Last Updated on October 28, 2025 by
At Liv Hospital, we lead in using chimeric antigen receptor (CAR) T-cell therapy for leukemia patients. This treatment uses a patient’s immune system to fight cancer.
CAR T-cell therapy is a new way to treat cancer with immunotherapy. It makes a patient’s T cells attack leukemia cells. This can lead to high remission rates in some leukemia patients.
Our team offers full care and support for CAR T-cell therapy patients. We focus on a team effort to give top-notch healthcare.
Key Takeaways
- CAR T-cell therapy is a revolutionary treatment for leukemia that harnesses the power of a patient’s immune system.
- This form of immunotherapy involves genetically engineering T cells to target leukemia cells.
- High remission rates have been achieved in patients with certain types of leukemia using CAR T-cell therapy.
- At Liv Hospital, we provide full care and support to patients undergoing CAR T-cell therapy.
- Our team is dedicated to delivering world-class healthcare through a team effort.
The Revolutionary Approach to Fighting Blood Cancer
CAR T cell therapy is a new way to fight leukemia and other blood cancers. It’s needed because old treatments don’t always work well. This is true, even for patients who have tried many treatments before.
In 2017, the first CAR T-cell therapy was approved. This was a big step forward for treating blood cancers like acute lymphoblastic leukemia (ALL). It gave hope to patients who had run out of other options.
The Need for Advanced Leukemia Treatments
Old treatments for leukemia, like chemotherapy and stem cell transplants, have their limits. Many patients don’t get better or even get worse. So, we really need new treatments that work better.
Challenges with Traditional Treatments:
- Relapse or resistance to therapy
- Severe side effects
- Limited efficacy in certain patient populations
CAR T Cell Therapy as a Breakthrough
CAR T cell therapy is a breakthrough in fighting blood cancers. It uses a patient’s own immune cells to attack cancer. For more info, check out the National Cancer Institute’s page on CAR T.
The table below shows how CAR T cell therapy is different from old treatments:
| Treatment Aspect | Traditional Treatments | CAR T Cell Therapy |
|---|---|---|
| Approach | One-size-fits-all | Personalized |
| Efficacy in Relapsed/Refractory Patients | Limited | High |
| Side Effects | Severe | Manageable with proper care |
As the table shows, CAR T cell therapy has big advantages over old treatments. It’s a game-changer in the fight against blood cancer.
What Is CAR T Cell Therapy?
CAR T cell therapy is a new way to fight cancer, mainly for leukemia patients. It’s getting a lot of attention for its targeted and effective treatment of blood cancers.
Definition and Basic Concept
CAR T cell therapy uses a patient’s T cells to attack cancer. Chimeric Antigen Receptor (CAR) T cell therapy makes T cells recognize and destroy cancer cells. This is done by adding a CAR to the T cells, so they can find specific cancer cell markers.
First, T cells are taken from the patient’s blood and sent to a lab. There, they are modified and grown. Then, these CAR T cells are given back to the patient to fight cancer.
The Living Drug Approach
CAR T-cell therapy is called a “living drug” because it uses the patient’s own T cells. These T cells are changed to find and kill cancer cells. This method offers a personalized treatment that could control cancer for a long time.
- CAR T cells can keep growing and watching for cancer in the body.
- The treatment is made just for the patient, making it very personal.
- Because CAR T cells can change and grow with cancer, this therapy is very hopeful.
Understanding CAR T cell therapy and its “living drug” approach shows how innovative it is. It has the power to change cancer treatment forever.
The Science Behind Chimeric Antigen Receptor T Cells
CAR T cell therapy is a complex process. It turns natural T cells into powerful cancer fighters. We’ll look at how CAR T cells are made to target and destroy leukemia cells.
