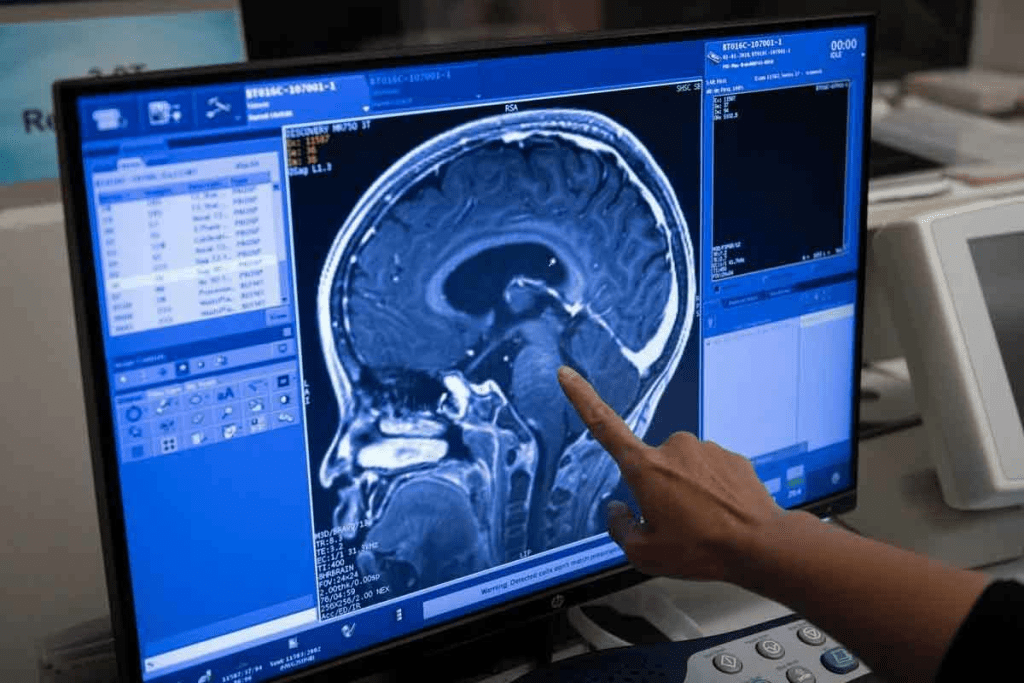
At Liv Hospital, we are dedicated to top-notch care for those with brain tumors. New targeted therapies and immunotherapies have greatly enhanced treatment choices. Drugs like temozolomide and vorasidenib are showing great promise in fighting various brain cancers.
We’re seeing a move towards more tailored and effective treatments. New drug discoveries are bringing hope for better patient results. For example, vorasidenib has been found to slow tumor growth and extend the time before tumors start growing again.
Key Takeaways
- Recent advancements in targeted therapies and immunotherapies are improving treatment options for brain tumor patients.
- Medications like temozolomide and vorasidenib are showing promise in treating different types of brain cancer.
- Vorasidenib has been shown to slow tumor growth and extend the time before the tumor starts growing again.
- New drug breakthroughs are bringing hope for better patient outcomes.
- Liv Hospital is committed to providing world-class care for patients with brain tumors.
The Current Landscape of Brain Tumor Medication

Recent breakthroughs in brain tumor treatment have brought about more effective and targeted therapies. We’re seeing a big change in how brain tumors are treated. This change focuses on precision medicine and treatment plans tailored to each patient.
Evolution of Treatment Approaches
The way we treat brain tumors has changed a lot over time. Traditional chemotherapy now works alongside newer methods like targeted therapy and immunotherapy. These new approaches have made treatments better and improved patients’ lives.
We’re moving towards more advanced treatment plans. These plans consider each patient’s tumor in detail. This includes looking at the genetic mutations that make the tumor grow. Then, we choose treatments that target those specific mutations.
Importance of Personalized Medicine
Personalized medicine is key in today’s brain tumor treatment. Tailoring treatments to each patient’s unique tumor improves results and cuts down on side effects.
The table below shows why personalized medicine is so important:
| Aspect | Description | Benefit |
| Genetic Profiling | Understanding the genetic mutations of the tumor | Identifying targeted therapy options |
| Tumor Classification | Classifying tumors based on molecular characteristics | Guiding treatment decisions |
| Tailored Treatment Plans | Creating treatment plans based on individual tumor characteristics | Improving treatment efficacy and reducing side effects |
By using personalized medicine, we can give patients with brain tumors better care. This approach is a big step forward in our fight to improve treatment outcomes for brain tumors.
