At Liv Hospital, we’re dedicated to improving medical research and patient care. Embryonic stem cells (ESCs) are key in our studies. They come from the inner cell mass of a blastocyst. These cells can grow into all three germ layers of an embryo.
Recent studies show ESCs’ big role in regenerative medicine and tissue engineering. They offer new ways to treat diseases. By learning more about ESCs, we can find new treatments for many health issues.
We’re working hard to use ESCs to better human health. We think studying these cells can lead to new medical treatments. This could greatly improve how we care for patients.
Embryonic stem cells are at the center of developmental biology. They are undifferentiated cells that can form all three germ layers”ectoderm, endoderm, and mesoderm. This makes them key for research in developmental biology and regenerative medicine.
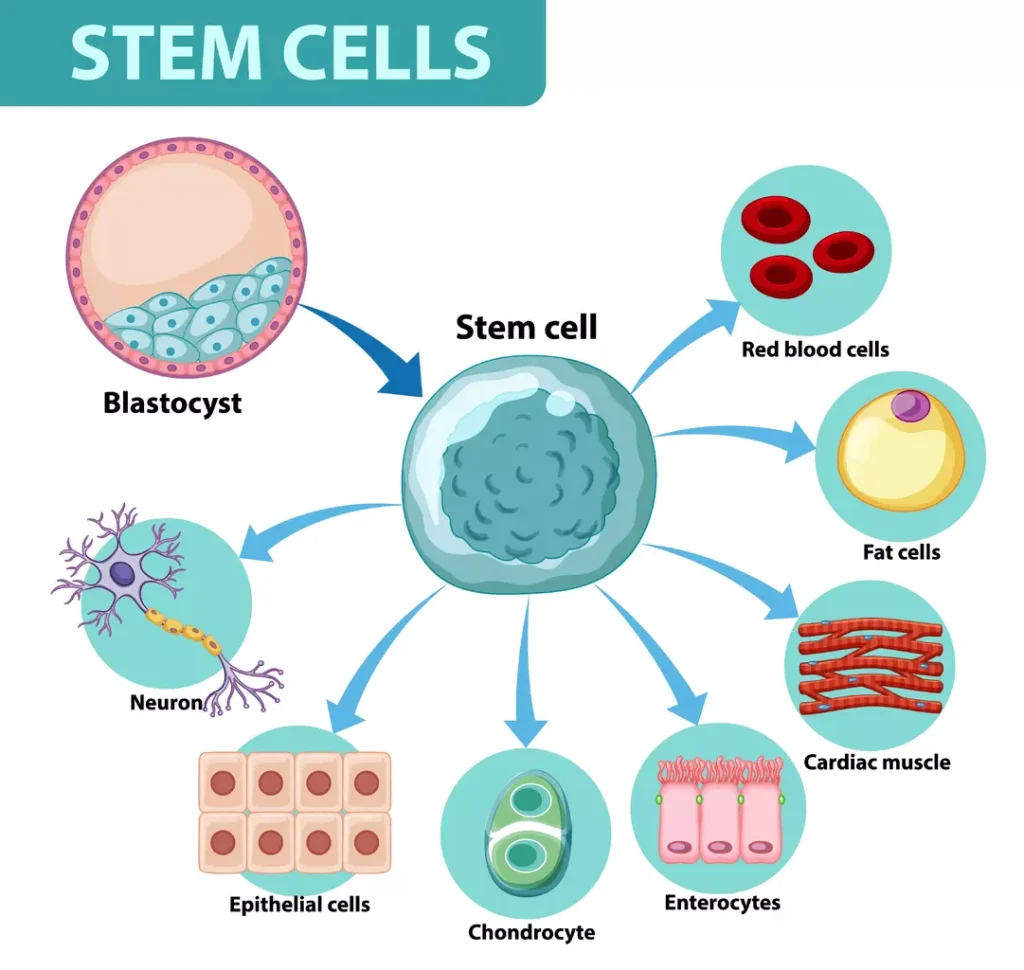
ESCs have pluripotency, which means they can turn into any cell type in the body. This is different from multipotent stem cells, which can only become a few cell types.
Martin Evans, a Nobel laureate, said, “The discovery of embryonic stem cells has opened up new avenues for understanding development and for the treatment of diseases.” This shows how important ESCs are for research and possible treatments.
The discovery of ESCs in the early 1980s was a big step in stem cell research. Scientists found and grew ESCs from mouse embryos. They showed they could renew themselves and turn into different cell types.
This breakthrough helped us understand human embryonic development better. It also opened doors for research in regenerative medicine. Studying ESCs in the lab has given us insights into how we develop and how diseases work.
