Last Updated on October 27, 2025 by
It’s key to know the difference between embryonic stem cells and adult stem cells for better medicine and new treatments. At Liv Hospital, we focus on this because we care about our patients and learning more. We want to help people get better.
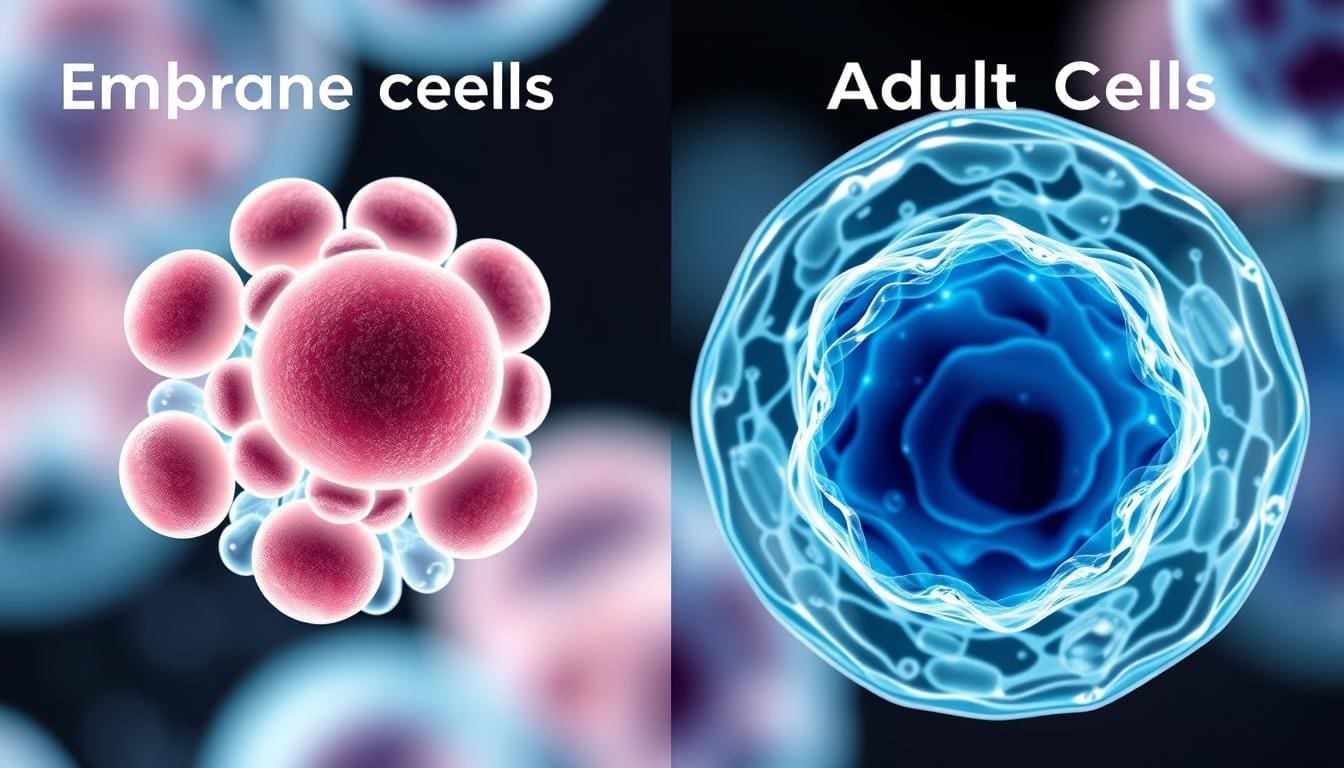
Embryonic stem cells can turn into almost any cell in our body. On the other hand, adult stem cells can only become specific cells in their own tissue. This big difference shows how they can help us in different ways.
Stem cells are at the core of biology, known for their ability to self-renew and differentiate. These traits are key for growth and repair. They can turn into different cell types, helping to keep tissues healthy and regenerating them when needed.
Stem cells are special because they can self-renew and differentiate into various cell types. This makes them vital for growth, keeping tissues healthy, and fixing them when damaged. They can keep their numbers up through self-renewal and turn into specialized cells for specific tasks.
Stem cells are defined by their ability to:
The self-renewal and differentiation of stem cells are controlled by both inside and outside factors. Self-renewal lets stem cells divide to make more of themselves, keeping their numbers steady. This is key for their long-term survival.
