
Radiation therapy is a common treatment for cancer. Knowing what to expect can help reduce anxiety. The journey starts with a meeting with a radiation oncologist. Then, a simulation or planning process called radiation mapping or CT simulation follows.
This first step is key to figuring out the exact area to treat. It usually takes 30 to 60 minutes, answering the question of how long does radiation mapping take. The radiation team uses imaging to map the tumor’s location and decide the best way to treat it.
Key Takeaways
- The simulation process, or radiation mapping, is essential before starting radiation therapy.
- The duration of radiation mapping typically ranges from 30 to 60 minutes.
- A personalized treatment plan is created based on the simulation to maximize effectiveness and minimize side effects.
- Radiation therapy involves daily treatments, usually once a day, Monday through Friday, for several weeks.
- The total appointment time for daily treatments, including setup, is about one hour each day.
Understanding Radiation Therapy for Cancer Treatment
Radiation therapy is a key part of fighting cancer. It uses high-energy rays to kill or slow cancer cells. This treatment is often used alone or with surgery and chemotherapy.
How Radiation Therapy Targets Cancer Cells
Radiation therapy damages cancer cells’ DNA. This stops them from growing and dividing. High-energy rays target the tumor site to kill the cells.
The success of radiation therapy depends on the cancer type and stage, and the patient’s health. External beam radiation therapy is common. It uses a machine outside the body to target the tumor, protecting healthy tissue.
Types of Radiation Treatment Options
There are two main types: external beam radiation therapy and internal radiation therapy, or brachytherapy. External beam uses a machine outside the body. Internal radiation places a radioactive source near the tumor.
The choice depends on the cancer’s type, size, and location, and the patient’s health. Brachytherapy is often used for localized tumors, like prostate cancer.
When Radiation Therapy Is Recommended
Radiation therapy is chosen based on the cancer type, stage, and the patient’s health. It can aim to cure the cancer or improve the quality of life.
Radiation therapy aims to control cancer while protecting healthy cells. Knowing about radiation therapy helps patients make informed decisions about their care.
The Radiation Therapy Consultation Process

Understanding radiation therapy starts with a detailed consultation with a radiation oncology team. This first meeting is key for patients to grasp their treatment choices and what therapy entails.
Meeting Your Radiation Oncology Team
In the initial consultation, patients meet with their radiation oncologist and support staff. This team will walk patients through the treatment, answering any questions or worries. The oncologist will detail the treatment plan, including the type of radiation and expected results.
Initial Assessment and Medical History Review
A detailed initial assessment reviews the patient’s medical history. This step is essential to understanding any past treatments or health issues that might affect the radiation therapy. The team will also discuss the patient’s health and any current medications.
Discussing Treatment Goals and Expectations
Discussing treatment goals and expectations is a critical part of the radiation therapy consultation. The oncologist will explain the treatment’s objectives, how long it will last, and possible side effects. This is also a chance for patients to ask questions and learn how to handle any side effects.
Patients often ask what radiation therapy is like. While experiences vary based on the treatment area and plan, common feelings include fatigue, mild skin changes, or localized discomfort. The radiation oncology team offers personalized advice and support during the treatment.
How Long Does Radiation Mapping Take: CT Simulation Explained
Radiation mapping, also known as CT simulation, is a key step before radiation therapy. It helps create a detailed treatment plan. This plan makes sure the radiation hits the tumor right, while keeping healthy tissues safe.
Purpose and Importance of CT Simulation
CT simulation gives detailed images of tumors and tissues around them. This info is key for the radiation team to plan the best treatment. CT simulation accurately marks the tumor, which is vital for good radiation therapy.
A leading radiation oncologist said, “CT simulation is a cornerstone of modern radiation therapy. It lets us give precise doses to tumors while protecting normal tissues.” This shows how important CT simulation is in today’s cancer treatment.
Step-by-Step Mapping Procedure
The CT simulation process has several steps:
- Patient positioning: The patient is placed on a table, and devices are used to keep them steady.
- CT scanning: A CT scanner takes detailed images of the tumor and tissues around it.
- Image acquisition: The images are used to make a precise treatment plan.
Duration Expectations (30-60 Minutes)
The CT simulation process usually takes 30 to 60 minutes. The time needed can change based on the case’s complexity and the treatment plan’s specifics. Patients should plan and ask their radiation oncology team about what to expect.
In summary, radiation mapping or CT simulation is a critical part of radiation therapy. It gives the needed info for a precise treatment plan. This ensures patients get the best care possible.
Creating Your Personalized Radiation Treatment Plan
Creating a customized radiation plan uses advanced technology and precise medical skills. This approach makes sure the treatment fits the patient’s needs perfectly. It aims to make the treatment as effective as possible.
