Last Updated on November 27, 2025 by Bilal Hasdemir
Getting a brain tumor diagnosis can feel scary. But knowing about the surgery options can help patients and their families make better choices.
At Liv Hospital, we focus on top-notch, ethical, and new care. Our skilled teams use the latest methods to safely take out tumors and help patients get better. Advanced surgical procedures, like craniotomy and small incision surgery, are used for both benign and malignant brain masses.
We’ll walk you through the steps of brain tumor removal. This way, you’ll know what to expect and why surgery is key.
Key Takeaways
- Knowing the type of brain tumor is key to picking the best surgery.
- Advanced techniques, like craniotomy and small incision surgery, are used for brain tumor removal.
- Liv Hospital is dedicated to giving high-quality, patient-focused care for brain surgery patients.
- The aim of brain tumor removal surgery is to safely remove the tumor and improve recovery.
- Our expert teams are here to support patients and their families during surgery.
Understanding Brain Tumors and Their Classification

It’s key to know if brain tumors are malignant or benign. This knowledge helps both patients and doctors. The type of tumor affects treatment plans and quality of life.
Brain tumors are abnormal cell growths in the brain. They can be cancerous (malignant) or noncancerous (benign). The tumor’s type and location guide surgery and treatment.
Types of Brain Tumors: Malignant vs. Benign
Brain tumors fall into two main types: malignant and benign. Malignant brain tumors are cancerous, grow fast, and can spread. They are dangerous. On the other hand, benign brain tumors are noncancerous, grow slower, and don’t spread. They can cause problems due to size and location.
The difference between malignant and benign tumors affects treatment. Malignant tumors need aggressive treatments like surgery, radiation, and chemotherapy. Benign tumors might be treated with surgery or watched closely, based on their characteristics and impact.
Common Locations and Their Surgical Implications
Brain tumors can happen in different parts of the brain. Their surgical implications change based on where they are. Tumors in key areas need careful planning to avoid harming important brain functions.
Tumors can be found in the cerebral hemispheres, cerebellum, and brainstem. Hemispheric tumors can affect many functions. Cerebellum tumors impact coordination and balance. Brainstem tumors can affect breathing and heart rate.
The tumor’s location affects surgery and possible risks. Advanced imaging and functional mapping help plan surgery. They check the tumor’s location and how close it is to important brain areas.
When Is Brain Tumor Removal Necessary?

Deciding if brain tumor removal surgery is needed depends on many factors. We look at the tumor’s type, size, and where it is. We also consider the patient’s health and symptoms. Each case is unique, and we decide if surgery is the best choice.
We examine the tumor’s type, size, and location. We also check the patient’s health and symptoms. Surgery is often suggested when symptoms are severe or the tumor is life-threatening.
Cases Where Surgery May Not Be Recommended
In some cases, surgery might not be the best option. For example, if the tumor is in a sensitive or hard-to-reach area, surgery could be risky. Also, patients with certain health issues or who are older might face too many risks.
Some reasons surgery might not be advised include:
- The tumor’s close proximity to critical brain structures
- The patient’s overall health and ability to recover from surgery
- The presence of multiple health issues that could complicate surgery or recovery
The Concept of Inoperable Brain Masses
Inoperable brain masses are tumors that cannot be safely removed through surgery. This could be because of their location, size, or the patient’s condition. Some tumors are inoperable because they are deeply embedded in critical brain areas or are too close to vital structures.
Determining if a brain tumor is inoperable requires advanced imaging and a team of healthcare professionals. They thoroughly evaluate the tumor and the patient’s condition.
| Factors Influencing Operability | Description | Impact on Surgery Decision |
| Tumor Location | Tumors in sensitive or hard-to-reach areas | May be considered inoperable due to risk |
| Patient’s Health | Presence of other health issues or advanced age | May complicate surgery or recovery |
| Tumor Type and Size | Malignant or large tumors | May require alternative treatments or a combination of therapies |
Preoperative Assessment and Planning
Before surgery, we do a detailed check-up to plan the best approach for brain tumor surgery. We look at every part of the patient’s health to make sure we’re ready.
