Patients with Acute Myeloid Leukemia (AML) might need a bone marrow transplant to live. At Liv Hospital, we use the newest treatments for AML. We aim to give top-notch care.
Getting a stem cell transplant can feel scary. Our team is here to help you through it. We make sure you get the best care possible.
Key Takeaways
- Understanding the role of bone marrow transplants in AML treatment
- The significance of stem cell transplants in restoring blood cell production
- Overview of the transplant process and what to expect
- The importance of donor matching for successful transplants
- Advances in AML treatment and their impact on patient outcomes
Understanding Acute Myeloid Leukemia (AML) and Its Impact
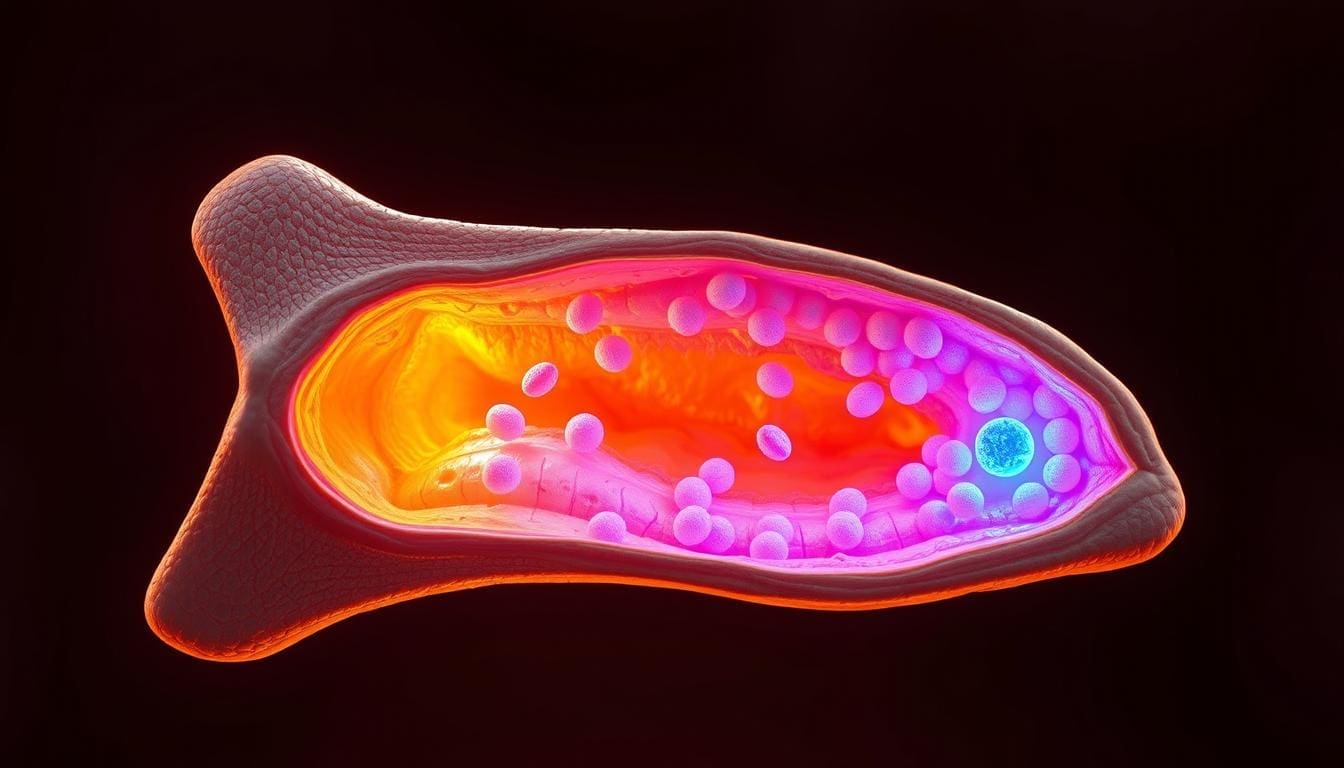
AML, or Acute Myeloid Leukemia, is a serious disease that affects the bone marrow. It stops the bone marrow from making healthy blood cells. This happens because abnormal cells grow too fast and take over the bone marrow.