3D Treatment Planning Technology
3D treatment planning technology helps find the tumor’s exact location and size. This technology lets doctors send precise amounts of radiation to the tumor. It also helps protect healthy tissues around it.
Determining Optimal Radiation Dosage
Finding the optimal radiation dosage is key for treatment success. Doctors carefully calculate the dose. They make sure the tumor gets enough radiation while keeping healthy tissue safe.
| Factors | Description | Impact on Dosage |
| Tumor Size and Location | The size and location of the tumor affect the dosage and delivery method. | Directly influences the radiation dosage. |
| Patient’s Overall Health | The patient’s general health and medical history are considered. | Affects the tolerance to radiation and possible side effects. |
| Type of Cancer | Different types of cancer respond differently to radiation. | Determines the effectiveness of the radiation dosage. |
Strategies for Protecting Healthy Tissue
Keeping healthy tissue safe is a major goal in radiation therapy. Doctors use precise targeting and advanced technology. They also plan carefully to lower the risk of side effects.
Latest Academic Protocols in Radiation Planning
The latest academic protocols in radiation planning keep getting better. They use new research and technology. These protocols make sure radiation treatment follows the best and most effective standards.
Radiotherapy might need changes in dosage and schedule to keep up with tumor changes. The planning process uses advanced tech like 3D treatment planning. It helps find the best radiation dosage and protects healthy tissues.
Radiation Therapy Schedule and Timeline
The radiation therapy schedule is made just for each patient. It’s designed to be effective and reduce side effects. This personalized plan makes treatment better for everyone.
Standard Treatment Frequency
Most treatments happen five days a week, from Monday to Friday. This schedule lets the body recover between sessions. It helps keep healthy tissues safe.
Typical Treatment Schedule:
- Monday to Friday: Radiation therapy sessions
- Weekends: Break to allow healthy tissues to recover
Total Duration of Radiation Treatment Courses
The length of radiation therapy varies. It depends on the cancer type and stage, and the treatment goals. Courses can last from weeks to months.
| Treatment Type | Typical Duration |
| Curative Treatment | 6-7 weeks |
| Palliative Treatment | 2-4 weeks |
| Stereotactic Body Radiation Therapy (SBRT) | 1-5 fractions |
Factors That Influence Treatment Length
Several things can affect how long treatment lasts. These include the tumor size and location, the patient’s health, and other medical conditions.
Key Factors:
- Tumor size and location
- Type and stage of cancer
- Patient’s overall health
- Treatment goals (curative vs. palliative)
Scheduling Considerations for Patients
Patients should talk to their radiation oncologist about scheduling. Work, travel, and personal needs should be considered.
Knowing the radiation therapy schedule helps patients prepare for their treatment journey.
What Happens During Each Radiation Treatment Session
Each radiation treatment session is a detailed plan to target cancer cells. It involves several steps to make sure the radiation goes right to the tumor.
Arrival and Preparation Procedures
When patients arrive, they change into a gown and remove jewelry. This is key for accurate radiation delivery. Radiation therapists help patients get ready, making sure they are comfortable and in the right spot.
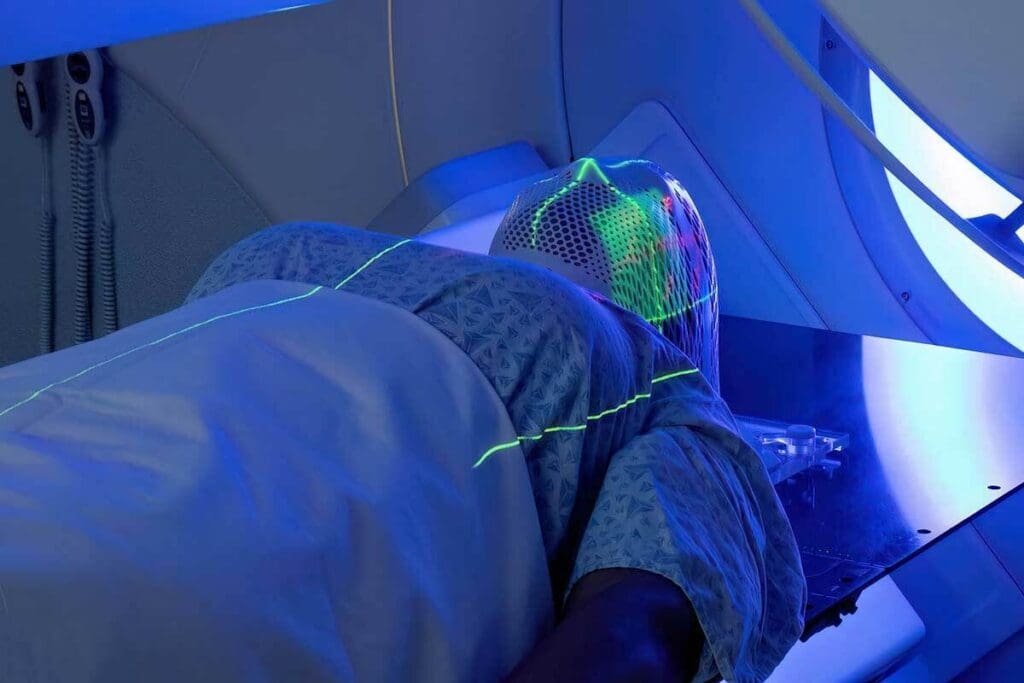
Positioning and Immobilization Techniques
Radiation therapists then place the patient on the treatment table. They use special devices to keep the patient steady. These devices are made just for each patient, giving the needed support.