Differentiation is when stem cells turn into specialized cells. This is vital for tissue growth and upkeep. The right balance between self-renewal and differentiation is important for healthy tissues and preventing diseases like cancer.
“The balance between self-renewal and differentiation is critical for maintaining tissue health and preventing disease.”
Embryonic and adult stem cells differ in their ability to develop into different cell types. Embryonic cells can become any cell type, while adult cells have more limited options. Knowing these differences is important for understanding the unique roles of each type of stem cell.
Understanding embryonic stem cells is key to medical progress. These cells come from the blastocyst stage of embryos, about 3 to 5 days old. They are pluripotent, which means they can turn into almost any cell in the body. This makes them very useful for research and possible treatments.
To get embryonic stem cells, scientists take the inner cell mass from blastocyst embryos. This is a critical step because the inner cell mass becomes the fetus. The outer layer forms the placenta and other tissues. The process needs careful handling to keep the stem cells viable and pluripotent.
Embryonic stem cells can become many different cell types, like nerve and muscle cells. This is both a benefit and a challenge. It’s important to control how these cells develop for treatments. Scientists are working on ways to guide their development into specific cells for healing.
In labs, embryonic stem cells grow under special conditions to keep them pluripotent. They need certain growth factors and media to self-renew and differentiate. Knowing how these cells grow is key for making more for research and treatments.
| Characteristics | Embryonic Stem Cells |
|---|---|
| Origin | Blastocyst stage embryos |
| Pluripotency | Can differentiate into nearly any cell type |
| Growth in Laboratory | Requires specific growth factors and culture conditions |
The human body has adult stem cells in different places. They help repair and keep tissues healthy. This is key for our body’s repair and upkeep.
Adult stem cells are found in places like bone marrow, fat tissue, and the gut lining. They live in special spots called niches. These spots give them the support and signals they need to work right. For example, adult stem cells in bone marrow are vital for making blood cells.
Adult stem cells are not as versatile as embryonic stem cells. They can only turn into certain cell types. For example:
This limited ability is both good and bad. It means they can’t make cells they shouldn’t, but it also limits their uses.
Adult stem cells can renew themselves, which is important for keeping their numbers up. But, aging can slow this down. Things like damage to DNA and changes in how genes work can hurt their ability to renew.
Knowing about adult stem cells helps us understand how they keep our bodies healthy. Their special places, limited abilities, and renewal powers all play a part in their role in healing and repair.
It’s important to know the differences between embryonic and adult stem cells. This knowledge helps us move forward in stem cell research and its uses. We’ll look at their differences in how they can change into different cells, how they are found and grown, and their genetic and epigenetic makeup.
Embryonic stem cells can turn into any cell type in the body. They are pluripotent. Adult stem cells, on the other hand, can only turn into specific cell types related to their tissue of origin. They are multipotent.
This difference affects how they can be used in medicine. Embryonic stem cells can make many cell types for replacing damaged tissues. Adult stem cells are better at fixing damaged tissues within their own lineage.
Getting and growing embryonic and adult stem cells is different. Embryonic stem cells come from early-stage embryos and need special care to stay pluripotent. Adult stem cells are found in tissues like bone marrow and need different conditions to grow.
These differences make it hard for researchers. Keeping embryonic stem cells pluripotent in the lab is tough. Adult stem cells may not grow much, making it hard to get enough for treatments.
Embryonic and adult stem cells also have genetic and epigenetic differences. These affect how they work and what they can do. Embryonic stem cells have an open structure that lets them change genes easily. Adult stem cells have restrictions that limit their changes.
These differences are key to understanding stem cells. They help us figure out how to use them for treatments.
| Characteristics | Embryonic Stem Cells | Adult Stem Cells |
|---|---|---|
| Differentiation Ability | Pluripotent | Multipotent |
| Isolation Source | Blastocyst-stage embryos | Various adult tissues |
| Cultivation Requirements | Specialized culture conditions | Tissue-specific growth factors |
Cellular potency covers a wide range of abilities. It goes from making a complete organism to becoming just one cell type. This range helps us understand what different stem cells can do.
Cellular potency has levels like totipotency, pluripotency, multipotency, and unipotency. Totipotency means a cell can make a whole organism, like the zygote and early cells in an embryo. As cells grow, they become pluripotent, able to turn into almost any cell, but not a complete organism.