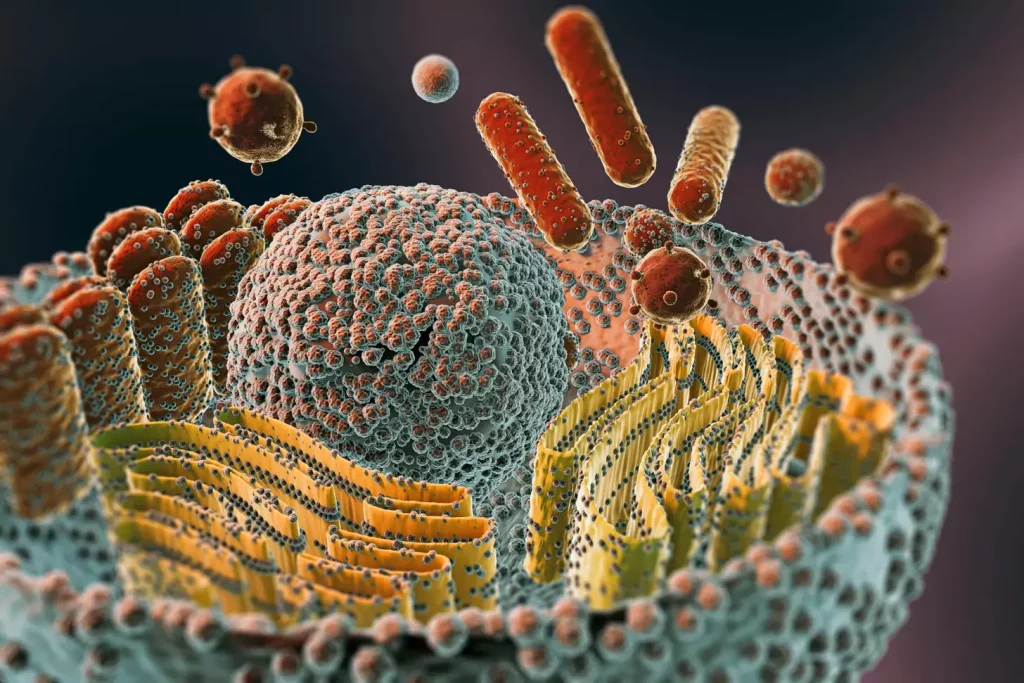
Natural T Cells vs. Engineered CAR T Cells
Natural T cells are key to our immune system. They fight off infected cells and foreign substances. But, they may not always find and attack cancer cells well.
Engineered CAR T cells are made to overcome this. They are programmed to find and attack specific cancer cell markers.
Engineered CAR T cells can spot and attack cancer cells better than natural T cells. This is because they are designed to do so.
How CAR T Cells Are Designed to Fight Cancer
CAR T cells are made to have chimeric antigen receptors (CARs). These receptors help them find and destroy cancer cells. The design includes parts for recognizing antigens, passing signals, and activating the T cell.
To make CAR T cells, scientists modify T cells to carry the CAR. This CAR binds to cancer cell markers, marking them for destruction. This targeted approach makes CAR T cell therapy effective against some leukemias.
The CAR T Cell Therapy Process for Leukemia Patients
For patients with leukemia, CAR T cell therapy is a powerful treatment. It uses the body’s immune system to fight cancer. The process involves several key steps.
Collection: Harvesting the Patient’s T Cells
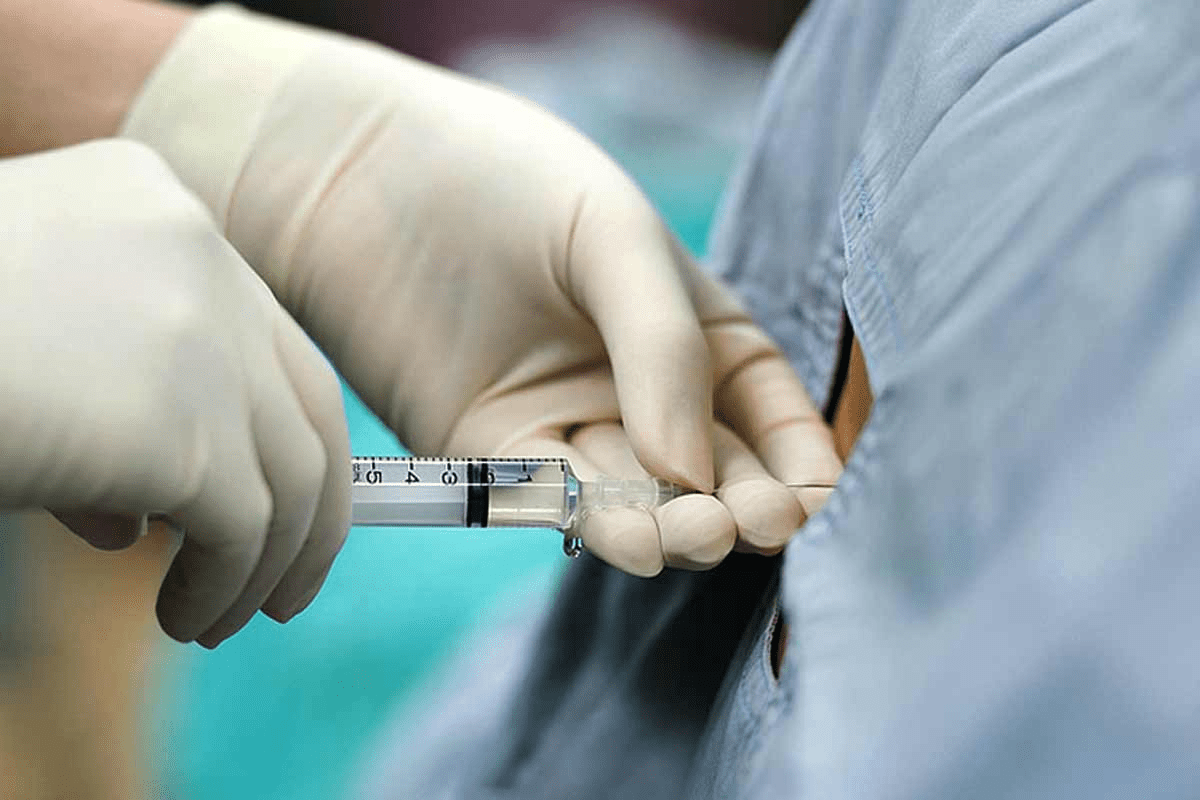
The first step is collecting T cells from the patient. This is done through a procedure called leukapheresis. Leukapheresis separates white blood cells, including T cells, from other blood components. These T cells are essential for creating CAR T cells.
Engineering: Creating the Chimeric Antigen Receptor
After collecting T cells, they are taken to a lab for genetic engineering. Here, they are given a chimeric antigen receptor (CAR) that targets leukemia cells. This CAR allows the T cells to recognize and attack leukemia cells.