“The use of immobilization devices has significantly improved the precision of radiation therapy,” – A radiation therapist
Actual Radiation Delivery Process
The actual radiation part is quick, lasting just a few minutes. The machine sends the right amount of radiation to the tumor. Patients don’t feel the radiation, and it’s painless.
Total Session Duration
The whole session, from start to finish, takes 10 to 45 minutes. Even though the radiation part is short, the whole process needs careful planning and checking to be safe and accurate.
In summary, each radiation treatment session is a detailed process. It includes careful planning, precise positioning, and accurate radiation delivery. Knowing what happens in each session helps patients prepare better for treatment.
Physical Sensations and Experiences During Radiation
Radiation therapy is usually painless, but patients have questions. Knowing what to expect can ease worries and prepare them for treatment.
Is Radiation Treatment Painful?
Many patients wonder if radiation therapy hurts. The answer is no, it’s not painful during treatment. Experts in cancer treatment say it’s a non-invasive process.
But some might feel discomfort from the treatment position or their condition. Talking to your radiation oncology team can help with these issues.
Common Physical Sensations During Treatment
Even though it’s painless, patients might feel different things during treatment. Here are some common experiences:
- Fatigue: Feeling very tired, which can get worse as treatment goes on.
- Skin changes: Mild redness, itching, or dryness in the treated area.
- Localized discomfort: Some might feel pain or discomfort in the treated area.
Immediate Post-Session Experiences
After each session, patients might feel many things. Some feel relieved, while others worry about future sessions or treatment success.
Physically, patients might not see side effects right away. But they might feel tired or notice changes in the treated area. Following your healthcare team’s post-treatment care is key to managing side effects.
Emotional Aspects of Undergoing Radiation
The emotional side of radiation therapy is important. Patients can feel anxious, fearful, hopeful, or determined. It’s essential to acknowledge these feelings and talk about them with your healthcare team or a support group.
Talking openly with your radiation oncology team can help with emotional concerns. They can offer the support you need during treatment.
Managing Side Effects of Radiation Therapy
Managing side effects of radiation therapy is key for cancer patients. It helps improve their quality of life during and after treatment.
Fatigue Management Strategies
Fatigue is a common side effect of radiation therapy. Pacing activities and taking breaks can help. Eating a healthy diet is also good. Patients should talk to their healthcare team about their needs.
Skin Care During Radiation Treatment
Radiation therapy can cause skin issues like redness and dryness. Gentle skin care helps. Using mild soap and avoiding harsh products is advised. Patients should follow their radiation team’s skin care tips.
Site-Specific Side Effects by Treatment Area
Side effects vary by treatment area. For example, head and neck treatment may cause dry mouth or difficulty swallowing. Pelvic area treatment may lead to urinary frequency or diarrhea. Knowing these side effects helps patients prepare and manage them better.
When to Contact Your Healthcare Team
Patients should know when to contact their healthcare team about side effects. Severe or persistent side effects need immediate reporting. They should also reach out for unusual symptoms or worsening conditions.
Monitoring Progress and Treatment Adjustments
Keeping track of how well radiation therapy works is key in cancer treatment. It helps doctors see if the treatment is working and make changes if needed.
Regular Assessment Procedures
During radiation therapy, doctors often check how the tumor is reacting. They use clinical checks, imaging, and lab tests. How often depends on the cancer type, stage, and the patient’s health.
Regular checks are important to spot any changes in the tumor. This lets doctors adjust the treatment plan quickly. It keeps the treatment effective and reduces side effects.
