Suppression and Blood Cell Production
The bone marrow is key for making blood cells. It’s hit hard by chemotherapy. This is because chemotherapy targets fast-growing cells, like cancer and blood-making cells.
Impact on White Blood Cells, Red Blood Cells, and Platelets
Chemotherapy can lower the number of white blood cells, red blood cells, and platelets. White blood cells fight infections, red blood cells carry oxygen, and platelets help blood clot. Fewer of these cells can cause infections, anemia, and bleeding.
Infection Risk and Management
Less white blood cells, especially neutrophils, means more infections. We’ll talk about how to lower this risk. This includes using granulocyte-colony stimulating factor (G-CSF) to boost white blood cells. Also, keeping clean and avoiding germs is key.
Recovery of Bone Marrow Function
But, bone marrow usually gets better after chemotherapy stops. How fast it recovers depends on the treatment. We’ll cover what affects recovery and how to help it along.
Knowing how chemotherapy affects bone marrow and blood cells is vital. It helps manage treatment side effects. By understanding the risks and taking steps to prevent them, patients can improve their treatment outcome.
Digestive System Damage from Chemotherapy
The digestive system is very sensitive to chemotherapy. This can lead to many problems that affect a patient’s life a lot. Chemotherapy harms cells that grow fast, like those in the digestive tract. This causes many side effects in the stomach and intestines.
Oral and Esophageal Complications
Chemotherapy often causes mouth problems, like mucositis. Mucositis is when the mouth’s lining gets inflamed and ulcers. It can hurt, make swallowing hard, and increase infection risk. To deal with it, we tell patients to brush gently, use saltwater rinses, and avoid spicy or acidic foods.
Esophageal issues can also happen, like esophagitis. This is when the esophagus gets inflamed. Symptoms include trouble swallowing, chest pain, and heartburn. We help by changing what and when they eat, and telling them not to lie down after meals.
Stomach and Intestinal Effects
Chemotherapy can mess with the stomach and intestines. It can cause nausea, vomiting, diarrhea, and constipation. Nausea and vomiting are common, with some drugs causing more problems. We use medicines, change diets, and try things like acupuncture to help.
Diarrhea and constipation can also happen. This is because chemotherapy affects the lining of the intestines and how they move. We help by changing diets, staying hydrated, and sometimes using medicines to control bowel movements.
Managing Gastrointestinal Side Effects
It’s important to manage side effects to keep patients healthy and well-nourished. We use diets, medicines, and other support to help. For example, we might suggest a diet that’s full of nutrients but easy on the stomach, along with medicines to stop nausea and vomiting.
| Gastrointestinal Side Effect | Management Strategies |
| Nausea and Vomiting | Anti-emetic medications, dietary adjustments, acupuncture |
| Diarrhea | Dietary changes, hydration, anti-diarrheal medications |
| Constipation | Dietary fiber, hydration, laxatives |
| Mucositis | Good oral hygiene, pain management, avoiding irritants |
By knowing about chemotherapy’s effects on the digestive system and how to manage them, we can make patients’ lives better during treatment.
Chemo Nerve Damage: Peripheral Neuropathy
Peripheral neuropathy is a common side effect of chemotherapy. It can greatly affect a patient’s quality of life. This condition damages the peripheral nerves. These nerves help send signals between the brain, spinal cord, and the rest of the body.
Symptoms and Progression
The symptoms of peripheral neuropathy vary. They depend on which nerves are affected. Common symptoms include:
- Numbness or tingling in the hands and feet
- Pain or burning sensations
- Muscle weakness
- Sensitivity to touch
These symptoms can get worse over time. If not treated, they can become permanent. This can greatly affect a patient’s daily life and overall well-being.
Chemotherapy Agents Most Likely to Cause Neuropathy
Some chemotherapy agents are more likely to cause peripheral neuropathy. These include:
- Platinum-based drugs (e.g., cisplatin, oxaliplatin)
- Taxanes (e.g., paclitaxel, docetaxel)
- Vinca alkaloids (e.g., vincristine)
Knowing which drugs are more likely to cause neuropathy helps in managing this side effect.
Treatment Options for Chemotherapy-Induced Neuropathy
Managing peripheral neuropathy requires a multi-faceted approach. Treatment options include:
- Medications to alleviate pain and other symptoms
- Physical therapy to maintain muscle strength and flexibility
- Lifestyle modifications such as avoiding cold temperatures and wearing comfortable clothing
In some cases, changing the chemotherapy regimen may be needed. This can help prevent further nerve damage. We work closely with patients to develop a personalized plan. This plan aims to manage neuropathy and improve their quality of life.
Impact on the Immune System
Chemotherapy can weaken the immune system, making patients more likely to get sick. This is a big deal in cancer treatment. It affects how well the treatment works and the patient’s life quality.
Short-term and Long-term Immune Suppression
Chemotherapy can weaken the immune system in two ways. Short-term immune suppression happens during and right after treatment, raising the risk of infections. Long-term immune suppression can last for months or even years after treatment stops. It makes it hard for patients to fight off diseases.