The engineering process is detailed and involves several stages. It includes gene transfer and cell expansion. The end result is CAR T cells ready to fight leukemia.
| Step | Description | Outcome |
|---|---|---|
| Collection | T cells are harvested through leukapheresis | T cells are isolated for further processing |
| Engineering | T cells are genetically modified to produce CAR | CAR T cells are created to target leukemia cells |
| Infusion | CAR T cells are infused back into the patient | CAR T cells target and attack leukemia cells |
Infusion and Monitoring: Returning Cells to the Patient
Once engineered, the CAR T cells are infused back into the patient. Patients are closely monitored for any side effects or reactions to the infusion. The CAR T cells then target and destroy leukemia cells, helping to achieve remission.
Monitoring continues after infusion to check treatment success and manage side effects. This includes regular check-ups and tests to evaluate the patient’s response to the CAR T cell therapy.
How CAR T Cell Leukemia Treatment Works
The science behind CAR T cell therapy is rooted in its ability to target specific antigens on leukemia cells. This targeted approach is what makes CAR T cell leukemia treatment so effective.
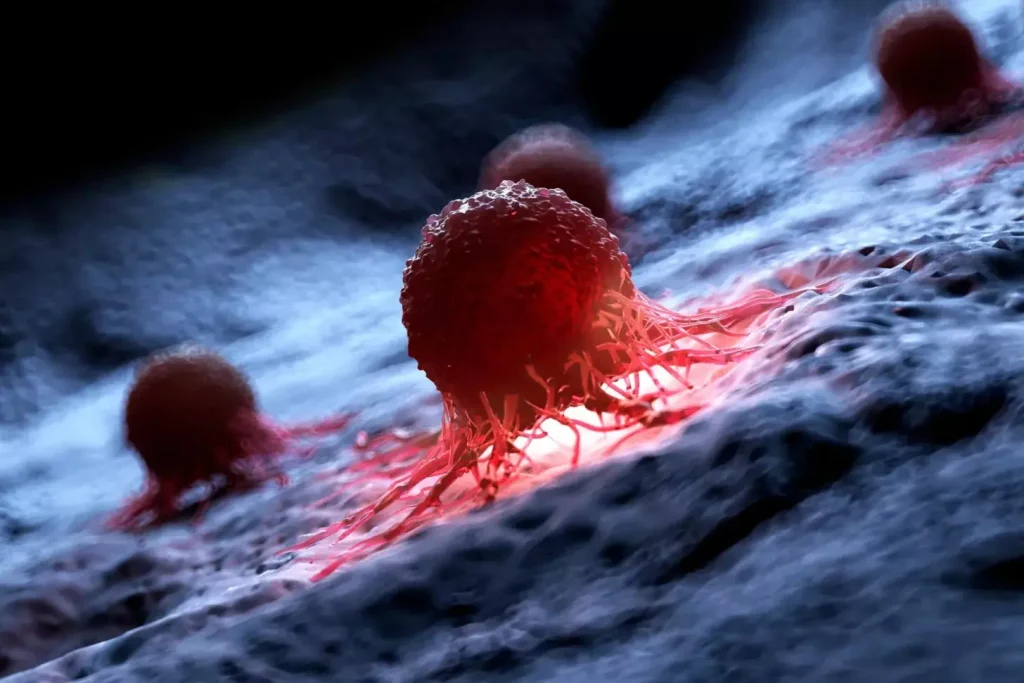
Targeting Specific Antigens on Leukemia Cells
CAR T cells are engineered to recognize and bind to specific antigens on the surface of leukemia cells. This specificity is key for avoiding damage to healthy cells and focusing on cancerous ones. We use chimeric antigen receptor engineering to give T cells this ability.
