Last Updated on October 20, 2025 by
We’re here to explain blood cancer. It’s a group of cancers that affect blood cells. These cancers start in the bone marrow or lymphatic system. They mess up the normal blood functions.
The main types of blood cell cancer are leukemia, lymphoma, and myeloma. Knowing what blood cancer is helps us understand its causes and risk factors. So, what is blood cancer? It’s a complex issue with many causes that we’ll dive into.
Blood cancer, also known as hematologic cancer, is a complex condition. It affects the body’s blood cells. The abnormal growth of these cells disrupts normal blood functions.
Blood cancer is a group of diseases that affect the blood, bone marrow, and lymphatic system. It happens when there’s an abnormal production of blood cells. This can be red blood cells, white blood cells, or platelets.
Red blood cells carry oxygen, white blood cells fight infections, and platelets help with blood clotting. When these cells become cancerous, it can harm the body’s ability to perform these functions.
Blood cancer can greatly impact the body’s blood functions. For example, leukemia can cause an overproduction of abnormal white blood cells. This can lead to infections, anemia, and bleeding disorders.
Lymphoma affects the lymphatic system, which is part of the immune system. It can cause lymph nodes to swell, weakening the immune response. Myeloma, a cancer of plasma cells, can damage the kidneys and bones by producing abnormal proteins.
Blood cancer often starts in the bone marrow, where blood cells are made. The bone marrow is the spongy tissue inside some bones, like the hips and thighbones. When DNA in bone marrow cells gets damaged, cancerous cells can develop.
The lymphatic system, including lymph nodes, spleen, and lymphoid tissues, is also a common place for blood cancer to start. Lymphoma, for example, begins in the lymphatic system. Knowing where blood cancer starts helps us understand how it progresses and affects the body.
In medical terms, blood cancer is known as hematologic malignancy. This term covers different cancers that affect the blood, bone marrow, and lymphatic system. It’s important to understand these terms to grasp the complexity of blood cancer.
Hematologic malignancies start in the blood-making cells of the bone marrow or in immune system cells. They disrupt normal blood cell production, causing health problems. Knowing about these malignancies helps doctors diagnose and treat blood cancer better.
Blood cancer is divided into types based on the cells affected and the disease’s nature. The main types are leukemia, lymphoma, and myeloma. Each type needs a specific treatment plan.
The various names for blood cancers show how the disease can appear differently. For example, leukemia affects blood-making cells, lymphoma targets the lymphatic system, and myeloma impacts plasma cells. These differences help doctors tailor treatments.
| Type of Blood Cancer | Cells Affected | Description |
|---|---|---|
| Leukemia | Blood-forming cells | Cancer of the blood or bone marrow characterized by an abnormal increase of immature white blood cells. |
| Lymphoma | Lymphatic system cells | Cancer that begins in cells of the lymph system, part of our immune system. |
| Myeloma | Plasma cells | Cancer of plasma cells, a type of white blood cell present in bone marrow. |
There are three main types of blood cancer: leukemia, lymphoma, and myeloma. Each affects different parts of the blood and lymphatic system. Knowing these differences is key for the right diagnosis and treatment.
Leukemia is a blood cancer that targets the bone marrow’s blood-forming cells. It leads to the abnormal production of white blood cells, which fight infections. Leukemia has several subtypes, like ALL, AML, CLL, and CML.
Symptoms of leukemia include fatigue, weight loss, and frequent infections. You might also notice easy bruising or bleeding. Doctors use blood tests and bone marrow biopsies to diagnose it.
Lymphoma starts in the lymphatic system, a part of the immune system. It happens when lymphocytes grow out of control. There are two main types: Hodgkin lymphoma and non-Hodgkin lymphoma (NHL).
Hodgkin lymphoma is marked by Reed-Sternberg cells in lymph nodes. Non-Hodgkin lymphoma is a broader category without these cells. Symptoms include swollen lymph nodes, fever, and weight loss.
Myeloma, or multiple myeloma, is a cancer of plasma cells in the bone marrow. Plasma cells make antibodies to fight infections. In myeloma, cancerous plasma cells take over the bone marrow, pushing out healthy cells.