The Blood-Brain Barrier: A Unique Challenge for Brain Tumor Drugs

Brain tumor treatment faces a big hurdle due to the blood-brain barrier. This barrier is a special layer that keeps the brain safe from harmful substances. It’s made up of cells and proteins that control what can get into the brain.
Structure and Function of the Blood-Brain Barrier
The blood-brain barrier is key to keeping the brain healthy. It stops harmful chemicals and tiny particles from entering the brain. But this makes it hard to get drugs to brain tumours.
The barrier’s tight structure and special proteins block most drugs. This is because it has tight connections between cells and a thick layer of proteins. It also has transporters that remove certain molecules from the brain.
Innovative Drug Delivery Technologies
Scientists are working on new ways to get drugs past the blood-brain barrier. They’re exploring:
- Nanoparticles designed to cross the blood-brain barrier
- Focused ultrasound to temporarily disrupt the barrier
- Convection-enhanced delivery to directly administer drugs into the brain
- Targeted drug delivery systems using specific ligands to cross the barrier
These methods aim to get drugs to brain tumours better. They also try to avoid harming healthy brain cells.
| Technology | Description | Potential Benefits |
| Nanoparticles | Engineered particles that can cross the blood-brain barrier | Improved drug delivery, reduced side effects |
| Focused Ultrasound | Temporary disruption of the blood-brain barrier using ultrasound | Enhanced drug penetration, non-invasive |
| Convection-Enhanced Delivery | Direct administration of drugs into the brain tissue | Bypasses the blood-brain barrier, with high local drug concentrations |
By improving these drug delivery methods, we’re making great strides. We’re finding ways to get drugs to brain tumors more effectively.
Temozolomide: The Gold Standard in Glioblastoma Treatment
Temozolomide is a key part of glioblastoma treatment. It has greatly improved how we treat this disease. Now, it’s a mainstay in treatment plans.
Mechanism of Action as a DNA Alkylating Agent
Temozolomide stops cancer cells from growing by damaging their DNA. It’s an oral drug that kills cells that grow fast, like glioblastoma cells. This helps control tumour growth.
Key aspects of temozolomide’s mechanism include:
- Inducing DNA methylation, which damages DNA and triggers cell death
- Being effective against glioblastoma due to its ability to cross the blood-brain barrier
- Causing cell cycle arrest and apoptosis in cancer cells
Stupp Protocol and Standard Dosing Regimens
The Stupp Protocol combines temozolomide with radiation therapy for glioblastoma. It has greatly improved patient results.
Standard dosing regimens typically involve:
- Concurrent temozolomide administration with radiotherapy
- Adjuvant temozolomide cycles post-radiotherapy
- Dose adjustments based on patient tolerance and MGMT status
| Treatment Phase | Temozolomide Dosage | Duration |
| Concurrent with Radiotherapy | 75 mg/m ²/day | 42 days |
| Adjuvant Phase | 150-200 mg/m ²/day | 5 days per 28-day cycle, for 6-12 cycles |
MGMT Status and Treatment Response
The MGMT gene promoter methylation status is very important. It tells us how well temozolomide will work. Patients with MGMT promoter methylation do better with temozolomide.
“The MGMT promoter methylation status is a strong predictor of the benefit from temozolomide in glioblastoma patients.” – A statement reflecting current clinical understanding.
Knowing the MGMT status helps doctors tailor treatments. It also helps predict how well a patient will respond to temozolomide.
Corticosteroids: Essential Meds for Brain Tumour Symptom Management
Corticosteroids, like dexamethasone, are key in treating brain tumor symptoms. They help reduce swelling around tumors. This makes patients feel better and live better lives.
Reducing Peritumoral Edema
Dexamethasone is great at cutting down swelling around tumors. This swelling can cause headaches, nausea, and other problems. By lessening swelling, dexamethasone helps patients feel better.
Dexamethasone works by stopping inflammation. It also helps keep fluid from leaking into the brain. This reduces swelling.
Optimal Dosing Strategies
Finding the right dose of dexamethasone is important. A high dose at first helps quickly reduce swelling. Then, the dose is slowly lowered to keep symptoms under control.
- Initial doses are often in the range of 4-8 mg per day.
- The dose is adjusted based on patient response and symptom severity.
- Tapering schedules are individualized to prevent recurrence of symptoms.