Advanced Imaging Techniques
We use MRI and CT scans to plan the surgery. These tools give us clear pictures of the brain tumor and the areas around it. They help us see the tumor’s size, where it is, and how it affects the brain.
- MRI shows us the tumor’s details in soft tissues.
- CT scans tell us how the tumor affects bones.
Functional Mapping and Neuronavigation
Functional mapping and neuronavigation are key in planning the surgery. Functional MRI (fMRI) and diffusion tensor imaging (DTI) help us find important brain functions and paths. This way, we can avoid harming them during surgery.
- Neuronavigation lets us see where we are in the brain as we operate.
- This helps us remove the tumor safely and keep the brain healthy.
Multidisciplinary Tumor Board Evaluation
A team of experts reviews each case before surgery. This team includes neurosurgeons, neuro-oncologists, and radiologists. They work together to create a treatment plan that fits the patient’s needs.
- The team talks about the patient’s diagnosis, scans, and health to decide on the best surgery.
- This teamwork makes sure we consider all options and what might happen.
Patient Preparation for Brain Surgery
Getting ready for brain surgery is very important to lower risks. We know it’s scary, but being well-prepared helps a lot. It’s key to a good result.
Medical Optimization
Before surgery, we make sure the patient is as healthy as possible. We look at their medical history, current meds, and any health issues. Our team helps manage things like high blood pressure, diabetes, and heart disease.
We also tell patients to make healthy lifestyle changes. This includes stopping smoking, drinking less, and eating well. These steps help improve health and make recovery easier.
Informed Consent Process
The informed consent process is very important. We make sure patients and their families know everything about the surgery. This includes risks, benefits, and other options.
We have detailed talks with our neurosurgery team. Patients can ask questions and share any worries. Our goal is to give patients the knowledge to make good choices.
We provide all the details about what to expect during surgery and after. This helps reduce anxiety and makes patients feel supported. With careful patient preparation, we aim for the best results for our patients.
Brain Tumor Removal: Surgical Approaches
Removing brain tumors needs careful planning. The right surgery depends on the tumor’s size, location, and type. Each case is unique.
Craniotomy: The Traditional Approach
Craniotomy is a common surgery for brain tumors. It involves removing a part of the skull to reach the brain. This lets surgeons see the tumor and nearby areas clearly.
Key aspects of craniotomy include:
- Direct access to the tumor
- Ability to visualize surrounding brain structures
- Flexibility in terms of the size of the craniotomy
It’s often used for big tumors or those in hard-to-reach spots.
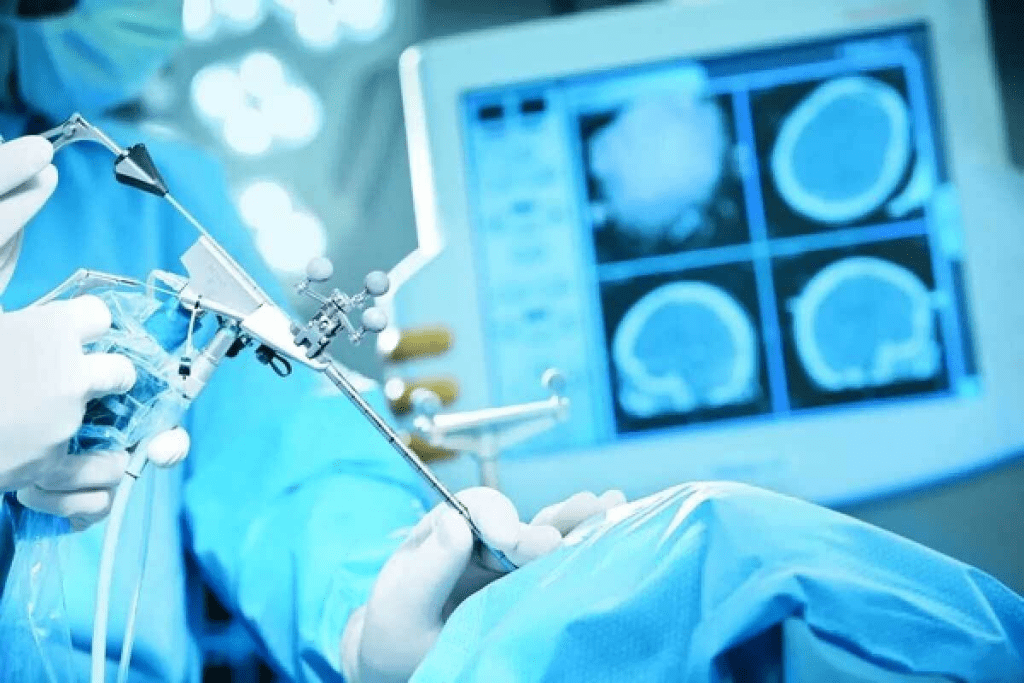
Neuroendoscopy Procedures
Neuroendoscopy uses a small endoscope to peek inside the brain. It’s great for tumors near the ventricles. This method is less invasive.