Symptoms of myeloma include bone pain, anemia, and kidney failure. You might also get infections more easily. Doctors use blood and urine tests, bone marrow biopsies, and imaging to diagnose it.
| Type of Blood Cancer | Cells Affected | Common Symptoms |
|---|---|---|
| Leukemia | Blood-forming cells | Fatigue, weight loss, frequent infections |
| Lymphoma | Lymphocytes | Swollen lymph nodes, fever, night sweats |
| Myeloma | Plasma cells | Bone pain, anemia, kidney failure |
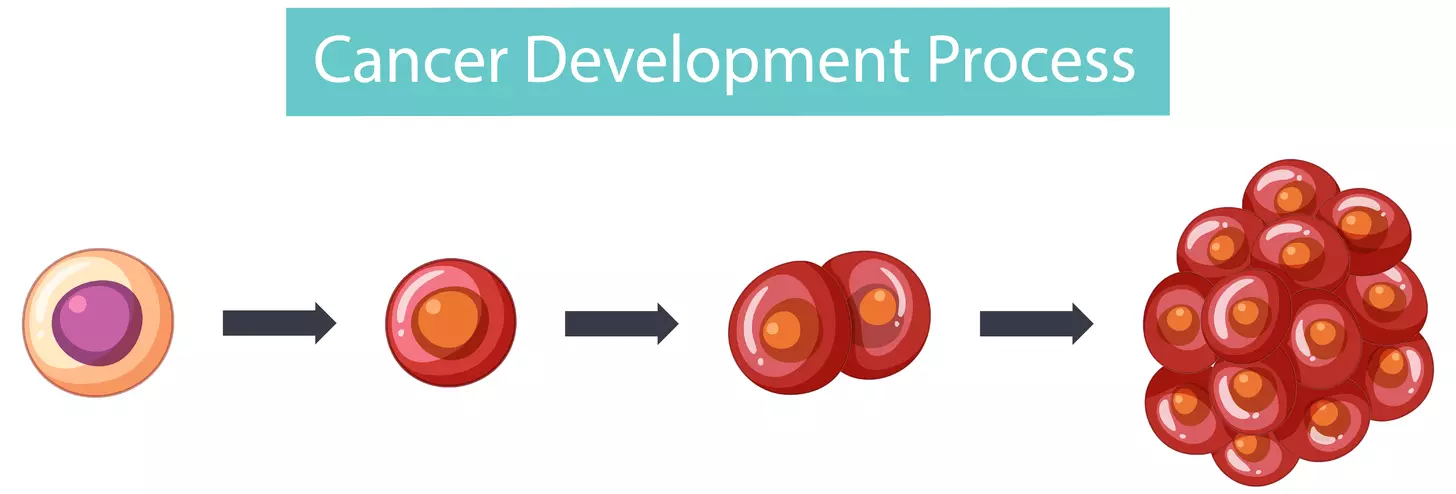
Blood cancer starts with changes at the cellular level. These changes disrupt how blood cells are made. We’ll look into how these changes happen and what drives the disease forward.
Blood cancer starts with DNA mutations in blood cells. This leads to uncontrolled cell growth. The body then can’t make blood cells right, affecting its ability to fight off infections and carry oxygen.
“It all starts with a cell that has a genetic mutation,” says, a hematologist.
“This initial mutation can be triggered by various factors, including genetic predisposition, exposure to certain chemicals, or viral infections.”
DNA mutations are key in blood cancer. They can change genes that control how cells grow and divide. This leads to abnormal blood cells that don’t work right.
In blood cancer, the bone marrow gets crowded with abnormal cells. This makes it hard for the bone marrow to make healthy blood cells. This leads to problems like anemia, infections, and bleeding disorders.
Understanding how blood cancer starts is key to finding treatments. By focusing on the disease’s causes, researchers can work on new ways to help the body make blood cells again.
Blood cancer can be caused by genetic factors. These include inherited traits and specific mutations. These elements greatly affect a person’s risk of getting blood cancer.
Some people are born with genetic mutations that make them more likely to get blood cancer. These inherited genetic predispositions can be passed down through generations. They can affect many family members.
For example, certain genetic syndromes like Li-Fraumeni syndrome and Down syndrome raise the risk of specific blood cancers.
A family history of blood cancer is a big risk factor. If a close relative has blood cancer, you might be at higher risk too.
Studies show that having a first-degree relative (like a parent or sibling) with blood cancer increases your risk. This means genetic factors in families play a part in blood cancer development.
Many genes are linked to a higher risk of blood cancer. For instance, mutations in the TP53 gene, which helps control cell division, are connected to various blood cancers.
Also, changes in genes like BRCA1 and BRCA2, which help fix DNA, can raise the risk of certain blood cancers.
Knowing about these genetic factors is key to creating targeted treatments and prevention plans for those at high risk of blood cancer.
Environmental exposures are key in determining blood cancer risk. We face many environmental factors daily. Some can greatly raise blood cancer risk.
Chemicals, like benzene, are linked to blood cancer risk. Benzene is found in petroleum, vehicle emissions, and some industrial processes.
Benzene Exposure Risks:
Ionizing radiation also raises blood cancer risk. Sources include nuclear accidents, medical procedures, and cosmic radiation.