Effects on Immune Cells
Chemotherapy harms different immune cells, like white blood cells. These cells are key in fighting off infections. The table below shows how chemotherapy affects different immune cells.
| Immune Cell Type | Effect of Chemotherapy | Clinical Implication |
| Neutrophils | Decreased count | Increased risk of bacterial infections |
| Lymphocytes | Suppressed function | Impaired immune response to viruses and other pathogens |
| Monocytes | Variable effects | Potential for both immune suppression and activation |
Balancing Cancer Treatment and Immune Function
It’s hard to treat cancer without hurting the immune system. Doctors use different ways to lessen immune suppression. They adjust chemotherapy doses, use supportive care meds, and watch patients for signs of infection.
Fertility Concerns and Reproductive Organ Damage
Chemotherapy can have far-reaching consequences on fertility, making preservation options crucial for many patients. As we navigate the complexities of cancer treatment, understanding the potential impact on reproductive health is essential.
Effects on Male Fertility
Chemotherapy can significantly affect male fertility by damaging sperm cells and altering hormone levels. Drugs like cyclophosphamide and doxorubicin are known to have gonadotoxic effects, potentially leading to temporary or permanent infertility. We recommend that men discuss sperm banking with their healthcare provider before starting treatment.
Effects on Female Fertility
In women, chemotherapy can cause damage to the ovaries, leading to a reduction in egg quality and quantity. The risk of premature ovarian failure is a significant concern, especially with certain chemotherapy agents. The impact varies depending on age and the specific drugs used. Women should consider discussing fertility preservation options, such as egg freezing, with their oncologist.
Fertility Preservation Options
Fortunately, there are several fertility preservation options available for both men and women. These include sperm banking, egg freezing, and ovarian tissue freezing.
“Fertility preservation is a vital aspect of cancer care, and patients should be aware of their options to make informed decisions about their reproductive health.”-Experts highlight.
We encourage patients to consult with fertility specialists to explore the best options for their individual circumstances.
Treating and Managing Lung Toxicity from Chemotherapy
Managing lung damage from chemotherapy is key to better patient outcomes and quality of life. Lung damage can show up in many ways. We need a full approach that includes medical care, pulmonary rehab, and sometimes changing treatment plans.
Medical Interventions for Lung Damage
Medical treatments are vital for lung toxicity management. We use corticosteroids to fight inflammation, antibiotics to prevent infections, and meds for symptoms like coughing or shortness of breath. “Early treatment is crucial to avoid lasting damage,” say oncologists. These steps help ease symptoms and slow lung damage.
Corticosteroids are a mainstay for treating lung inflammation from chemo. The amount and length of corticosteroid use depend on the lung damage’s severity and the patient’s health.
Pulmonary Rehabilitation Approaches
Pulmonary rehab is a program that includes exercise, education, and support. It’s especially helpful for those with lung damage from chemo. It boosts lung function, stamina, and reduces symptoms.
- Exercise tailored to the patient’s abilities
- Breathing exercises to enhance lung function
- Education on symptom management and meds
- Nutritional advice for better health
Adding pulmonary rehab to treatment plans can greatly improve patients’ well-being.
When Treatment Modifications Are Necessary
At times, adjusting the chemo regimen is needed to manage lung toxicity. This might mean changing the dosage, switching drugs, or stopping treatment temporarily. The decision to change treatment depends on the lung damage’s severity and how the patient responds.
“The aim is to keep cancer treatment effective while reducing harm,” says a top oncologist. Changing treatment plans can help achieve this.
We closely watch patients and adjust their treatment as needed. This ensures the best results for them.
Minimizing Organ Damage During Chemotherapy
Managing damage from chemotherapy is a mix of medical steps and lifestyle changes. It’s key to act early to protect vital organs during treatment.
Preventive Medications and Approaches
Some medicines help shield organs from chemotherapy harm. For example, dexrazoxane guards the heart in patients getting anthracyclines. We also look into amifostine to lessen kidney and dry mouth risks.
We adjust how much and when chemotherapy is given to cut down on side effects. Our team keeps a close eye on each patient to find the best plan for them.
Lifestyle Factors That May Reduce Toxicity
Changing your lifestyle can help lessen chemotherapy side effects. Eating a healthy diet and drinking plenty of water can help. Also, regular exercise that fits the patient’s health can boost well-being and lower organ damage risk.
It’s also important to avoid tobacco and limit alcohol use. These can make organ damage worse. We help patients talk to their doctors about how to improve their lifestyle.
The Role of Supportive Care
Supportive care is a big part of cancer treatment. It aims to ease symptoms and improve life quality. Our supportive care team helps manage side effects, offers nutrition advice, and provides mental support.
By using preventive medicines, making lifestyle changes, and supportive care, we can greatly reduce organ damage during chemotherapy. This makes treatment better for our patients.
Long-term Monitoring After Chemotherapy
After chemotherapy, patients need ongoing care. This care is key to spotting and handling late treatment effects. It helps ensure patients get the best care possible.