Balancing Benefits and Side Effects
Dexamethasone is very good at managing symptoms, but long-term use has downsides. These include bone loss, diabetes, and a higher risk of infections. It’s important to weigh the good against the bad.
Ways to lessen long-term side effects include:
- Use the lowest effective dose for the shortest duration necessary.
- Monitoring patients regularly for signs of side effects.
- Considering alternative treatments or adjunct therapies to reduce corticosteroid dependency.
By managing dexamethasone doses and keeping an eye on patients, doctors can make sure the benefits outweigh the risks.
Vorasidenib: Breakthrough Medicine for Brain Tumour with IDH Mutations
Vorasidenib is a big step forward in treating brain tumors with IDH mutations. It’s made to target IDH1 and IDH2 mutations, common in low-grade gliomas.
Targeting IDH1/2 Mutations in Low-Grade Gliomas
Low-grade gliomas are tough to treat because of their location and growth risk. Vorasidenib stops the IDH1 and IDH2 enzymes from growing tumors. It’s a new treatment option for those with IDH-mutant gliomas.
Recent trials show Vorasidenib slows tumor growth and improves patient outcomes.
2023 FDA Approval and Clinical Trial Results
In 2023, Vorasidenib got FDA approval for treating IDH-mutant low-grade gliomas. This was thanks to positive trial results showing it’s safe and effective.
The trials included patients with advanced or recurrent low-grade gliomas with IDH mutations. They found Vorasidenib greatly improved progression-free survival and was safe.
Patient Selection Criteria and Monitoring Requirements
To get Vorasidenib, patients must have an IDH-mutant low-grade glioma confirmed. They also need regular checks to see how they’re doing and handle side effects.
These checks include imaging studies and tests for liver function and other side effects. Doctors should also watch for signs of tumor progression or treatment resistance.
Tovorafenib: Targeted Therapy for Pediatric Brain Tumours
Tovorafenib is a big step forward in treating pediatric brain tumors. It’s a targeted therapy that aims at specific tumor characteristics. This could lead to better treatment with fewer side effects.
MAPK Pathway Inhibition Mechanism
Tovorafenib blocks the MAPK signaling pathway. This pathway is key to cancer cell growth. It targets BRAF-altered gliomas, common in kids’ brain tumors. By blocking this pathway, tovorafenib may slow or stop tumor growth.
The MAPK pathway is complex, involving many proteins. Tovorafenib targets specific mutated proteins that drive tumors. This targeted approach makes tovorafenib very promising for treating certain pediatric brain tumors.
Efficacy in BRAF-Altered Pediatric Gliomas
Clinical trials show that ovorafenib works well for BRAF-altered pediatric gliomas. It’s most effective when the tumor has a specific BRAF mutation. While results vary, tovorafenib offers significant benefits to many patients.
Research is ongoing to fully understand tovorafenib’s benefits. As we learn more, tovorafenib’s role in treating pediatric brain tumors may grow.
Pediatric Dosing and Safety Considerations
Finding the right dose of tovorafenib for kids is key. Pediatric dosing is based on age, weight, and tumor characteristics. Getting the dose right is important for effectiveness and safety.
Keeping an eye on side effects is also vital. Healthcare providers closely watch for any issues. They work with families to manage side effects and ensure the best results for young patients.
Lomustine and Carmustine: Traditional Chemotherapy for High-Grade Tumors
Lomustine and carmustine have been key treatments for high-grade brain tumours for years. They are important in fighting aggressive brain cancers, like glioblastoma.
Nitrosourea Mechanism and Cell Cycle Effects
Lomustine and carmustine are part of the nitrosourea class of alkylating agents. They work by linking DNA strands, stopping DNA replication and transcription. This action is not limited to cell division, making it effective against all cancer cells.
These drugs can cross the blood-brain barrier, which is a big plus for treating brain tumors. This ability helps them reach the tumor, making them more effective.
Gliadel Wafer Implants vs. Oral Administration
Carmustine is used in Gliadel wafers, placed in the tumor cavity during surgery. This method delivers high drug concentrations to the tumor while reducing systemic exposure.
Lomustine, on the other hand, is taken orally. The choice between these methods depends on the tumor’s characteristics, the patient’s health, and treatment goals.
Use in Recurrent Disease and Combination Regimens
Lomustine and carmustine are used for recurrent high-grade brain tumors. They are effective in this setting and are important for patients whose disease has progressed.