Radiation Exposure Sources:
Some jobs increase blood cancer risk due to chemical and radiation exposure. Workers in these fields should know the risks and take precautions.
| Occupation | Hazardous Exposure | Blood Cancer Risk |
|---|---|---|
| Chemical plant workers | Benzene, other chemicals | High |
| Nuclear power plant workers | Ionizing radiation | High |
| Petroleum industry workers | Benzene, petroleum products | Moderate to High |
Knowing about these exposures can help lower blood cancer risk. People in risky jobs or exposed to harmful substances should talk to doctors. They can offer advice on how to reduce risks and monitor health.
It’s important to know how infections can lead to blood cancer. Some infections increase the risk of getting blood cancer. Research has shown how this happens.
Viral infections are a big worry for blood cancer. Human T-cell leukemia virus-1 (HTLV-1) causes adult T-cell leukemia/lymphoma, a serious blood cancer. Epstein-Barr Virus (EBV) is linked to lymphoma, including Burkitt and Hodgkin lymphoma. These viruses can change blood cells’ genes, causing cancer.
Some bacterial infections also raise blood cancer risk. Helicobacter pylori (H. pylori) infection is linked to gastric MALT lymphoma. The bacteria cause long-term inflammation, which can lead to lymphoma.
Infections can start blood cancer in different ways. Chronic inflammation from infections can make blood cells unstable. Some pathogens directly infect blood cells, changing their function and possibly causing cancer. Knowing how this happens helps us find ways to prevent and treat blood cancer.
| Infectious Agent | Type of Blood Cancer | Mechanism |
|---|---|---|
| HTLV-1 | Adult T-cell leukemia/lymphoma | Direct infection of T-cells |
| EBV | Burkitt lymphoma, Hodgkin lymphoma | Genetic alteration of B-cells |
| H. pylori | Gastric MALT lymphoma | Chronic inflammation |
Understanding how infections cause blood cancer helps us see the complex factors involved. This knowledge can guide prevention and lead to new treatments.
Blood cancer risk is linked to age and other demographic factors. Knowing these factors helps us find who’s at higher risk. It also guides us in taking steps to prevent it.
Age is a big risk factor for blood cancer. For example, chronic lymphocytic leukemia often strikes people over 60. As we get older, our cells are more likely to get damaged, leading to cancer.
Gender and ethnicity also affect blood cancer rates. Some cancers are more common in men, while others don’t show a big difference. For example, men often get certain lymphomas more than women.
There are also ethnic differences in blood cancer rates. These can be due to genetics and environment. For instance, people of European descent might face higher risks for some cancers.
Knowing these differences helps tailor prevention and screening efforts to different groups.
Where you live also affects your risk of blood cancer. Rates vary a lot around the world. This is because of lifestyle, environment, and healthcare access.
For example, industrialized countries might see more cases due to pollution. Understanding these trends helps us target public health efforts to lower blood cancer rates.
It’s important to know the early signs of blood cancer. This includes leukemia, lymphoma, and myeloma. These symptoms can be hard to spot because they often look like other illnesses.
There are common signs of blood cancer that everyone should watch out for. These include:
Blood cancer affects how blood cells are made. This can lead to anemia and bleeding problems. For example, not enough red blood cells cause fatigue. Not enough platelets can cause bleeding issues.
If you’re experiencing several of these symptoms, see a doctor. Early treatment can make a big difference.
Look for a doctor if you notice:
To diagnose blood cancer, doctors run several tests. These tests check for cancer cells in the blood or bone marrow. The process includes:
| Diagnostic Test | Purpose |
|---|---|
| Complete Blood Count (CBC) | Measures the levels of different blood cells |
| Bone Marrow Biopsy | Examines the bone marrow for cancer cells |
| Imaging Tests (CT, MRI, PET scans) | Helps determine the extent of cancer spread |
| Genetic Testing | Identifies specific genetic mutations associated with blood cancer |
These tests help figure out the type and stage of blood cancer. This information helps doctors plan the best treatment.
Understanding blood cancer’s seriousness means looking at its prognosis and survival rates. Blood cancer impacts the blood, bone marrow, or lymph nodes. The outlook depends on the cancer type, its stage, and the patient’s health.
Thanks to new treatments, survival rates for blood cancer have gone up. The 5-year survival rate for all blood cancers is about 65%. But, survival chances vary by cancer type.
For example, leukemia’s 5-year survival rate is 65%. Lymphoma’s is 72%, and myeloma’s is around 50%. Oncology departments offer detailed stats and personalized outlooks based on each patient’s situation.
Several things can change a blood cancer patient’s outlook. These include:
Knowing these factors helps doctors give a more precise outlook. They can then tailor treatments to fit each patient’s needs.