What is Acute Myeloid Leukemia?
AML is a fast-growing cancer that starts in the bone marrow and spreads to the blood. It can also move to other parts of the body like the lymph nodes and liver. Unlike other types of leukemia, AML is very aggressive and needs quick treatment.
Key characteristics of AML include:
- Rapid progression
- Accumulation of malignant cells in the bone marrow
- Interference with normal blood cell production
How AML Affects Bone Marrow Function
The bone marrow makes blood cells like red and white blood cells and platelets. In AML, it makes too many immature white blood cells, or blasts. These cells can’t work right, causing problems like anemia and infections.
| Normal Bone Marrow Function | Bone Marrow Function in AML |
|---|---|
| Produces healthy red and white blood cells and platelets | Produces large numbers of immature white blood cells (blasts) |
| Supports the body’s need for blood cells | Fails to produce sufficient healthy blood cells, leading to complications |
The Need for Advanced Treatment Options
AML is a tough disease that needs strong treatments. Options like bone marrow or stem cell transplants can cure or give long-term relief. These treatments replace the bad marrow with healthy one, either from the patient or a donor.
“The development of more effective and less toxic conditioning regimens has significantly improved the outcomes of AML patients undergoing hematopoietic stem cell transplantation.”
As research gets better, AML patients have more hope. New treatments could lead to a cure for this tough disease.
Overview of AML Transplant Procedures and Their Importance
Transplantation is a key treatment for AML, giving hope for long-term remission. For those with Acute Myeloid Leukemia (AML), the idea of a transplant is both hopeful and scary.
The Role of Transplantation in AML Treatment
Allogeneic Hematopoietic Stem Cell Transplantation (Allo-HSCT) is a cure for high-risk AML patients. It replaces the patient’s sick bone marrow with healthy stem cells from a donor. This helps restore normal blood cell production.
Transplantation in AML treatment has many benefits. It kills leukemia cells and offers a graft-versus-leukemia effect. This effect can lower the chance of the disease coming back.
When Transplantation Becomes Necessary
Transplantation is needed for AML patients at high risk of relapse or with refractory disease. The choice to transplant depends on the patient’s health, leukemia type, and donor availability.
For those with high-risk AML, transplant offers a chance for a cure. It can also improve survival rates and quality of life.
High-Risk and Refractory Disease Considerations
Patients with high-risk or refractory AML face special challenges. They often need stronger conditioning before transplant to increase success chances.
| Disease Status | Transplant Considerations | Outcomes |
|---|---|---|
| High-Risk AML | Intensive conditioning regimens, careful donor selection | Improved survival rates, possible cure |
| Refractory AML | Alternative donor sources, new conditioning regimens | Better graft-versus-leukemia effect, better outcomes |
In conclusion, AML transplant procedures are vital for treating Acute Myeloid Leukemia, mainly for high-risk or refractory disease patients. Understanding transplantation’s importance helps patients and doctors make the best treatment choices.
Key Fact #1: How Bone Marrow and Stem Cell Transplants Replace Diseased Cells
Stem cell transplantation is a key treatment for AML. It replaces diseased cells with healthy ones. This is vital for Acute Myeloid Leukemia patients, as it offers a chance for a cure.
The Biological Process of Transplantation
The process of transplantation is complex. First, the patient’s diseased bone marrow is removed using chemotherapy and/or radiation. This makes room for new stem cells to grow.
After the diseased marrow is gone, the patient gets the stem cell transplant. The stem cells can come from bone marrow, blood, or umbilical cord blood. They then grow into different blood cells in the bone marrow.