These drugs are also part of combination treatments with other agents and radiation. Using them together aims to improve treatment results and patient outcomes.
| Treatment Regimen | Key Components | Typical Use |
| Lomustine-based | Lomustine, temozolomide | Recurrent glioblastoma |
| Carmustine (Gliadel) Wafer | Carmustine, surgical resection | High-grade glioma, newly diagnosed or recurrent |
| Combination Therapy | Lomustine or carmustine, radiation, and other chemotherapy agents | Newly diagnosed or recurrent high-grade brain tumors |
We use these traditional chemotherapy agents carefully, considering each patient’s needs. Understanding how lomustine and carmustine work helps us offer better treatment options for high-grade brain tumors.
Bevacizumab: Anti-Angiogenic Approach to Brain Cancer Treatment
Bevacizumab is a key treatment for brain cancer. It stops tumors from growing by blocking the formation of new blood vessels. This is done by targeting vascular endothelial growth factor (VEGF), a protein that helps tumors get the blood they need to grow.
VEGF Inhibition and Reduced Tumor Vascularity
Bevacizumab works by attaching to VEGF, stopping it from reaching the cells that make new blood vessels. This stops the tumor from getting the blood it needs to grow. This is why bevacizumab is so important in fighting glioblastoma.
- Bevacizumab binds to VEGF, preventing its interaction with VEGF receptors.
- This binding inhibits the angiogenic pathway, reducing tumor vascularity.
- Reduced vascularity leads to decreased tumor growth and metastasis.
Role in Recurrent Glioblastoma Management
Bevacizumab is a big help for people with glioblastoma that comes back. When treatment fails, options are limited. Bevacizumab gives patients a new hope, helping to manage symptoms and improve life quality. Studies show it can shrink tumors and help patients live longer without their cancer getting worse.
“Bevacizumab has emerged as a standard treatment for recurrent glioblastoma, giving patients a chance at better outcomes.”
Expert Opinion
Pseudoresponse and Imaging Challenges
Bevacizumab treatment can sometimes show false signs of success on scans. This is called pseudoresponse. It happens when the tumor’s blood vessels look better on scans, even if the tumor itself isn’t getting smaller. Doctors are using new imaging methods to get a clearer picture of how well treatment is working.
- Pseudoresponse can make it hard to tell if treatment is working based on scans.
- New imaging methods are being tested to solve this problem.
- Being able to accurately measure treatment success is key to helping patients.
Can Brain Tumors Be Cured by Medicines? Treatment Limitations and Realities
Exploring brain tumor management shows that “cure” has many sides. We look at what “cure” and “control” mean, which tumors medicine works best on, and why we need many treatments.
Defining “Cure” vs. “Control” in Brain Tumor Management
In brain tumors, “cure” and “control” mean different things. A “cure” means the tumor is gone for good. “Control” means we can slow the tumor’s growth, making life better, even if it’s not gone.
It’s important to know this difference. Some patients might get a cure, while others need ongoing care to manage their tumor.
Tumor Types Most Responsive to Medical Therapy
Not all brain tumors react the same to medicine. For example, low-grade gliomas with certain genetic changes might do well with specific treatments. Tumors with IDH1/2 mutations have shown good results with drugs like Vorasidenib.
| Tumor Type | Typical Response to Medical Therapy | Common Treatment Approaches |
| Low-grade gliomas with IDH1/2 mutations | Highly responsive | Targeted therapies (e.g., Vorasidenib) |
| Glioblastoma | Variable response | Combination of surgery, radiation, and chemotherapy (e.g., Temozolomide) |
| Pediatric brain tumors with BRAF alterations | Responsive to targeted therapy | MAPK pathway inhibitors (e.g., Tovorafenib) |
The Necessity of Multimodal Treatment Approaches
Medical therapy is key in treating brain tumors, but it’s not enough alone. A mix of surgery, radiation, and medicine is often needed for the best results.
This approach lets doctors tailor treatment to each patient. They can focus on the tumor’s specific traits and the patient’s health.
Using many treatments together can lead to better outcomes. It can improve life quality and even cure some patients.
Emerging Brain Tumor Drugs and Future Directions
The future of treating brain tumors looks bright with new methods like immunotherapy and targeted therapies. As we learn more about brain tumors, we’re finding new ways to help patients. These new treatments aim to improve how we fight brain tumors.