For example, in B-cell acute lymphoblastic leukemia (B-ALL), CAR T cells target the CD19 antigen. This allows them to kill leukemia cells while sparing normal B cells.
The Killing Mechanism: Perforin and Granzymes
Once CAR T cells bind to leukemia cells, they start a killing process. They release perforin and granzymes. Perforin makes holes in the target cell’s membrane, letting granzymes in. Granzymes then cause the cell to die.
This method is very effective at killing leukemia cells. Studies show CAR T cell therapy can greatly reduce leukemia cell numbers, leading to better patient outcomes.
Amplifying the Immune Response Against Cancer
CAR T cell therapy not only kills leukemia cells but also boosts the immune response against cancer. It activates the immune system, encouraging other immune cells to fight leukemia too.
For more information on CAR T cell therapy, visit Cleveland Clinic’s CAR T Cell Therapy page. It offers detailed information on the treatment, its benefits, and what to expect.
Types of Leukemia Treated with CAR T Cell Therapy
CAR T cell therapy has changed how we treat leukemia. It offers hope to those who have tried other treatments. Now, different leukemia types can be treated with CAR T cell therapy, starting a new chapter in fighting blood cancer.
Acute Lymphoblastic Leukemia
Acute Lymphoblastic Leukemia (ALL) is common in kids but also affects adults. CAR T cell therapy is very effective for ALL that doesn’t respond to other treatments. Clinical trials show high remission rates, improving patient outcomes.
Acute Myeloid Leukemia
Acute Myeloid Leukemia (AML) is tough to treat, mainly in adults. CAR T cell therapy for AML is being studied, with early results looking good. Scientists are working to make CAR T cells better for AML by targeting specific cancer markers.
Other Blood Cancers Responding to CAR T Therapy
CAR T cell therapy is also being tested for other blood cancers. This includes some lymphomas and multiple myeloma. Its flexibility in targeting different cancer markers makes it a promising treatment for many blood cancers.
The following table summarizes the current state of CAR T cell therapy for different types of leukemia:
| Leukemia Type | CAR T Cell Therapy Status | Notable Outcomes |
|---|---|---|
| Acute Lymphoblastic Leukemia (ALL) | Approved for relapsed/refractory cases | High remission rates in clinical trials |
| Acute Myeloid Leukemia (AML) | Under investigation | Promising early results |
| Other Blood Cancers | Varies by cancer type | Potential for treating various hematological malignancies |
Clinical Effectiveness and Success Rates
CAR T cell therapy is changing how we treat leukemia. It’s a big step forward in immunotherapy. This therapy is showing great results and success.
Remission Rates in Pediatric and Adult Patients
CAR T cell therapy is working well for kids and adults with certain leukemias. In kids with Acute Lymphoblastic Leukemia (ALL), some studies show remission rates of 80% to 90%. For adults, the results vary but are promising.
- Pediatric patients with ALL have shown high remission rates with CAR T cell therapy.
- Adult patients with certain types of leukemia are also benefiting from this treatment.
- Ongoing research is focused on improving outcomes for all patient groups.
Long-term Outcomes and Survival Statistics
Looking at long-term results and survival is key. The data shows some patients have durable remissions. This means they live longer. Studies are watching these outcomes closely.
- Durable remissions have been observed in a subset of patients.