Embryonic Stem Cells (ESCs) come from the blastocyst stage, about 4“7 days after fertilization. At this time, the embryo is called a blastocyst. It has two main parts: the outer trophoblast layer and the inner cell mass (ICM).
The blastocyst stage is a critical time for the embryo. It prepares for implantation in the uterus. The blastocyst has a fluid-filled cavity (blastocoel) and is surrounded by the trophoblast and the ICM. The ICM is key because it forms the embryoblast, which will become the fetus.
ESCs come from the inner cell mass of the blastocyst. To get these cells, scientists use dissection and culturing techniques. These cells can become any cell type in the body, making them very useful for research and possible treatments.
Getting ESCs involves careful thought about ethics and technique. The process must respect ethical standards and focus on the technical aspects to keep the cells viable and of high quality.
Understanding where ESCs come from and how they are obtained helps us see their value in medical research and therapy.
Embryonic stem cells (ESCs) come from the early stages of a developing embryo. They are special because they can grow into any cell type in the body. They also keep growing without stopping.
Pluripotency means a cell can turn into any cell type in the body. ESCs are pluripotent, so they can become any of the three main cell layers: ectoderm, mesoderm, and endoderm. This makes them very useful for studying how cells develop and for possible treatments.
The reason ESCs can do this is because of special proteins and signals. Oct4, Sox2, and Nanog are key players in keeping them in this state.
ESCs can also keep growing themselves. This means they can keep dividing to make more of themselves. This lets them grow endlessly in a lab, giving scientists a constant supply of cells for study and possible treatments.
To keep growing, ESCs need certain conditions. These include growth factors like leukemia inhibitory factor (LIF).
ESCs are different from adult stem cells (ASCs) in many ways. While ASCs can only turn into a few cell types, ESCs can become any cell type. This makes ESCs much more versatile.
These differences highlight why ESCs are so valuable in research and for regenerative medicine.
Embryonic stem cells can turn into the three main germ layers. This is key to human growth, as it leads to all body tissues and organs. We’ll see how these stem cells become the ectoderm, mesoderm, and endoderm layers.
The ectoderm is a primary germ layer in embryonic development. It forms the brain, spinal cord, and peripheral nervous system. It also creates the skin, hair, and nails.
Ectodermal Derivatives
The mesoderm is vital for developing connective tissues. It turns into muscles, bones, and the circulatory system. This includes the heart and blood vessels. It also forms the urogenital system and the adrenal cortex.
| Mesodermal Derivatives | Examples |
|---|---|
| Musculoskeletal System | Muscles, bones, cartilage |
| Circulatory System | Heart, blood vessels |
| Urogenital System | Kidneys, reproductive organs |
The endoderm is the innermost germ layer. It lines various bodily systems. It forms the digestive system, including the liver and pancreas, and the respiratory system. It also lines the bladder and urethra.
Endodermal Derivatives
Donations from IVF clinics are key for getting human embryonic stem cells for research. These donations help us learn more about human development and diseases.
Many human embryonic stem cells come from IVF clinics. These clinics often have extra embryos not used for fertility treatments. With consent, these embryos can be donated for research.
We value IVF clinic donations for stem cell research. The process follows strict ethical rules to make sure donations are made with full consent.
There are strict rules for getting human embryonic stem cells. These rules ensure the process is done right and with respect for donors. They vary by country but include informed consent and no financial rewards.
We follow strict ethical standards for getting these stem cells. This means donors know how their embryos will be used and give consent freely.
| Ethical Consideration | Description |
|---|---|
| Informed Consent | Donors must be fully aware of how their embryos will be used in research. |
| Donor Autonomy | Donors have the right to make decisions about their embryos without external pressure. |
| Prohibition of Financial Inducements | Donors must not be offered financial incentives for donating their embryos. |
Researchers are also looking into other ways to get human embryonic stem cells. One method is using induced pluripotent stem cells (iPSCs). These are made by changing adult cells to act like embryonic cells.
We’re looking into iPSCs as a possible alternative. This could help solve some of the ethical issues with using embryos in research. It could also give us important insights into human biology and disease.
Embryonic stem cells can turn into many types of cells. This makes them key for new treatments and understanding human growth. They are used in many ways, like studying human development and creating new therapies.
Embryonic stem cells give us a peek into early human growth. By studying them, we learn about how tissues form and how embryos grow. This helps us understand developmental issues and find new treatments.
Studies show these cells can mimic early human growth in labs. This lets us see how genes and environment affect growth. For example, they help us study the human nervous system and find causes of brain disorders.
Embryonic stem cells are also used for disease modeling and drug testing. By turning them into specific cells, researchers create disease models. These models help study diseases, test drugs, and develop personalized treatments.