Recent years have brought big leaps in blood cancer treatment. These advances have led to better results for patients. Some of these include:
These new methods have boosted survival rates and improved life quality for blood cancer patients. As research keeps advancing, we can look forward to even better treatment results.
There are many ways to lower the risk of blood cancer. While we can’t prevent all cases, making lifestyle changes can help a lot. These changes can greatly reduce the chance of getting this disease.
People with a family history of blood cancer or those exposed to toxins need to take action. Regular health check-ups and genetic counseling are key. They help spot risks early. Also, high-risk folks might benefit from clinical trials on preventing blood cancer.
Healthy choices can lower blood cancer risk. Avoiding harmful chemicals, eating well, and staying active are important. Not smoking and drinking less alcohol also help your health and lower cancer risk.
Finding blood cancer early can lead to better treatment. Regular screening is vital for those at high risk. It includes blood tests and physical exams for signs of illness.
Knowing the early warning signs of blood cancer is also key. Look out for fatigue, weight loss, and frequent infections. These signs mean it’s time for a doctor’s visit.
By following these steps and making healthy choices, you can lower your risk of blood cancer. Keeping up with the latest research and treatments is also important.
We’ve looked into the many reasons behind blood cancer. It’s not just one thing. Instead, it’s a mix of genetics, environment, and other factors that affect blood cells.
Genetics, chemicals, radiation, and infections all play a part in blood cancer. Knowing this helps us understand who might be at risk. It also guides how we can prevent it.
By understanding blood cancer’s causes, we see how vital awareness is. This knowledge helps people take care of their health. It also encourages them to see a doctor when they need to.
Our talk shows how important research into blood cancer is. We want to find better ways to diagnose and treat it. This way, we can lessen its effects on people’s lives.
Blood cancer, also known as hematologic malignancy, is a group of cancers. They affect the blood cells and disrupt normal blood functions. It starts in the bone marrow or lymphatic system.
The main types are leukemia, lymphoma, and myeloma. Leukemia affects blood-forming cells. Lymphoma affects the lymphatic system. Myeloma affects plasma cells.
Blood cancer starts with DNA mutations in blood cell formation. These mutations can be genetic, environmental, or due to infections.
Yes, genetic factors like inherited predispositions and family history can increase risk. Specific genes also play a role.
Yes, exposure to chemicals like benzene and radiation can increase risk. Occupational hazards also play a part.
Viral and bacterial infections can trigger genetic mutations. They can also disrupt normal blood cell production.
Age is a big risk factor, with risk increasing with age. Gender and ethnic variations also affect incidence rates.
Symptoms include fatigue, weight loss, frequent infections, and swollen lymph nodes. Seek medical attention if symptoms persist or worsen.
Diagnosis involves physical exam, medical history, and tests like blood tests and bone marrow biopsy. Imaging studies are also used.
Blood cancer is serious and can be life-threatening. Survival rates vary based on type, stage, and individual factors. Treatment advances have improved outcomes.
Prevention is not guaranteed, but high-risk individuals can take steps. Avoiding certain chemicals and radiation and regular screening can help.
A healthy lifestyle can reduce risk. This includes a balanced diet, regular exercise, and avoiding smoking.
Blood cancer, also known as hematologic malignancy, is a group of cancers. They affect the blood cells and disrupt normal blood functions. It starts in the bone marrow or lymphatic system.
The main types are leukemia, lymphoma, and myeloma. Leukemia affects blood-forming cells. Lymphoma affects the lymphatic system. Myeloma affects plasma cells.
Blood cancer starts with DNA mutations in blood cell formation. These mutations can be genetic, environmental, or due to infections.
Yes, genetic factors like inherited predispositions and family history can increase risk. Specific genes also play a role.
Yes, exposure to chemicals like benzene and radiation can increase risk. Occupational hazards also play a part.
Viral and bacterial infections can trigger genetic mutations. They can also disrupt normal blood cell production.
Age is a big risk factor, with risk increasing with age. Gender and ethnic variations also affect incidence rates.
Symptoms include fatigue, weight loss, frequent infections, and swollen lymph nodes. Seek medical attention if symptoms persist or worsen.
Diagnosis involves physical exam, medical history, and tests like blood tests and bone marrow biopsy. Imaging studies are also used.
Blood cancer is serious and can be life-threatening. Survival rates vary based on type, stage, and individual factors. Treatment advances have improved outcomes.
Prevention is not guaranteed, but high-risk individuals can take steps. Avoiding certain chemicals and radiation and regular screening can help.
A healthy lifestyle can reduce risk. This includes a balanced diet, regular exercise, and avoiding smoking.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!