Adapting Treatment to Tumor Response
The goal of radiation therapy is to hit the tumor with the right amount of radiation. Adjustments are made based on how the tumor reacts. This ensures the treatment is as effective as possible.
Tumor response can differ from person to person. Ongoing checks help doctors tailor the treatment. This might mean changing the radiation dose, schedule, or technique.
Potential Dosage and Schedule Modifications
Sometimes, the radiation dose or schedule needs to be changed. These changes depend on how the tumor is responding and any side effects the patient has.
| Modification Type | Purpose | Potential Benefits |
| Dosage Adjustment | Optimize tumor response | Enhanced treatment effectiveness |
| Schedule Modification | Minimize side effects | Improved patient comfort |
Imaging During Treatment Course
Imaging, like CT or MRI scans, is key in tracking the tumor’s response. These scans show the tumor’s size, shape, and location. This helps doctors make the best treatment decisions.
Using advanced imaging and regular checks, doctors can fine-tune radiation therapy. This improves patient outcomes and quality of life.
Post-Radiation Treatment Recovery and Follow-up
The journey doesn’t end with radiation therapy. It moves into a vital recovery phase. This time is key for checking health, solving problems, and making sure treatment works right.
What to Expect After Completing Radiation
After radiation therapy, patients start feeling the first signs of recovery. Recovery times differ for everyone. Follow-up care is critical during this phase to watch progress and fix any new problems quickly.
Follow-up Appointment Schedule
Patients will see their radiation oncologist for many follow-up visits. These visits are to check on recovery, watch for cancer return, and handle side effects. How often these visits happen can change, but they’re usually more often in the first year.
| Time After Treatment | Follow-up Frequency |
| 0-1 Year | Every 3-4 Months |
| 1-2 Years | Every 6 Months |
| 2+ Years | Annually |
Long-term Monitoring Protocol
A long-term plan is set to keep an eye on the patient’s health over time. This includes regular check-ups, imaging tests, and more as needed. The aim is to spot any problems early, like cancer coming back or side effects showing up later.
Managing Delayed Side Effects
Some patients face side effects from radiation therapy later on. It’s vital for patients to know about these possible side effects and when to get medical help. Common late side effects include fibrosis, secondary cancers, and organ problems, based on where the treatment was given.
Knowing what to expect in the recovery phase and sticking to the follow-up plan helps patients on their way to getting better. Talking openly with the healthcare team is important for handling any challenges that come up.
Conclusion: Navigating Your Radiation Therapy Journey Successfully
Knowing what to expect from radiation therapy can really help. It makes it easier to get through the treatment. With the right info and support, patients can do well and feel better.
Understanding the treatment, its side effects, and follow-up care is key. Being informed helps patients manage their treatment better. They can work closely with their team for a good outcome.
A team of healthcare professionals is vital for a successful journey. Patients should ask questions and seek help when needed. This way, radiation therapy can be a powerful tool against cancer, helping patients recover.
FAQ
What is radiation therapy, and how does it work?
Radiation therapy uses high-energy rays to kill cancer cells. It’s a key part of cancer treatment. It can be used alone or with other treatments like surgery and chemotherapy.
How long does radiation mapping take?
Radiation mapping, or CT simulation, takes 30 to 60 minutes. The team uses imaging to map the tumor and plan treatment.
What happens during a radiation therapy consultation?
At the consultation, patients meet with their team. This includes doctors, nurses, and support staff. They review the patient’s history and discuss treatment goals.
How is a personalized radiation treatment plan created?
A personalized plan involves several steps and advanced technologies. The team uses 3D planning to accurately target the tumor for precise radiation delivery.
What is the typical schedule for radiation therapy?
Radiation therapy is given Monday to Friday for several weeks. The exact duration depends on the cancer type and stage.
How long does each radiation treatment session take?
The actual treatment is quick, lasting a few minutes. The whole session, including prep, takes 10 to 45 minutes.
Is radiation treatment painful?
Radiation therapy is generally painless. Most patients don’t feel much discomfort. Some might feel tired or experience skin changes.
How are the side effects of radiation therapy managed?
Managing side effects is key to quality of life. Patients can pace activities, take breaks, and eat well to fight fatigue. Skin care is also important.
What happens after completing radiation therapy?
After treatment, patients have follow-up appointments. These are important for monitoring recovery and addressing any issues. They help catch cancer recurrence early.
How is progress monitored during radiation therapy?
Regular checks are done to see how the tumor responds. Imaging technologies help assess progress and guide treatment adjustments.
References
- National Cancer Institute. (n.d.). Radiation therapy side effects. https://www.cancer.gov/about-cancer/treatment/types/radiation-therapy/side-effects