Multipotency is when cells can turn into several cell types, but only in a certain lineage or tissue. For example, blood-making stem cells are multipotent, creating different blood cells. At the end, unipotency means a cell can only become one type of cell.
As cells move from totipotency to unipotency, they face big developmental limits. This is because they commit to specific paths, limiting their options. This choice is influenced by genes and how genes are turned on or off.
“The process of cellular differentiation is like a branching tree. Each choice narrows down the paths a cell can take, leading to the many cell types in our bodies.”
Knowing about these limits is key for stem cell research and use. It helps us see how stem cells can help in medicine and how to guide them for specific treatments.
Recent breakthroughs in reprogramming adult cells have opened new doors for treatments. Induced pluripotent stem cells (iPSCs) are made by turning adult cells into a state similar to embryonic stem cells. This has changed the game in stem cell research, making it a key tool for regenerative medicine and more.
Reprogramming involves adding special genes to adult cells to make them pluripotent. Shinya Yamanaka and his team first showed this was possible with four key genes: Oct4, Sox2, Klf4, and c-Myc.
This breakthrough means we can make iPSCs from a patient’s own cells. This could lead to endless possibilities for fixing damaged tissues.
iPSCs can turn into many cell types like embryonic stem cells. But, they’re made from adult cells, not embryos. This makes them a better choice for avoiding ethical debates.
| Characteristics | iPSCs | Embryonic Stem Cells | Adult Stem Cells |
|---|---|---|---|
| Source | Reprogrammed somatic cells | Derived from embryos | Found in adult tissues |
| Pluripotency | Yes | Yes | No (multipotent) |
| Ethical Concerns | No | Yes | No |
iPSCs are great for personalized treatments and more. But, they also come with challenges like the risk of tumors and changes in gene expression. More research is needed to make them safer and more efficient.
Advantages: Personalized medicine, disease modeling, drug discovery, and potentially unlimited cell source.
Limitations: Risk of teratoma formation, epigenetic changes, and variable reprogramming efficiency.
Embryonic stem cells are a big step forward in medical research. They are making great progress in treating many diseases. This is thanks to ongoing clinical trials and research.
These cells are being tested for regenerative medicine. Many trials are looking at their use for macular degeneration, Parkinson’s disease, and diabetes. This is to see if they are safe and work well.
At Liv Hospital, we keep up with the latest research. We want to give the best care to patients from all over. Our team is always looking for new ways to use embryonic stem cells.
Embryonic stem cells are also great for studying diseases and finding new drugs. They can turn into different cell types. This helps scientists understand diseases better and find new treatments.
They are also useful in finding new medicines. By testing many compounds at once, they can find drugs faster and cheaper.
| Disease | Cell Type | Potential Therapy |
|---|---|---|
| Parkinson’s Disease | Dopaminergic Neurons | Cell Replacement Therapy |
| Diabetes | Pancreatic Beta Cells | Insulin Replacement |
| Macular Degeneration | Retinal Pigment Epithelial Cells | Cell Therapy for Vision Restoration |
There are big challenges before these therapies can be used in hospitals. We need to make sure they are safe and work well. We also have to deal with immune rejection and make them on a large scale.
We know these challenges and are working hard to solve them. Our goal is to bring new treatments to patients. This will help them live better lives.
Adult stem cells are changing medicine. They can turn into many cell types, making them useful in treatments. But, they are not as versatile as embryonic stem cells.
Adult stem cells are key in treating blood cancers and disorders. Hematopoietic stem cell transplantation is a main treatment for leukemia, lymphoma, and multiple myeloma. It uses stem cells to make new blood cells.
The process of hematopoietic stem cell transplantation includes several key steps:
Adult stem cells are also being looked at for regenerative medicine. This field aims to fix or replace damaged tissues and organs. Mesenchymal stem cells are being studied for their role in fixing heart disease, diabetes, and bone injuries.
Regenerative medicine could help with:
Choosing between autologous (patient’s own cells) or allogeneic (donor cells) stem cells is important. Autologous cells avoid immune rejection but might not be available in all cases. Allogeneic cells are always ready but can cause graft-versus-host disease.
The decision depends on the patient’s health, the disease, and donor availability.
Stem cell research brings up big ethical and regulatory issues. The use of embryonic stem cells is a big debate worldwide.
Embryonic stem cell research is a big ethical debate. It’s because these cells come from embryos. This has started a global talk on the moral side of using human embryos for science. The ethical sides are many, like consent, the value of human life, and balancing science with morals.