Immunotherapy Advances: Checkpoint Inhibitors and Vaccines
Immunotherapy has changed how we treat many cancers, and it’s making a big difference in brain tumor treatment, too. Checkpoint inhibitors help the immune system fight cancer more effectively. Vaccine-based therapies also help by teaching the immune system to attack tumor cells.
One exciting area is personalized neoantigen vaccines. These vaccines are made just for a patient’s tumor. Early trials show they might offer a new hope for treatment.
Novel Targeted Therapies in Clinical Trials
Targeted therapies are key in fighting brain tumors. They aim at specific changes in the tumor that make it grow. Many novel targeted therapies are being tested in trials, giving us hope for better treatments.
Researchers are focusing on treatments for IDH mutations and BRAF alterations in brain tumors. Early trials show these treatments can shrink tumors significantly in some patients.
| Targeted Therapy | Target | Current Status |
| Vorasidenib | IDH1/2 mutations | In clinical trials |
| Tovorafenib | BRAF alterations | Approved for pediatric use |
| Other novel agents | Various molecular targets | In early-stage development |
Precision Medicine and Molecular Profiling
Precision medicine has changed how we treat brain tumors. By studying the tumor’s genes, we can find the right treatment. This approach helps us target the tumor more effectively.
Molecular profiling is a detailed study of the tumor’s genes. It helps us find the right treatment and understand why some treatments might not work. This information is key to improving treatment plans.
As we move forward, precision medicine and molecular profiling will be even more important. They help us tailor treatments to each patient, leading to better care and outcomes.
Conclusion: Navigating Brain Tumor Treatment Decisions
When dealing with brain tumors, making smart choices is key to the best results. This article talked about drugs like temozolomide and new ones like vorasidenib and tovorafenib. These medicines offer different ways to tackle brain tumors.
Choosing the right treatment for a brain tumor involves many things. These include the type of tumor, the patient’s health, and what they hope to achieve. Knowing about all the options and the latest in brain tumor drugs helps people make better decisions about their care.
Looking at all the treatment choices means understanding their good and bad sides. We need to think about the benefits of a drug and its possible side effects. We also need to see how it fits into the bigger picture of treatment.
Patients can face the tough parts of brain tumor treatment by staying up to date and working with their healthcare team. This way, they can make choices that meet their specific needs and goals.
FAQ
What are the most common medications used to treat brain tumors?
Common treatments for brain tumors include temozolomide, vorasidenib, and tovorafenib. Other drugs like lomustine, carmustine, and bevacizumab are also used. Each drug targets different types of brain tumors in unique ways.
How does temozolomide work in treating glioblastoma?
Temozolomide damages the DNA of cancer cells, stopping them from growing. It’s a key part of the Stupp Protocol for glioblastoma treatment.
What is the role of corticosteroids in managing brain tumor symptoms?
Corticosteroids, like dexamethasone, reduce swelling around tumors. They help ease symptoms by decreasing inflammation and swelling.
How does vorasidenib target IDH mutations in brain tumors?
Vorasidenib blocks mutant IDH1 and IDH2 enzymes. These enzymes are linked to some brain tumors, like low-grade gliomas with IDH mutations.
What is the significance of the blood-brain barrier in brain tumor treatment?
The blood-brain barrier limits what can enter the brain. This barrier makes it hard to treat brain tumors effectively. Researchers are working on new ways to get drugs past this barrier.
Can brain tumors be cured by medicines alone?
Medicines are key in treating brain tumors, but curing them is rare. Treatment success depends on the tumor type and grade. Often, a combination of surgery, radiation, and chemotherapy is needed.
What are the emerging trends in brain tumor treatment?
New trends include immunotherapy and targeted therapies in trials. Precision medicine and molecular profiling are also growing in importance for treatment planning.
How is bevacizumab used in managing recurrent glioblastoma?
Bevacizumab blocks VEGF, slowing tumor growth. It’s used for recurrent glioblastoma, but measuring its success can be tricky due to pseudoresponse.
What is the importance of MGMT status in temozolomide treatment?
MGMT status helps predict how well temozolomide will work. Patients with MGMT promoter methylation tend to respond better to temozolomide. This makes MGMT status a key factor in treatment planning.
How does tovorafenib work in treating pediatric brain tumours?
Tovorafenib targets the MAPK pathway, often altered in pediatric gliomas. It’s effective against BRAF-altered pediatric gliomas.
References
- U.S. Food and Drug Administration. (2025, August 6). FDA grants accelerated approval to dordaviprone for diffuse midline glioma. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-dordaviprone-diffuse-midline-glioma