Last Updated on October 21, 2025 by mcelik

Nearly 1 in 4 people worldwide suffer from anemia. This is a condition where you have too few red blood cells or not enough hemoglobin. While it’s often treatable, severe cases can be deadly if not treated.
Severe anemia can cause heart failure and other serious health problems. It’s important to know the risks and spot symptoms early. This can help prevent these serious issues.
Key Takeaways
- Anemia affects a significant portion of the global population.
- Severe anemia can lead to life-threatening conditions.
- Early recognition of symptoms is key for effective treatment.
- Untreated anemia can result in heart failure.
- Understanding anemia’s risks is vital for prevention.
Understanding Anemia: Definition and Basic Concepts
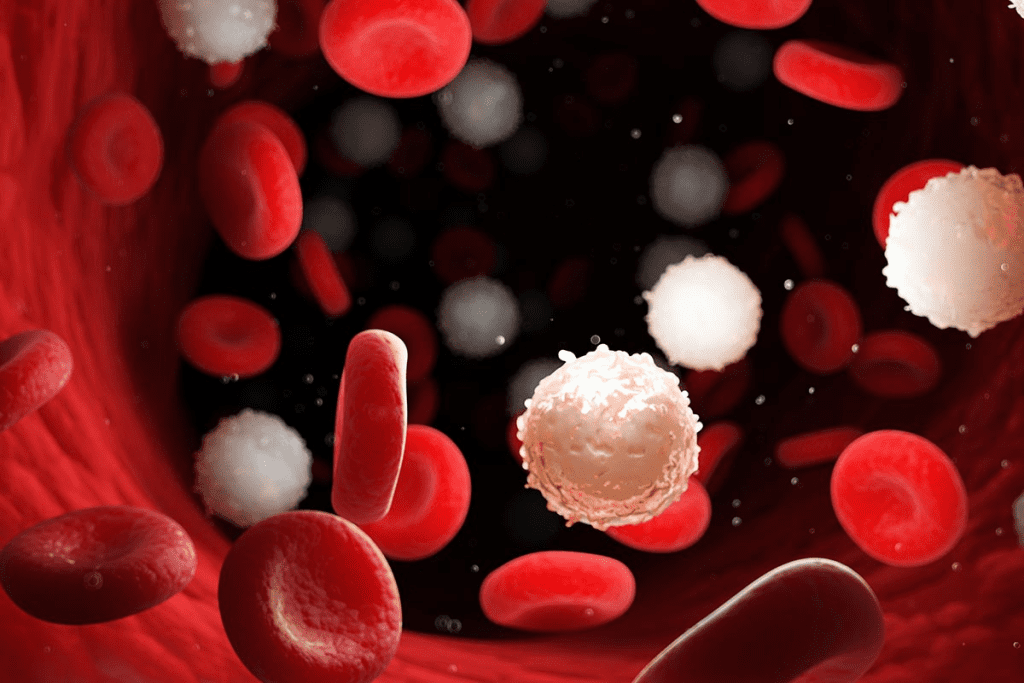
Anemia is when your body doesn’t have enough red blood cells or they don’t carry enough oxygen. Red blood cells are key for getting oxygen to all parts of your body.
What Is Anemia?
Anemia means you don’t have enough red blood cells or they’re not good enough. These cells are vital for carrying oxygen. It can happen for many reasons, like not making enough red blood cells or losing too much blood.
Key factors contributing to anemia include:
- Insufficient iron intake or absorption
- Chronic diseases
- Blood loss due to injury, surgery, or menstruation
How Blood Cells Function in the Body
Blood cells are essential for keeping you healthy. Red blood cells carry oxygen to your body’s tissues. White blood cells help fight infections. Platelets help your blood clot, stopping too much bleeding.
Normal vs. Anemic Blood Values
What’s considered normal can vary, but generally, healthy adults have certain hemoglobin levels. Men usually have levels between 13.8 and 17.2 grams per deciliter (g/dL). Women’s levels are between 12.1 and 15.1 g/dL. Anemia is when these levels are too low, showing your body can’t carry enough oxygen.