Restoring Healthy Blood Cell Production
The main goal of bone marrow and stem cell transplants is to make healthy blood cells again. The new stem cells start producing blood cells like red and white blood cells, and platelets. This is key for recovery and survival.
As the new stem cells work, patients see their blood cell counts improve. This can take weeks to months. During this time, they may need blood transfusions and other care.
Graft-Versus-Leukemia Effect
Allogeneic stem cell transplantation has a big advantage: the graft-versus-leukemia (GVL) effect. The donor’s immune cells fight the remaining leukemic cells. This can lower the chance of relapse and improve survival.
Studies show the GVL effect is key to success in AML patients. A study on Liv Hospital’s website found stem cell transplantation can greatly reduce relapse and improve survival in AML patients.
“The graft-versus-leukemia effect is a powerful tool in our fight against AML, giving patients a potentially curative treatment option.” -Hematologist
| Benefits of Bone Marrow and Stem Cell Transplants | Description |
|---|---|
| Replacement of Diseased Cells | Transplantation replaces leukemic cells with healthy stem cells, potentially curing AML. |
| Restoration of Healthy Blood Cell Production | New stem cells restore normal hematopoiesis, improving blood cell counts and overall health. |
| Graft-Versus-Leukemia Effect | Donor immune cells attack remaining leukemic cells, reducing relapse risk and improving survival. |
Key Fact #2: Types of Transplants Available for AML Patients
AML patients have different transplant options. Each option has its own benefits and things to consider. The choice depends on the patient’s health, disease stage, and donor availability.
Allogeneic Hematopoietic Stem Cell Transplantation
Allogeneic hematopoietic stem cell transplantation (HSCT) is a common AML treatment. It uses stem cells from a donor, often a sibling or unrelated donor. Allogeneic HSCT can offer a graft-versus-leukemia effect, where the donor’s immune cells fight the leukemia. We’ll look into its benefits and risks more closely.
Autologous Transplantation Options
Autologous transplantation uses the patient’s own stem cells. It’s less common for AML but can be an option for those in remission. Autologous transplantation avoids graft-versus-host disease (GVHD), a serious risk of allogeneic HSCT. But, it may not offer the same graft-versus-leukemia effect as allogeneic HSCT.
Peripheral Blood vs. Bone Marrow Sources
Stem cells can come from peripheral blood or bone marrow. Peripheral blood stem cell (PBSC) donation is more common. It involves mobilizing stem cells into the bloodstream for collection. PBSC transplantation is preferred for most allogeneic transplants due to faster engraftment and lower risk of complications. Bone marrow harvest collects stem cells directly from the bone marrow under general anesthesia.
Cord Blood Transplants
Cord blood transplants use stem cells from umbilical cord blood. They’re used when an adult donor isn’t available. Cord blood transplants are readily available and have a lower GVHD risk. But, they have fewer stem cells, leading to delayed engraftment and higher infection risk.
Key Fact #3: The AML Transplant Journey from Preparation to Recovery
The path to recovery for AML patients after a transplant is complex. It involves several key stages. We’ll walk you through from the start to the long recovery phase. This way, you’ll know what to expect at every step.
Pre-Transplant Evaluation and Conditioning
Before the transplant, patients get a detailed check-up. This is to see if they’re healthy enough for the transplant. Tests check organ function, screen for infections, and evaluate their mental health.
Then, conditioning therapy starts. This may include chemotherapy and/or radiation. It kills any cancer cells left and weakens the immune system. This makes it easier for the new stem cells to take hold without being rejected.
The Transplantation Procedure
The transplant itself is when healthy stem cells are infused into the patient’s blood. This is done through an intravenous line, like a blood transfusion. The stem cells then go to the bone marrow to make new blood cells.
This process happens in a hospital. Patients might need to stay for a bit to be watched over.
Immediate Post-Transplant Care
Right after the transplant, patients are watched closely for signs of new blood cell production. This is a critical time because they’re at risk for infections and graft-versus-host disease (GVHD). They get medicines to prevent these problems.