Benefits of neuroendoscopy include:
- Smaller incisions
- Less brain tissue disruption
- Potential for shorter recovery times
It can be used alone or with other surgeries.
Minimally Invasive Techniques
Minimally invasive surgeries are gaining popularity. They aim to reduce recovery time and damage to brain tissue. Advanced imaging and navigation help with these techniques.
Examples of minimally invasive techniques include:
- Keyhole surgery
- Laser-induced thermal therapy
- Stereotactic radiosurgery
In conclusion, picking the right surgery for brain tumors depends on many factors. Knowing the options is key for the best results.
Surgical Tools and Technologies in Brain Surgery
Brain surgery has seen big changes thanks to new tools and tech. These advancements help doctors remove tumors more accurately and safely. We use cutting-edge tech to improve surgery results.
Microsurgical Instruments
Microsurgical tools are key in brain surgery. They let doctors cut and remove tumors with great care. These tools are made to be very delicate, helping surgeons work on the brain’s tiny parts without harming nearby tissue.
Key Features of Microsurgical Instruments:
- High precision
- Ergonomic design for reduced fatigue
- Compatibility with advanced imaging technologies
Ultrasonic Aspiration Systems
Ultrasonic aspiration systems are a big step forward in brain surgery. They help safely take out tumors. These systems use sound waves to break down tumor tissue, which is then sucked out.
The benefits of ultrasonic aspiration include:
- Reduced risk of damage to surrounding brain tissue
- Enhanced precision in tumor removal
- Improved outcomes in complex surgical cases
Laser Ablation Technologies
Laser ablation tech is a new way to treat brain tumors. It uses laser heat to kill tumor cells while keeping healthy tissue safe. This method is less invasive, which means patients recover faster.
Advantages of Laser Ablation:
- Minimally invasive, reducing recovery time
- Precision in targeting tumor cells
- Potential for treating tumors in difficult-to-reach locations
We keep adding these advanced tools and tech to our work. This way, we make sure our patients get the best and safest care.
Intraoperative Techniques for Tumor Identification
Intraoperative techniques are key in telling the tumor from healthy brain tissue. These advanced methods help surgeons spot and understand brain tumors during surgery. This is vital for treating them well.
Fluorescence-Guided Surgery
Fluorescence-guided surgery lights up cancer cells, making it easier to see what’s normal and what’s not. A special dye is given that sticks to tumor cells. Then, under special light, these cells glow, helping surgeons remove tumors more accurately.
Intraoperative MRI and Ultrasound
Intraoperative MRI and ultrasound help check how well tumors are removed during surgery. Intraoperative MRI gives clear images to see if all the tumor is gone. Intraoperative ultrasound shows real-time images, helping spot tumor edges and important brain areas.
Distinguishing Malignant from Non-Malignant Tissue
Telling apart bad and good tissue is key in brain tumor surgery. Histopathological examination and molecular diagnostics help figure out what the tumor is. This info is key for deciding how much to remove and what to do next.