Knowing these values is key for spotting and treating anemia.
Types of Anemia and Their Severity Levels
Anemia is a term for many conditions, each with its own causes and severity. Knowing these types is key to diagnosing and treating anemia well.
Iron Deficiency Anemia
Iron deficiency anemia is the most common type. It happens when the body doesn’t have enough iron for hemoglobin. Symptoms can range from mild to severe and include fatigue, weakness, and pale skin. Mild cases might not show symptoms, while severe cases can cause serious health problems.
Hemolytic Anemia
Hemolytic anemia is when red blood cells are destroyed too fast. It can be acute or chronic and is often caused by infections, medications, or autoimmune disorders. The severity depends on how fast red blood cells are destroyed and how well the body can make new ones.
Aplastic Anemia
Aplastic anemia is a rare and serious condition where the bone marrow can’t make blood cells. This condition is considered severe and needs immediate medical help. Treatment often includes bone marrow transplantation or immunosuppressive therapy.
Sickle Cell Anemia
Sickle cell anemia is a genetic disorder that makes red blood cells sickle-shaped. This can lead to chronic anemia, pain crises, and increased risk of infections. The severity of sickle cell anemia varies, with some having mild symptoms and others facing severe issues.
Understanding the specific type and severity of anemia is critical for effective treatment. Each type of anemia has its unique challenges and needs a tailored approach to management and care.
Recognizing Anemia: Common Symptoms and Warning Signs

It’s important to know the signs of anemia to get the right medical help. Anemia happens when there’s not enough red blood cells or hemoglobin. Its symptoms can range from mild to severe.
Mild Anemia Symptoms
Mild anemia might show signs that are easy to miss. You might feel fatigue, weakness, and have pale skin. You could also get mild shortness of breath and dizziness when standing up.
Moderate Anemia Symptoms
When anemia gets worse, symptoms get stronger. You might feel increased heart rate, headaches, and have cold hands and feet. Some people might also lose hair and have brittle nails.
Severe Anemia Symptoms
Severe anemia significantly impacts your health, causing extreme fatigue and making everyday tasks difficult.. You could also have chest pain and severe shortness of breath even when sitting. In bad cases, you might faint or feel confused because your body isn’t getting enough oxygen.
Emergency Warning Signs
In very bad cases, anemia can be deadly. Look out for severe chest pain, rapid or irregular heartbeat, and severe difficulty breathing. If you see these signs, get help right away.
Knowing these symptoms helps you spot when you or someone else might need medical help fast.
Anemia Can Kill You: Understanding the Life-Threatening Potencial
Anemia is common, but it can be deadly if not treated. It happens when you have too few red blood cells or not enough hemoglobin. This can cause serious health problems if not managed well.
Acute vs. Chronic Anemia Dangers
Anemia comes in two types: acute and chronic. Acute anemia happens suddenly, often from losing a lot of blood or red blood cells being destroyed fast. It’s very dangerous because the body can’t quickly replace lost red blood cells.
Chronic anemia develops slowly, from things like not getting enough nutrients, chronic diseases, or problems with the bone marrow. It’s not as immediate a threat, but it can damage organs over time.
Hemoglobin Thresholds for Critical Concern
Hemoglobin levels show how bad anemia is. A level below 8 g/dL is very severe and needs quick medical help. But, what’s critical can change based on your health, age, and other conditions.
How Anemia Leads to Organ Failure
Severe anemia can cause organs to fail. The heart works harder to pump blood because there’s less oxygen. This can lead to heart failure. Other organs, like the kidneys and brain, also suffer from not getting enough oxygen.