Follow-up Schedules for Different Organ Systems
Patients need regular check-ups after chemotherapy. These visits help keep an eye on different body parts. The timing of these visits depends on the treatment and the patient’s health.
For example, some treatments can harm the heart. So, these patients might need heart tests often. Others might need lung tests to check for breathing problems.
| Organ System | Potential Complications | Follow-up Tests |
| Cardiac | Heart failure, arrhythmias | Echocardiogram, ECG |
| Pulmonary | Fibrosis, pneumonitis | PFTs, Chest X-ray |
| Renal | Kidney damage, failure | Creatinine levels, eGFR |
Screening for Delayed Toxicity
Some chemotherapy can cause problems later on. These issues might show up months or years later. Regular checks are important for catching these problems early.
Some treatments can lead to new cancers. Catching these early can make treatment easier.
When Recovery Can Be Expected
Recovery times after chemotherapy vary. It depends on the treatment, the patient’s health, and any other health issues.
Some people recover quickly, while others face ongoing challenges. Ongoing care and support are key to managing these issues and improving life quality.
Understanding the need for long-term monitoring helps patients deal with life after chemotherapy. Following recommended follow-up plans is crucial.
Conclusion: Balancing Treatment Benefits and Organ Protection
Chemotherapy is a key treatment for many cancers. But, it’s also important to think about the risks and side effects. Protecting organs during chemotherapy is key to avoid long-term damage.
Managing chemotherapy side effects is crucial. It helps patients get the most from their treatment while keeping vital organs safe. Knowing the side effects and managing them early can lead to better results.
To balance treatment benefits and organ protection, we need a detailed plan. This includes watching closely, using preventive medicines, and making lifestyle changes. We must all work together to make smart treatment choices and handle side effects well.
This way, we can make sure patients get the treatment they need. And at the same time, protect their health and well-being.
FAQ
What are the common side effects of chemotherapy on the lungs?
Chemotherapy can harm the lungs, causing inflammation and scarring. It can also make breathing harder. Symptoms include shortness of breath, coughing, and trouble breathing.
How does chemotherapy affect the heart?
Some chemotherapy can damage the heart. This can lead to heart problems, like reduced function or failure. The risk depends on the type and dose of chemotherapy.
Can chemotherapy damage the liver?
Yes, chemotherapy can harm the liver. It can cause changes in liver function tests and inflammation. The risk varies based on the chemotherapy and the liver’s health before treatment.
What is the impact of chemotherapy on kidney function?
Chemotherapy can harm the kidneys. It can reduce kidney function, cause electrolyte imbalances, and even lead to failure. Some chemotherapy agents are more harmful to the kidneys than others.
What is “chemo brain” and how is it managed?
“Chemo brain” refers to brain fog caused by chemotherapy. It includes memory issues, trouble concentrating, and confusion. To manage it, cognitive training, lifestyle changes, and sometimes medication are used.
How does chemotherapy affect blood cell production?
Chemotherapy can damage the bone marrow. This reduces the production of blood cells, leading to infections, anemia, and bleeding. It affects white blood cells, red blood cells, and platelets.
What are the gastrointestinal side effects of chemotherapy?
Chemotherapy can cause nausea, vomiting, diarrhea, constipation, and mouth sores. To manage these, medications, dietary changes, and supportive care are used.
Can chemotherapy cause peripheral neuropathy?
Yes, some chemotherapy can cause peripheral neuropathy. This is a condition with numbness, tingling, and pain in the hands and feet. Treatment includes medications, physical therapy, and sometimes changing the chemotherapy.
How does chemotherapy affect the immune system?
Chemotherapy can weaken the immune system. This makes it harder to fight infections and can affect the body’s ability to fight cancer.
What are the fertility concerns associated with chemotherapy?
Chemotherapy can harm reproductive organs, affecting fertility in men and women. Options for preserving fertility include sperm banking, egg freezing, and ovarian tissue freezing.
How is lung toxicity from chemotherapy treated?
Lung toxicity treatment includes corticosteroids, pulmonary rehabilitation, and sometimes changing the chemotherapy. The treatment depends on the lung damage’s severity and type.
What strategies can minimize organ damage during chemotherapy?
To reduce organ damage, preventive medications and lifestyle changes are used. This includes diet, exercise, hydration, and nutritional support.
What is the importance of long-term monitoring after chemotherapy?
Long-term monitoring is key to catch and manage chemotherapy’s late effects. This includes organ damage, secondary cancers, and other complications. Follow-up plans vary based on the individual and treatment.
How can patients balance the benefits of chemotherapy with the risk of organ damage?
Patients should talk to their healthcare team about risks and benefits. This includes the type and dose of chemotherapy, health conditions, and potential organ damage. This helps make informed treatment decisions and reduce complications.
References
- Dhamija, R., Puri, S., & Datta, D. (2020). Chemotherapy-induced pulmonary complications in cancer. PMC. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7240883/