Awake Craniotomy for Functional Mapping
An awake craniotomy is used to map brain function. The patient stays awake to check brain function live. This way, we can save important brain areas and avoid damage.
In summary, methods like fluorescence-guided surgery, intraoperative MRI and ultrasound, and awake craniotomy are vital for finding and understanding tumors during surgery. They help us remove tumors safely and effectively.
Brain Tumor Resection: Achieving Maximum Safe Removal
Removing a brain tumor safely is a tricky task. It’s all about taking out the tumor without harming the brain. The main goal is to get rid of as much of the tumor as we can while keeping the brain safe.
Gross Total vs. Subtotal Resection
How much of the tumor we can remove matters a lot. Gross total resection means we try to take out as much as we can, leaving almost nothing behind. On the other hand, subtotal resection means we remove a big part of the tumor, but some might stay.
“Choosing between gross total and subtotal resection depends on many things,” says a top neurosurgeon. “Things like where the tumor is, how big it is, and how close it is to important brain parts matter. We always aim to remove as much as we can while keeping the brain working right.”
Preserving Neurological Function
Keeping the brain working right is key during surgery. We use special methods like intraoperative mapping and monitoring to find and save important brain areas. This helps lower the chance of brain problems after surgery.
Surgical Margins and Their Significance
The edges of the tumor are very important in surgery. Surgical margins are the tissue around the tumor we remove. Clear margins help prevent the tumor from coming back. But, getting clear margins can be hard because of where the tumor is.
Handling Difficult Tumor Locations
Some tumors are hard to get to because of where they are. We use special tools and methods, like neuronavigation and intraoperative imaging, to safely remove them.
By knowing how to remove brain tumors and using the latest surgical methods, we can safely take out tumors. This helps keep the brain working well.
Post-Operative Procedures and Analysis
After removing a brain tumor, we focus on post-operative care. This is key for the patient’s recovery and to learn about the tumor. It’s a critical phase.
Histological Evaluation of Brain Tumor Extracted Samples
The tumor sample is examined closely. This helps find out the tumor’s type and how aggressive it is. Histological evaluation is vital for making treatment plans.
Our team works with pathologists for accurate diagnosis. They use special techniques and molecular analysis to find markers or genetic mutations in the tumor.
Immediate Post-Surgical Care
Immediate care after surgery is essential. We watch the patient’s brain function, vital signs, and overall health. Effective pain management is also a priority to keep the patient comfortable.
- Monitoring neurological status
- Managing pain effectively
- Preventing infection
Monitoring for Complications
Patients after brain surgery face risks like infection, bleeding, and neurological problems. We use various methods to watch for these issues. This includes regular brain checks and imaging studies.
Finding complications early helps us act fast. This is important for lessening their effect on recovery.
Determining Next Steps in Treatment
The results from the tumor analysis and the patient’s health guide our next steps. This might include more surgery, radiation, chemotherapy, or a mix of these.
- Reviewing histological evaluation results
- Assessing the patient’s clinical status
- Discussing treatment options with the patient and their family
We analyze the data and the patient’s surgery response to create a personalized plan. This plan aims to meet their specific needs and improve their chances of a good outcome.
Recovery After Brain Surgery for Tumor Removal
The journey to recovery after brain tumor surgery is complex. It includes rehabilitation and managing neurological deficits. Understanding this journey and the need for tailored care is key.
Rehabilitation Strategies
Rehabilitation is vital for patients to regain strength and function after surgery. Physical therapy, occupational therapy, and speech therapy are essential. They help with mobility, cognitive issues, and communication problems.
Studies show early and intense rehabilitation is beneficial. Early mobilization can reduce complications and improve recovery. We create personalized plans for each patient’s needs and goals.
Managing Neurological Deficits
Managing neurological deficits is a key part of recovery. These deficits vary based on the tumor’s location and surgery extent. Our team uses medication, physical therapy, and cognitive rehabilitation to manage them.
For cognitive impairments, cognitive training can help. For motor deficits, physical therapy is used. Addressing these deficits early can greatly improve a patient’s life quality.