- Reduced oxygen delivery to vital organs
- Increased cardiac workload leading to heart failure
- Potential for kidney damage due to chronic hypoxia
Statistical Data on Anemia-Related Mortality
Anemia is a big killer worldwide, mostly in places where healthcare is hard to get. The World Health Organization (WHO) says anemia is a big risk for death, mainly in pregnant women and kids.
| Region | Anemia Prevalence | Estimated Annual Deaths |
| Global | 24.8% | 46,000 – 62,000 |
| Low-income countries | 43.2% | 30,000 – 40,000 |
| High-income countries | 10.4% | 1,000 – 2,000 |
It’s important to know about anemia’s dangers to help reduce its impact on health worldwide. Catching it early and treating it right can lower the risk of serious problems.
Complications of Untreated Anemia
Untreated anemia can cause serious health problems. It can harm many parts of the body. This can lead to serious illness and even death.
Cardiovascular Complications
Anemia affects the heart a lot. The heart works harder because of the lack of red blood cells. This can cause heart failure and other heart problems.
- Increased heart rate and cardiac output
- Potential for heart failure
- Reduced exercise tolerance
Neurological Effects
Severe anemia can harm the brain. The brain doesn’t get enough oxygen. This can cause:
- Dizziness and lightheadedness
- Headaches
- Cognitive impairments
Immune System Impairment
Anemia weakens the immune system. People with anemia are more likely to get sick. This is a big worry for those with chronic anemia.
Pregnancy Complications
Anemia in pregnancy is very serious. It can harm both the mother and the baby. Problems include:
- Preterm labor
- Low birth weight
- Increased risk of maternal and fetal mortality
It’s very important for pregnant women to get checked for anemia. They need to be treated to avoid these problems.
When Anemia Becomes a Medical Emergency
It’s important to know when anemia is a medical emergency. Anemia is when you don’t have enough red blood cells or hemoglobin. It can become very serious if not treated right away.
Acute Blood Loss Anemia
Acute blood loss anemia happens when you lose a lot of blood quickly. This can be from injuries, surgery, or bleeding inside your body. It’s a big problem because your body can’t get enough oxygen to your organs.
- Symptoms include dizziness, fainting, rapid heartbeat, and shortness of breath.
- Immediate treatment involves stopping the bleeding, fluid resuscitation, and possibly blood transfusions.
Hemolytic Crisis
A hemolytic crisis is when your red blood cells break down too fast. This can be from infections, medicines, or your body attacking itself. It’s a serious situation because your body can’t keep up.
Key indicators include:
- Jaundice
- Dark urine
- Severe fatigue
- Shortness of breath
Severe Aplastic Anemia
Severe aplastic anemia is when your bone marrow stops making blood cells. This means you don’t have enough red blood cells, white blood cells, or platelets. It’s a serious condition that can be life-threatening.
Treatment options may include:
- Blood transfusions
- Immunosuppressive therapy
- Bone marrow transplantation
Anemia with Organ Dysfunction
Severe anemia can cause your organs to not get enough oxygen. This can lead to problems like chest pain, confusion, or not making enough urine. These are signs that something is very wrong.
In conclusion, knowing when anemia is a medical emergency is key. It helps prevent serious problems and improves treatment outcomes. Quick medical help is needed for acute blood loss anemia, hemolytic crisis, severe aplastic anemia, and anemia with organ dysfunction.
The Connection Between Anemia and Heart Failure
Anemia and heart failure are closely linked. One condition often makes the other worse. It’s important to manage both conditions well.
How Anemia Strains the Heart
Anemia makes the heart work harder. This is because there are fewer red blood cells or hemoglobin. The heart pumps more blood to get enough oxygen to the body.
This extra work can cause the heart to change shape and size. It might even lead to heart failure over time.
The heart’s response to anemia includes:
- Increased heart rate
- Enhanced cardiac output
- Potential for ventricular hypertrophy
Anemia as a Complication vs. Cause of Heart Failure
Anemia can be both a complication and a cause of heart failure. In heart failure patients, anemia can make symptoms worse. It can also lead to heart failure in people without heart problems.
Studies show treating anemia can help heart failure patients feel better. The relationship between anemia and heart failure is complex.