Long-Term Recovery Timeline
Recovery times vary, but it usually takes several months to a year or more. Regular check-ups with the healthcare team are key. They help catch any late transplant effects, manage issues, and adjust medicines.
Patients also need to make lifestyle changes. This includes eating right, exercising, and avoiding infections. These steps are important for recovery.
Our team is here to offer full care and support throughout the AML transplant journey. We know the challenges and uncertainties. We’re committed to helping our patients through each stage for the best outcomes.
Key Fact #4: Success Rates and Outcomes of Leukemia Bone Marrow Transplants
Leukemia bone marrow transplants are a key treatment, with success rates depending on several factors. We’ll look at the outcomes, focusing on survival rates, what affects success, and life quality after the transplant.
Survival Statistics and Relapse Reduction
Studies show bone marrow transplants can greatly improve survival for Acute Myeloid Leukemia (AML) patients. The five-year survival rate for AML patients getting allogeneic hematopoietic stem cell transplantation is between 40% and 60%. Also, transplantation can lower the risk of relapse, a big worry for AML patients.
Recent data shows the relapse rate after transplant can be as low as 20% for patients in complete remission at transplant time. This is a big improvement over other treatments. We’ll keep watching these stats to give the most up-to-date info to patients and doctors.
Factors Affecting Transplant Success
Many things can affect how well a leukemia bone marrow transplant works. These include the patient’s age and health, the stage of leukemia at transplant time, and how well the donor and recipient match. The conditioning regimen before transplant and any health issues also matter.
We also look at the type of transplant (allogeneic vs. autologous) and the source of stem cells (bone marrow, peripheral blood, or cord blood). Each of these factors is important for predicting the patient’s chances of long-term survival.
Quality of Life After Transplantation
The quality of life after a bone marrow transplant is very important for patients and their families. While the transplant process is tough, many patients see big improvements in their life quality after. Things like graft-versus-host disease (GVHD), infection risks, and long-term side effects can affect recovery and well-being.
We stress the need for full care after transplant, including regular check-ups and support therapies. This helps patients get the best life quality possible. Knowing what to expect from leukemia bone marrow transplants helps patients make informed choices about their treatment.
Key Fact #5: Can Bone Marrow Transplant Cure Leukemia?
The idea of a “cure” with bone marrow transplants for leukemia is complex. It means different things to different people. For some, it means the disease is gone for good. But for others, it might mean the disease is controlled for a long time.
Understanding “Cure” vs. Long-Term Remission
Many times, a bone marrow transplant can lead to long-term remission. This means the disease is kept under control, and the patient might stay healthy for years. But, it’s important to know the difference between “cure” and long-term remission.
Here’s why:
- The type of leukemia affects how well the transplant works.
- Whether it’s an allogeneic or autologous transplant matters too.
- The patient’s health and how well they can handle the transplant are key.
Realistic Expectations for AML Patients
For AML patients thinking about a bone marrow transplant, it’s vital to have realistic expectations. Some might get a complete cure. Others might stay in remission for a long time or need ongoing treatment.
Research shows that many things affect how well a transplant works. These include:
- The disease’s stage at the time of transplant.
- How well the donor and recipient match.
- The patient’s overall health.
Success Stories and Case Studies
There are many success stories of patients who got long-term remission or cure after a transplant. These stories show how this treatment can change AML patients’ lives.
For example, a study in a medical journal told of a patient who stayed in remission for over five years. This shows the transplant’s power to control the disease for a long time.
As we keep improving bone marrow transplants, AML patients are living longer and healthier lives. This progress shows how important it is to keep researching and finding new ways to help these patients.
Key Fact #6: Potential Complications and Management Strategies
Going through an AML transplant means facing possible complications and finding ways to manage them. AML transplant can save lives, but it’s important to know the risks and how to handle them.