Some say the benefits of this research, like new treatments, are worth it. Others think it’s wrong to destroy embryos for science. This shows we need a careful way to handle embryonic stem cell research.
Stem cell research rules change a lot from country to country. Some places let it go more, while others limit it a lot or ban it. Knowing these rules is key for scientists and.
These rules affect research, treatments, and how scientists work together worldwide. Experts say, “The ethical and regulatory issues with embryonic stem cells show we need to keep talking and working together.”
“The ethical and regulatory challenges surrounding embryonic stem cell research underscore the need for ongoing dialogue and cooperation among stakeholders to navigate this complex landscape.”
In short, the ethics and rules of stem cell research, like with embryonic stem cells, are very complex. We need a fair way to deal with these issues. It must look at both the science and the ethics.
Stem cell research is moving forward, leading to new treatments and personalized medicine. New technologies and methods will shape this field. They promise to improve patient care.
New technologies like gene editing and biomaterials are changing stem cell research. Gene editing technologies like CRISPR/Cas9 allow for precise changes to stem cells. This boosts their healing power. Biomaterials are also being used to improve how stem cells are delivered and engineered into tissues.
Personalized medicine will greatly benefit from stem cell research. Induced pluripotent stem cells (iPSCs) help create models for studying diseases and testing drugs. Bioengineering is also advancing, aiming to create artificial organs and tissues. This could change regenerative medicine forever.
As we look ahead, stem cell research, new technologies, and bioengineering will change healthcare. We’re dedicated to pushing these areas forward. Our goal is to bring innovative, patient-focused solutions to healthcare.
Understanding the differences between embryonic and adult stem cells is key. We also see the growing role of induced pluripotent stem cells (iPSCs). By combining these, we can get the best results in regenerative medicine.
Using different stem cell types and technologies can make treatments better. Knowing their strengths and weaknesses is vital. This way, we can make therapies that work well.
Embryonic stem cells can become many types of cells, but they raise ethical issues. Adult stem cells are more specific and less controversial. iPSCs are a middle ground, turning regular cells into many types. Mixing these can lead to treatments tailored for each patient.
As we look to the future, combining stem cell methods is essential. Our aim is to use stem cells fully to create new, effective treatments. These treatments will change lives for the better.
Embryonic stem cells can turn into any cell type. Adult stem cells can only turn into specific cell types in their tissue.
They come from the blastocyst stage of embryos. This is usually from in vitro fertilization.
They could help in treating diseases and injuries. This is because they can become different cell types.
iPSCs are made by changing adult cells back into a stem cell state. This makes cells that match a patient for research and treatment.
Adult stem cells are found in adult bodies. They can only turn into a few cell types. They also can’t renew themselves as much.
They can be taken from the patient’s body. This lowers the chance of immune rejection. They are used in treatments for some diseases.
It goes from totipotency (making a whole organism) to unipotency (making one cell type). Pluripotency and multipotency are in the middle.
Using human embryos for research is a big ethical issue. It raises questions about the value of embryos and the risk of destroying them.
Stem cells, like iPSCs, are being looked at for personalized medicine. They could help make cells for each patient for disease modeling and treatments.
The future includes new ways to get, change, and use stem cells. It also includes using them in bioengineering and regenerative medicine.
Autologous uses the patient’s own stem cells. Allogeneic uses stem cells from another person. Allogeneic has a risk of immune rejection.
Embryonic stem cells are more basic and have open DNA. Adult stem cells are more specific and have closed DNA.
https://pmc.ncbi.nlm.nih.gov/articles/PMC9404248/ — “Stem cells: a comprehensive review of origins and emerging clinical …” PMC
https://stemcell.nd.edu/research/alternative-stem-cell-sources/adult-stem-cells/ — Notre Dame’s summary of adult stem cell biology stemcell.nd.edu
https://pmc.ncbi.nlm.nih.gov/articles/PMC6495514/ — “New perspectives in stem cell research: beyond embryonic stem cells” PMC
https://stemcellres.biomedcentral.com/articles/10.1186/s13287-019-1165-5 — “Stem cells: past, present, and future” BioMed Central
https://www.nature.com/articles/s41392-022-01134-4 — Review on stem cell-based therapy for human diseases Nature
https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2024.1414156/full — Paper about plasticity, differentiation potential, and adult stem cells under stress / engineered conditions PMC
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!