Cardiac Symptoms of Severe Anemia
Severe anemia can cause heart symptoms like:
- Palpitations
- Shortness of breath
- Chest pain or discomfort
- Fatigue and weakness
These symptoms happen because the heart is under a lot of stress. It’s important to recognize these symptoms early.
In conclusion, anemia and heart failure are closely related. Understanding this connection is key to effective treatment.
Anemia and Other Serious Health Conditions
Understanding anemia is key when caring for patients with serious health issues. It can impact their health outcomes. Anemia often stems from underlying diseases, making patient care more complex.
Cancer and Anemia: A Complex Relationship
Anemia is common in cancer patients, affecting their quality of life. It can also impact treatment success. Chemotherapy-induced anemia is a known side effect, where red blood cell production drops.
Chronic Kidney Disease and Anemia
Chronic kidney disease (CKD) is closely tied to anemia. As kidney function worsens, the body makes less erythropoietin. This hormone is key for red blood cell production.
Managing anemia in CKD patients is vital. It can slow kidney disease progression and improve outcomes.
- Reduced erythropoietin production
- Iron deficiency
- Chronic inflammation
These factors contribute to anemia in CKD patients.
Autoimmune Disorders and Anemia
Autoimmune diseases, like rheumatoid arthritis and lupus, can cause anemia. Chronic inflammation from these conditions affects iron and red blood cell production.
Anemia in Critical Illness
Critically ill patients often get anemia due to various reasons. These include frequent blood draws, inflammation, and poor nutrition. Anemia can worsen their condition, leading to longer hospital stays and higher mortality rates.
Managing anemia in critical illness requires a detailed plan. This includes improving nutrition, reducing blood loss, and possibly using erythropoiesis-stimulating agents.
Diagnosing Severe Anemia: Tests and Procedures
Getting a correct diagnosis for severe anemia is key. It needs a detailed approach to find the cause and how severe it is.
Complete Blood Count Analysis
A Complete Blood Count (CBC) is the main test for anemia. It checks different parts of the blood, like:
- Red Blood Cell (RBC) count
- Hemoglobin (Hb) levels
- Hematocrit (Hct)
- Mean Corpuscular Volume (MCV)
These tests show how severe and what kind of anemia you have. For example, a low MCV means microcytic anemia, and a high MCV means macrocytic anemia.
Additional Blood Tests for Anemia Causes
More blood tests are needed to find why you have anemia. These include:
- Iron studies to check for iron deficiency
- Vitamin B12 and folate levels for megaloblastic anemia
- Reticulocyte count to see how the bone marrow is doing
These tests help find the exact reason for anemia. They guide the right treatment.
Bone Marrow Testing
In some cases, bone marrow aspiration or biopsy is needed. This is for anemia types like aplastic anemia or myelodysplastic syndromes. It looks at bone marrow cells to see how they’re working.
Imaging and Other Diagnostic Procedures
Imaging studies like X-rays, CT scans, or MRI help find what’s causing anemia. This could be something like bleeding in the gut or tumors. Other tests, like a gastrointestinal endoscopy, can find where the bleeding is coming from.
By using all these tests and procedures, doctors can accurately diagnose severe anemia. They can then find the cause and plan the best treatment.
Treatment Approaches for Life-Threatening Anemia
Life-threatening anemia needs quick and effective treatment. The right treatment depends on the cause, how severe it is, and the type of anemia. Knowing the treatment options is key to managing severe anemia and avoiding complications.
Emergency Blood Transfusions
Severe anemia, caused by sudden blood loss or hemolysis, might need emergency blood transfusions. Blood transfusions quickly raise the red blood cell count. This improves oxygen delivery to important organs. The decision to give blood is based on how severe the anemia is, symptoms, and the patient’s overall health.