For instance, they’ve been used for diseases like Parkinson’s and ALS. These models help find new treatments and test their effectiveness.
| Disease | Cell Type Modeled | Research Applications |
|---|---|---|
| Parkinson’s Disease | Dopaminergic Neurons | Disease modeling, drug testing, cell replacement therapy |
| ALS | Motor Neurons | Disease modeling, drug testing, understanding disease mechanisms |
| Diabetes | Pancreatic Beta Cells | Disease modeling, drug testing, cell replacement therapy |
Embryonic stem cells are promising for regenerative medicine. They can become many cell types, making them great for repairing damaged tissues. Researchers are looking into using them for heart disease, diabetes, and spinal cord injuries.
Studies show they can fix heart tissue and improve heart function. They’re also being explored for treating type 1 diabetes.
While there are challenges, the possibilities for regenerative medicine are huge. Research is ongoing to solve technical and ethical issues. This could lead to new treatments.
Embryonic stem cell research faces many hurdles, from technical issues to ethical debates. This field is complex, and several challenges must be overcome to fully benefit from it.
One big challenge is the technical and scientific hurdles in this research. Directed differentiation of stem cells into specific types is hard. Even with progress, the success rate and precision of these methods are not perfect, and there’s a risk of teratoma formation.
Keeping stem cells in a state where they can grow and renew themselves is also tricky. The conditions needed for this are complex. The lack of standard methods across labs makes things even harder.
Ethical debates are a big part of the controversy around using human embryos in research. The ethical debate revolves around the moral status of embryos and the balance between research benefits and human life respect.
It’s important to follow ethical guidelines and regulations for using embryonic stem cells. Getting consent from donors and respecting their choices are key. Ethical rules vary worldwide, showing different cultural and societal views.
Regulations for embryonic stem cell research vary greatly between countries. Regulatory variability impacts funding, research scope, and ethical standards.
In some places, rules are strict, while others are more open. This means researchers must know and follow the laws of their country and any international partners.
To move forward, we need to talk more among researchers, policymakers, and the public. This will help tackle the ethical, scientific, and regulatory issues in embryonic stem cell research.
Research is moving fast, showing how embryonic stem cells can change medicine. We’re on the edge of a new medical era. ESCs’ unique traits will lead to new treatments.
Embryonic stem cells are promising for many medical uses. They can turn into any cell type, making them great for fixing damaged cells. This could help with Parkinson’s, diabetes, and heart disease. Different stem cells are being studied, but ESCs are leading because they can do more.
Using ESCs in medicine is just starting, but it’s showing promise. Scientists are working hard to solve the technical and ethical issues. As these problems are solved, we’ll see more ESC treatments in trials.
Combining ESCs with gene editing, like CRISPR/Cas9, opens new ways to treat genetic diseases. Scientists can fix genes in ESCs to prevent disease. This boosts ESCs’ power and helps us understand diseases better.
Gene editing in ESCs lets us make disease models for testing drugs and learning about diseases. This mix of ESCs and gene editing is key to making medicine more personal.
Embryonic stem cells are huge for personalized medicine. Using a patient’s cells to make ESCs means treatments can be made just for them. This reduces the chance of rejection and makes treatments work better.
Improvements in epigenetic reprogramming and gene editing are key for personalized medicine with ESCs. As these areas get better, we’ll see big advances in disease treatment.
In summary, the future of embryonic stem cells in medicine looks bright. We’re seeing new uses, working with gene editing, and moving towards personalized treatments. As research keeps going, we’ll see new therapies that will change medicine and help patients.
Our look into embryonic stem cells (ESCs) shows their key role in medical science. These cells can turn into many types, making them very useful for research and treatments.
Recent studies show how important ESCs are. They help us understand human growth, mimic diseases, and find new treatments. The possibilities for using ESCs in regenerative medicine are huge.
In summary, studying ESCs is vital for medical progress. As we learn more about ESCs, we get closer to finding new treatments. This makes ESCs very important for improving human health.
Embryonic stem cells (ESCs) come from the inner cell mass of a blastocyst. This is an early stage in embryonic development. They can turn into any cell type in the body.
This research studies ESCs. It looks at their properties and how they can be used in medicine and biology.
ESCs are in the inner cell mass of a blastocyst. This happens about 5-6 days after fertilization.
They are usually taken from blastocysts from IVF clinics. Donors give consent for this.
This research could change how we understand human development and disease. It could lead to new treatments for many conditions.
ESCs can become any cell type, renew themselves, and are pluripotent.
They turn into the three germ layers: ectoderm, mesoderm, and endoderm. These layers then form various cell types and tissues.
Using human embryos for research is a big ethical issue. Rules are in place to make sure this research is done right.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!