Graft-Versus-Host Disease (GVHD)
Graft-Versus-Host Disease (GVHD) is a big risk with allogeneic hematopoietic stem cell transplantation (HSCT). It happens when the donor’s immune cells attack the recipient’s body. We treat GVHD with medicines and watch the patient closely. Allogeneic stem cell transplant risks include GVHD, which can be acute or chronic.
GVHD can harm different parts of the body, like the skin, liver, and gut. Symptoms can be mild or severe, like rashes, diarrhea, and liver problems. We aim to catch GVHD early and treat it with the right plan.
| GVHD Severity | Symptoms | Management Approach |
|---|---|---|
| Mild | Skin rash, mild diarrhea | Topical steroids, supportive care |
| Moderate | Liver dysfunction, moderate diarrhea | Systemic immunosuppression |
| Severe | Severe diarrhea, liver failure | Aggressive immunosuppression, hospitalization |
Infection Risks and Immune System Recovery
Infections are a big worry after AML transplant because the immune system is weak. We use antibiotics, antifungals, and antivirals to prevent infections. Watching for signs of infection and acting fast is key.
Getting the immune system back takes time, sometimes years. We help with vaccinations and keep using medicines to prevent infections.
Organ Damage and Secondary Malignancies
Organ damage and secondary cancers are possible long-term problems after AML transplant. Damage can come from the treatment, GVHD, or infections. We keep an eye on organ function and treat any damage.
Secondary cancers are rare but can happen because of the treatment and being immunosuppressed. We follow patients closely for early detection and treatment.
Supportive Care Approaches
Supportive care is vital for managing problems after AML transplant. This includes helping with nutrition, mental health, and managing symptoms like pain and tiredness. A team of experts works together to provide full care.
By knowing the risks of AML transplant and using good management strategies, we can make patients’ lives better and improve their outcomes.
Key Fact #7: Latest Advances in Stem Cell Transplant for AML
Research is moving fast, bringing new hope for AML patients. We’re seeing big steps forward, from new ways to prepare for transplants to better care after. These changes are making a big difference.
Novel Conditioning Regimens
Old ways of preparing for transplants were too harsh. Novel conditioning regimens aim to be gentler but just as effective. For example, venetoclax combined with hypomethylating agents is showing great results in relapsed AML patients. It’s improving their chances and reducing risks.
These new methods help the graft take better, cutting down on relapse risks. Patients can handle the transplant better, leading to better survival rates.
Haploidentical Transplantation
Haploidentical transplantation is now an option for those without a perfect match. It uses a half-match donor, often a family member. Thanks to progress, it’s becoming a reliable and effective choice, opening up more donor options.
Using post-transplant cyclophosphamide has greatly reduced GVHD risks in haploidentical transplants. This has greatly improved patient results, making it a good choice for many AML patients.
Post-Transplant Maintenance Therapies
Post-transplant maintenance therapies are being looked into to stop relapse and improve long-term results. They aim to get rid of any leftover leukemia cells. Targeted and immunotherapies are being studied for their benefits.
The goal is to keep AML from coming back while keeping side effects low. Research is ongoing to find the best maintenance plans for each patient.
Reducing Transplant-Related Mortality
Lowering transplant-related death rates is key to making stem cell transplants safer for AML patients. Better care for infections and GVHD has helped lower these rates.
By improving transplant methods and care, we can make transplants safer and more effective for AML patients.
Patient Eligibility and Finding the Right Donor
The journey to an AML transplant starts with checking if a patient can get a transplant. This involves finding a good donor. It’s a detailed process with many important steps.
Determining Candidacy for Transplantation
To see if a patient can get an AML transplant, we look at their health and leukemia status. We also consider their age and any other health issues. We use the patient’s medical history, current health, and past treatments to decide.
Key factors influencing patient eligibility include:
- The stage and aggressiveness of the AML
- Response to previous treatments
- Presence of genetic mutations
- Overall physical and mental health
HLA Matching and Donor Selection
HLA (Human Leukocyte Antigen) matching is key in picking a donor for AML transplants. The HLA system helps the immune system. Matching HLA types between donor and recipient lowers the risk of complications.