- Survival statistics indicate a positive trend for patients responding to CAR T cell therapy.
- Continuous monitoring is essential to understand the long-term benefits and possible late effects.
As we learn more, CAR T cell therapy looks very promising for leukemia treatment.
Side Effects and Complications of CAR T Cell Therapy
CAR T cell therapy brings hope to leukemia patients. But, knowing its side effects is key for good care. We must weigh the benefits against the risks.
Causes and Symptoms of Cytokine Release Syndrome
Cytokine release syndrome (CRS) is a big side effect of CAR T cell therapy. It happens when T cells release a lot of cytokines into the blood. This can cause mild symptoms like fever and fatigue or serious issues like low blood pressure and organ failure.
CRS can be different for everyone. It’s important to watch patients closely and sometimes use special treatments. Knowing the causes and spotting symptoms early helps manage CRS well.
Cognitive and Neurological Effects of Neurotoxicity
Neurotoxicity is another issue with CAR T cell therapy. It can cause problems like confusion, headaches, or even seizures. These symptoms can be mild or very serious.
We’re learning more about why neurotoxicity happens. It’s thought that cytokines and other substances can harm the brain. Quick action and care are key to avoiding lasting damage.
B-Cell Aplasia and Other Long-term Considerations
B-cell aplasia is a common long-term effect. It happens when CAR T cells target B cells. This can lead to low levels of antibodies, making infections more likely and needing treatment with immunoglobulins.
Other long-term issues include the chance of the disease coming back. It’s important to keep an eye out for this. A good follow-up plan is needed to manage these effects.
| Side Effect/Complication | Symptoms | Management Strategies |
|---|---|---|
| Cytokine Release Syndrome (CRS) | Fever, fatigue, hypotension, organ failure | Monitoring, anti-cytokine therapies (e.g., tocilizumab) |
| Neurotoxicity | Confusion, headache, seizures, cerebral edema | Supportive care, corticosteroids, seizure prophylaxis |
| B-Cell Aplasia | Infections, hypogammaglobulinemia | Immunoglobulin replacement therapy |
Knowing about the side effects and complications of CAR T cell therapy helps doctors care for patients better. Ongoing research and experience will help us deal with these issues better.
Managing and Treating CAR T Cell Therapy Complications
It’s vital to manage CAR T cell therapy complications well. This ensures patient safety and treatment success. CAR T cell therapy is changing how we treat some leukemias. Knowing how to handle its side effects is key.
CAR T cell therapy can cause big problems, like Cytokine Release Syndrome (CRS) and neurological side effects. Handling these issues right is essential for better patient results.
Specialized Protocols for Cytokine Release Syndrome
CRS is a serious issue with CAR T cell therapy. Early treatment is vital. We have special plans to tackle CRS, including:
- Watching patients closely for CRS signs like fever, low blood pressure, and breathing trouble
- Using tocilizumab, a drug that blocks IL-6 receptors, to lessen CRS
- Offering support care, like fluids and oxygen, when needed
Addressing Neurological Side Effects
Neurological side effects, like confusion, memory loss, and seizures, can happen after CAR T cell therapy. Quick action is needed to avoid lasting harm. We tackle these side effects by:
- Keeping a close eye on patients for neurological signs
- Starting corticosteroids to fight inflammation
- Providing supportive care, like seizure prevention and symptom management
Long-term Monitoring Requirements
Long-term checks are critical to catch late effects of CAR T cell therapy. These can include B-cell aplasia and secondary cancers. We stress the need for:
- Regular check-ups to watch patient health
- Imaging and lab tests to spot complications early
- Teaching patients to recognize signs of complications
By managing complications well and keeping a close eye on patients, we can make CAR T cell therapy safer and more effective.
Recent Advances in CAR T Cell Therapy
The field of CAR T cell therapy is growing fast. New discoveries are making it more effective. Scientists are always looking for ways to make this treatment better and use it for more types of cancer.
Dual-Targeted CAR T Cells for Improved Efficacy
Dual-targeted CAR T cells are a big step forward. These cells can find and destroy cancer cells that show two different signs. This could make the treatment work better.
- Enhanced specificity: These cells are better at finding cancer cells. This means they are less likely to harm healthy cells.
- Increased efficacy: By going after two targets, these cells might be able to beat cancer cells that try to hide.
- Better outcomes: Early tests show that these cells could lead to better results and longer remissions.