Individualized Care Pathways
Individualized care is central to effective recovery. Each patient’s journey is unique, influenced by health, tumor nature, and personal preferences. We create care plans tailored to each patient’s needs and goals.
A multidisciplinary team provides ongoing support. This team monitors progress, adjusts plans, and offers support to patients and families.
In conclusion, recovery after brain surgery for tumor removal is complex. It requires a multifaceted approach, including rehabilitation, managing deficits, and individualized care. By focusing on personalized care, we can improve outcomes and enhance patients’ lives.
Conclusion: Advances in Brain Tumor Surgery and Future Directions
Brain tumor surgery has seen big improvements. New technologies and better surgical methods have made operations safer and more precise.
New tools like fluorescence-guided surgery and intraoperative MRI have changed the game. They help doctors remove tumors more accurately, keeping brain function intact.
Research is always pushing the boundaries of brain tumor surgery. We’re looking at better imaging, smaller surgical tools, and using artificial intelligence in planning.
It’s vital to keep funding research and innovation. This will help us find even better ways to treat brain tumors. It’s all about improving patient care and quality of life.
FAQ
What is the difference between malignant and benign brain tumors?
Malignant brain tumors are cancerous and grow fast. They can spread to other brain areas. Benign brain tumors are not cancerous and grow slower. They usually have a clear boundary from the surrounding tissue.
How is the type and location of a brain tumor determined?
MRI and CT scans help find out the type and location of a brain tumor. This is key for planning surgery.
When is brain tumor removal necessary?
Removing a brain tumor is needed when it causes significant symptoms or is cancerous. It’s also needed when it presses on important brain parts. But, surgery might not be suggested if the tumor can’t be safely removed or if the risks are too high.
What is an inoperable brain mass?
An inoperable brain mass is a tumor that can’t be safely removed by surgery. This is because of its location, size, or how close it is to important brain parts.
What is the role of preoperative assessment and planning in brain tumor surgery?
Before surgery, advanced imaging and planning are done. This includes mapping brain functions and using technology to guide the surgery. A team of experts also reviews the case for a detailed plan.
How are patients prepared for brain surgery?
Patients get ready for surgery by improving their health and understanding the surgery. This includes a full check-up and teaching them about the surgery.
What are the different surgical approaches used for brain tumor removal?
There are several ways to remove a brain tumor. These include opening the skull, using tiny tools, and other methods. Each method works best for different tumors based on their location and type.
What advanced surgical tools and technologies are used in brain surgery?
Modern tools and tech include special instruments and systems that use sound waves or lasers. These help surgeons be more precise and protect the brain tissue.
How is a brain tumor identified and characterized during surgery?
During surgery, special techniques like using light to guide surgery and MRI are used. These help doctors tell if the tumor is cancerous or not.
What is the goal of brain tumor resection?
The main goal is to safely remove as much of the tumor as possible. This can be all or part of the tumor, depending on the situation. The goal is to keep the brain working well and understand the surgery’s success.
What happens after brain surgery for tumor removal?
After surgery, the tumor is checked to see what it is. Patients get care right away and are watched for any problems. This helps decide what to do next.
How do patients recover after brain surgery for tumor removal?
Recovery includes getting better through therapy and managing any brain problems. Each patient gets a plan that’s just for them to help them get better.
Can all brain tumors be removed surgically?
No, not all brain tumors can be removed by surgery. If the tumor is in a bad place or is too big, surgery might not be possible.
What is the significance of awake craniotomy in brain tumor surgery?
Awake craniotomy lets surgeons map brain functions during surgery. This helps keep important brain areas working by finding out which parts control things like speech and movement.
How does laser ablation technology work in brain tumor surgery?
Laser ablation uses heat from a laser to kill tumor cells. It’s a way to treat some brain tumors without a big surgery.
References
- Vadhavekar, N. H., et al. (2024). Advancements in imaging and neurosurgical techniques: improving brain tumor resection in the modern era. Frontiers in Neurosurgery / PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC11607568/