Iron and Vitamin Supplementation
For many anemia types, iron supplementation is a main treatment. Supplements like folate and vitamin B12 are also used if needed. The goal is to fix the deficiency, boost red blood cell production, and ease symptoms.
| Type of Supplementation | Indication | Common Dosage |
| Iron Supplements | Iron deficiency anemia | 150-200 mg/day |
| Folate Supplements | Folate deficiency anemia | 1-2 mg/day |
| Vitamin B12 Supplements | Vitamin B12 deficiency anemia | 1000 mcg/month |
Medications for Specific Anemia Types
Different anemia types need specific medicines. For example, anemia from chronic disease or chemotherapy might be treated with erythropoiesis-stimulating agents (ESAs). These agents help make more red blood cells. Hemolytic anemia might be treated with drugs that reduce the immune system’s attack on red blood cells.
Bone Marrow Transplantation
In severe cases of aplastic anemia or certain bone marrow failures, bone marrow transplantation might be an option. This involves replacing damaged bone marrow with healthy marrow from a donor. It’s a potentially life-saving treatment but carries big risks and needs careful patient selection.
Treating life-threatening anemia is complex and needs a personalized approach. Quick diagnosis and the right treatment can greatly improve outcomes for those with severe anemia.
Living with Chronic Anemia: Long-Term Management
Chronic anemia needs a detailed plan for long-term care. This plan should include medical treatment, lifestyle changes, and regular check-ups.
Monitoring Blood Values
It’s important to keep an eye on blood values to manage chronic anemia. You should track hemoglobin levels and red blood cell count. This helps make sure anemia is being well-managed.
Key tests for monitoring anemia include:
- Complete Blood Count (CBC)
- Reticulocyte count
- Iron level tests
Dietary Modifications
Changing your diet is key in managing chronic anemia. Eating more iron, vitamin B12, and folate can help reduce symptoms.
Recommended dietary adjustments include:
- Increasing consumption of red meat, poultry, and fish
- Eating more beans, lentils, and dark leafy greens
- Including vitamin C-rich foods to enhance iron absorption
Activity Adjustments and Limitations
Chronic anemia may mean you need to slow down and rest more. This helps manage fatigue and prevent symptoms from getting worse.
Pacing activities and incorporating rest periods can help manage energy levels.
Quality of Life Considerations
Chronic anemia can affect your quality of life. But with the right management, you can live a happy and active life.
Strategies for maintaining quality of life include:
- Staying connected with friends and family
- Engaging in hobbies and activities that bring joy
- Seeking support from healthcare professionals and support groups
Anemia Prevention: Reducing Your Risk
To prevent anemia, you need to make dietary changes, get regular health check-ups, and manage any health conditions. These steps can greatly lower your chance of getting anemia.
Nutritional Approaches to Prevention
Eating a balanced diet is key to avoiding anemia. Iron-rich foods like red meat, poultry, fish, beans, and fortified cereals are important. Also, foods high in vitamin C, like citrus fruits and leafy greens, help your body absorb iron better.
Having a varied diet is essential. It should include foods that prevent anemia. Some important tips are:
- Eat more iron-rich foods
- Choose foods that boost iron absorption, like vitamin C-rich foods
- Include foods high in folate, like leafy greens and legumes
- Avoid drinking tea and coffee with iron-rich foods
Regular Health Screenings
Getting regular health screenings is critical for catching anemia early. Blood tests can spot iron deficiency and other nutritional issues before they cause anemia. Doctors might suggest more tests for people at higher risk.
Managing Underlying Conditions
Some health issues, like chronic diseases, raise your risk of anemia. Taking care of these conditions through medicine and lifestyle changes can lower your risk. For example, people with chronic kidney disease might need special diets and medicines.
Special Considerations for High-Risk Groups
Pregnant women, young children, and people with certain chronic conditions are at higher risk for anemia. For these groups, it’s important to take extra steps. This might include supplements, more health tests, and careful management of their health conditions.
By knowing the risks and taking action, you can lower your chance of getting anemia. This helps keep you healthy overall.
When to Seek Medical Help for Anemia Symptoms
Knowing when to see a doctor for anemia symptoms is key. It’s important to tell the difference between symptoms that are not urgent and those that are. Anemia can show up in many ways, and knowing how serious your symptoms are is vital.