Overcoming Tumor Heterogeneity Challenges
Tumors are made up of different cells, which makes treating them hard. New research is trying to solve this problem:
- Multi-antigen targeting: CAR T cells that target more than one antigen can tackle the problem of different cells in a tumor.
- Combination therapies: Scientists are looking at using CAR T cells with other treatments to make them work better together.
- Personalized approaches: New ways to study tumors are helping make CAR T cell treatments that fit each patient’s cancer better.
These new developments in CAR T cell therapy are big wins for treating leukemia and other blood cancers. As scientists keep working, we can look forward to even better results and using this therapy for more cancers.
Specialized Treatment Centers and Patient Care
CAR T cell therapy needs advanced tech and a full care plan found in special centers. These centers, like Liv Hospital, show the best in patient care. They are key in the treatment’s growth.
The Importance of Experienced Medical Teams
Teams with experience are vital for CAR T cell therapy success. They include doctors and support staff with the needed skills. Their know-how helps manage side effects and gives top care.
“The expertise of our medical team is a critical factor in the success of CAR T cell therapy,” says a key point. This teamwork meets patients’ complex needs in this therapy.
World-Class Facilities Like Liv Hospital
Top facilities are key for quality CAR T cell therapy. Places like Liv Hospital have the latest tech and support patients well. Their staff is dedicated to outstanding care.
Liv Hospital stands out for CAR T cell therapy care. It has the best setup and focuses on patients, setting a global standard.
Patient-Centered Approaches to CAR T Therapy
Putting patients first is key in CAR T cell therapy. It means care that fits each patient’s needs, not just the medical side. It also includes emotional and mental support.
This focus on the whole patient boosts care quality and results. A patient shared,
“The care I received was not just about treating my condition, but about supporting me as a person.”
This kind of care is what we aim for in CAR T cell therapy.
Conclusion: The Future of CAR T Cell Therapy
Looking ahead, CAR T cell therapy is set to change the game in cancer treatment. New studies and trials will make this therapy even better. It will bring hope to those fighting leukemia and maybe other cancers too.
This therapy is on track to help more people with blood cancers. As it grows, we’ll see better results and more people getting help. It’s a bright future for CAR T cell therapy.
Liv Hospital is leading the way in this field. They offer top-notch care and support for patients from around the world. With each new discovery, they’re ready to provide the latest treatments and care with kindness.
FAQ
What is CAR T cell therapy, and how does it work to treat leukemia?
CAR T cell therapy is a new way to fight cancer. It uses the body’s T cells to attack cancer cells. First, we take T cells from the patient. Then, we make them recognize and destroy leukemia cells. After that, we put them back into the patient to fight the cancer.
What types of leukemia can be treated with CAR T cell therapy?
CAR T cell therapy mainly treats Acute Lymphoblastic Leukemia (ALL). It also shows promise for Acute Myeloid Leukemia (AML) and other blood cancers.
What are the possible side effects of CAR T cell therapy?
Side effects include Cytokine Release Syndrome (CRS), neurotoxicity, and B-cell aplasia. We watch patients closely and have ways to handle these side effects.
How effective is CAR T cell therapy in achieving remission for leukemia patients?
CAR T cell therapy has high remission rates in both kids and adults with certain leukemias. It gives new hope to those who didn’t respond to other treatments.
What is Cytokine Release Syndrome (CRS), and how is it managed?
CRS is a serious side effect of CAR T cell therapy. It happens when cytokines flood the blood. We treat CRS with tocilizumab and corticosteroids.
How are neurological side effects of CAR T cell therapy addressed?
Neurological side effects like confusion and seizures are managed with supportive care. Sometimes, we use corticosteroids or other medicines to help symptoms.
What is the role of specialized treatment centers in CAR T cell therapy?
Centers like ours are key in providing top-notch care for CAR T cell therapy. We have experienced teams and the best facilities.
What advancements are being made in CAR T cell therapy to improve treatment outcomes?
New developments include dual-targeted CAR T cells and ways to tackle tumor heterogeneity. These aim to make CAR T cell therapy more effective and lasting.
How does CAR T cell therapy compare to traditional leukemia treatments?
CAR T cell therapy is a groundbreaking approach to leukemia treatment. It uses the immune system for a more targeted and possibly effective treatment than traditional therapies.
What is the future outlook for CAR T cell therapy in treating leukemia and other cancers?
The future of CAR T cell therapy looks bright. Ongoing research aims to improve results, treat more cancers, and enhance patient care.