The HLA matching process involves:
- Identifying possible donors in the family or through registries
- Doing HLA typing to see how well they match
- Checking the donor’s health to see if they can donate
Alternative Donor Sources
If a perfect match isn’t found, we look at other options. These include half-matched family members, cord blood, and donors from international registries.
Physical and Psychological Preparation
After finding a donor, both the patient and donor prepare for the transplant. This includes getting ready physically and emotionally. Counseling helps with the emotional side of the transplant.
By carefully checking if a patient can get a transplant and finding the right donor, we boost the chances of a successful AML transplant. Our team supports patients and their families through this complex journey.
Conclusion: The Future of AML Treatment Through Transplantation
Acute Myeloid Leukemia (AML) treatment has made big strides with bone marrow and stem cell transplants. We’ve looked at how important transplantation is in AML treatment. This includes the different transplant types and finding the right donor.
The future of AML treatment looks bright, thanks to ongoing research. Studies show that new transplant methods are helping patients live longer. These include haploidentical transplantation and new ways to prepare for transplants.
As we keep working on AML treatment, our goal is to make patients’ lives better. With transplant advancements, we’re moving towards more tailored and effective treatments for AML.
What is an AML transplant, and how does it work?
An AML transplant, also known as a bone marrow or stem cell transplant, replaces diseased bone marrow with healthy cells. It uses high-dose chemotherapy and/or radiation to kill cancer cells. Then, it infuses healthy stem cells to help the body make blood cells again.
What are the types of transplants available for AML patients?
There are two main types of transplants: allogeneic (using a donor’s stem cells) and autologous (using the patient’s own stem cells). Allogeneic transplants can be related or unrelated donor transplants, and cord blood transplants.
How does a bone marrow transplant cure leukemia?
A bone marrow transplant can cure leukemia by replacing diseased bone marrow with healthy cells. This helps eliminate cancer cells. The donor’s immune cells also attack any remaining cancer cells, helping achieve long-term remission.
What is the success rate of leukemia bone marrow transplants?
The success rate of leukemia bone marrow transplants varies. It depends on the patient’s age, disease status, and donor match. Generally, these transplants can significantly improve survival chances and quality of life for AML patients.
What are the possible complications of AML transplant?
Possible complications include graft-versus-host disease (GVHD), infection risks, organ damage, and secondary malignancies. To manage these, supportive care like immunosuppressive medications and infection prophylaxis is used.
Can leukemia be cured with bone marrow transplant?
While a bone marrow transplant can greatly improve survival and quality of life, the idea of a “cure” is complex. It depends on the disease status and patient characteristics. Long-term remission is a more realistic goal for many AML patients.
What is the role of HLA matching in finding a suitable donor?
HLA matching is key in finding a suitable donor for an allogeneic transplant. A close HLA match between donor and recipient reduces GVHD risk and improves transplant success.
What are the latest advances in stem cell transplant for AML?
Recent advances include novel conditioning regimens, haploidentical transplantation, and post-transplant maintenance therapies. These aim to make transplants more effective and safer, reducing mortality and improving outcomes.
How is patient eligibility determined for AML transplant?
Patient eligibility is determined by a thorough evaluation. This includes disease status, age, overall health, and donor availability. A team assesses these factors to decide if a transplant is suitable.
What is the process of finding a suitable donor for AML transplant?
Finding a suitable donor involves HLA typing, donor screening, and evaluating the donor’s health. If a matched related donor isn’t available, alternative sources like unrelated donors or cord blood are considered.
References
American Cancer Society. (n.d.). Stem Cell Transplant for Acute Myeloid Leukemia (AML). Retrieved from https://www.cancer.org/cancer/types/acute-myeloid-leukemia/treating/bone-marrow-stem-cell-transplant.html Cancer.org+1