Non-Emergency Symptoms That Warrant Attention
If you’re feeling very tired, weak, or having trouble breathing, you should see your doctor. These signs might mean you have anemia. Catching it early can help manage it better.
Other signs that need a doctor’s visit include:
- Pale skin or jaundice
- Dizziness or feeling lightheaded
- Headaches or trouble focusing
- Cold hands and feet
Emergency Symptoms Requiring Immediate Care
Some symptoms are urgent and need quick medical help. If you have any of these, go to the emergency room right away:
- Severe chest pain or trouble breathing
- Severe dizziness or fainting
- Rapid heartbeat or palpitations
- Confusion or feeling disoriented
Severe anemia can be very dangerous. It means your body’s tissues and organs might not get enough oxygen. This can lead to serious health issues.
| Symptom | Non-Emergency | Emergency |
| Fatigue | Yes | No |
| Severe Chest Pain | No | Yes |
| Dizziness | Yes | Yes, if severe |
Questions to Ask Your Healthcare Provider
When talking to your doctor about anemia symptoms, it’s good to have questions ready. Ask things like:
- What is the cause of my anemia?
- What treatments are available?
- How can I manage my symptoms?
- Are there any diet changes I should make?
Being informed and taking action can greatly help with managing anemia and improving your health.
Conclusion: Understanding the Seriousness of Anemia
Anemia is a serious condition that can have big health problems if not managed well. It’s important for people to know about anemia and its dangers. This way, they can spot warning signs and get help when needed.
Anemia can lead to serious issues like organ failure and heart problems if not treated right. Knowing about anemia helps people manage it better. This can prevent severe problems.
Knowing the symptoms of anemia and when it’s a medical emergency can save lives. Being aware of anemia and its risks helps people make better health choices. This includes understanding their treatment options.
The question of whether anemia can be fatal is very important. In severe cases, yes, anemia can be deadly. It’s key to treat it quickly and effectively to avoid serious risks.
FAQ
Can anemia kill you?
Yes, anemia can be deadly if not treated. It can cause serious problems, like organ failure, if it’s severe.
Is anemia curable?
Many anemia types can be cured or managed. The success depends on the cause, severity, and treatment.
What are the symptoms of dying from anemia?
Symptoms include severe fatigue and pale skin. You might also feel short of breath, dizzy, or have chest pain. In bad cases, you could lose consciousness or organs can fail.
Can you die from low iron?
Yes, iron deficiency anemia can be serious. It can lead to heart issues, poor pregnancy outcomes, and other life-threatening problems.
How long can you live with anemia without treatment?
It varies by anemia type and severity. Mild cases might not be life-threatening right away. But, untreated anemia can cause serious health problems over time. Severe cases need immediate medical help.
Is anemia life-threatening?
Anemia itself isn’t always deadly. But, severe cases or those linked to serious health issues can be. Quick diagnosis and treatment are key to avoiding complications.
Can anemia lead to heart failure?
Yes, severe anemia can strain the heart. This can lead to heart failure. The heart works harder without enough red blood cells, causing cardiac issues.
Can anemia be a sign of cancer?
Yes, anemia can be linked to cancer. It might be caused by the disease or treatments like chemotherapy. Some cancers can lead to anemia through different ways.
What happens if anemia is left untreated?
Untreated anemia can cause many problems. These include heart and brain issues, weakened immune system, and pregnancy complications.
Is anemia treatable?
Yes, anemia can be treated. Treatment varies by cause and might include diet changes, supplements, medications, or blood transfusions.
Can you die from anemia in your sleep?
It’s rare, but severe anemia can be fatal. This includes during sleep if it’s extremely severe and untreated.
Is being anemic bad?
Being anemic can greatly affect your life quality. Severe or untreated anemia can lead to serious health issues. It’s important to get medical help and treatment.
Reference
- Lippi, G., & Mattiuzzi, C. (2020). Anemia and mortality: A systematic review and meta-analysis. Annals of Translational Medicine, 8(14), 882. https://pubmed.ncbi.nlm.nih.gov/32875064/





