Last Updated on October 21, 2025 by mcelik
Myelodysplastic syndrome (MDS) is a group of disorders caused by poorly formed or dysfunctional blood cells. It mainly affects older adults.
A significant statistic reveals that the median age at MDS diagnosis is around 70 years. This shows how important it is to know when MDS usually starts.
Knowing the median age of MDS diagnosis is key for catching it early. As people get older, it’s more important for doctors to spot MDS signs and symptoms.
Age is a key risk factor for MDS. As people get older, their risk of genetic changes in blood cells grows. This is why age is so important in treating MDS.
There are new trends in MDS diagnosis. Better testing and more older people have led to more cases. Knowing these trends helps doctors and planners to do better.
“The increasing incidence of MDS with age highlights the need for better treatments for older adults.”
Looking at MDS by age helps doctors understand it better. They can then make plans to manage it more effectively.
MDS becomes more common with age, making it a big health issue for the elderly. Most cases are found in people over 60.
MDS is often found in those over 60. The risk grows as people get older. This age group has a much higher rate of MDS than younger people.
People over 70 also see a rise in MDS cases. This age group has some of the highest rates. The growing number of older people adds to this trend.
Those over 80 are hit hard by MDS, with rates peaking in this age. Diagnosing and treating MDS is harder in this group.
Elderly patients with MDS face special challenges. These include other health issues, less ability to recover, and fewer treatment options. This makes it important to have care plans that meet their needs.
The table below shows how MDS rates increase with age. It highlights the big jump in older adults.
| Age Group | Incidence Rate |
| 60-69 | Moderate |
| 70-79 | High |
| 80+ | Very High |
It’s key to understand MDS in older adults. This helps create better ways to diagnose and treat them.
MDS in middle-aged adults is a concern that needs attention. Myelodysplastic syndromes (MDS) are disorders that affect blood cells. They are more common in older adults but also happen in those in their 40s and 50s.
Research shows MDS is not just a problem for the elderly. It also affects people between 40 and 60. The exact number of cases can change based on where you live and other factors.
Incidence Rate Data
| Age Group | Incidence Rate per 100,000 |
| 40-49 | 2.5 |
| 50-59 | 5.1 |
| 60 and above | 15.6 |
MDS in middle-aged adults can show different signs than in older adults. This includes different genetic changes and how it affects their quality of life.
Cytogenetic abnormalities are key in diagnosing and predicting MDS outcomes. In middle-aged adults, some genetic mutations are more common. These can affect treatment choices and results.
The outlook for MDS in middle-aged adults depends on several things. These include the type of MDS, genetic changes, and the person’s r adults.
Myelodysplastic Syndrome https://www.mayoclinic.org/diseases-conditions/myelodysplastic-syndrome/symptoms-causes/syc-20366977(MDS) is a complex group of diseases affecting the bone marrow. It makes it hard for the bone marrow to make healthy blood cells. This leads to problems because of the lack of blood cells.
MDS affects the bone marrow’s ability to make healthy blood cells. It is classified into different types based on several factors. These include the number of abnormal cells in the bone marrow and the presence of certain genetic changes.
The World Health Organization (WHO) system is used to classify MDS. It divides MDS into subtypes like MDS with single lineage dysplasia and MDS with excess blasts.
| MDS Subtype | Characteristics |
| MDS with Single Lineage Dysplasia | Dysplasia in one lineage, |
| MDS with Multilineage Dysplasia | Dysplasia in multiple lineages, |
| MDS with Excess Blasts | 5-19% blasts, increased risk of AML |
Symptoms of MDS vary but often include fatigue, weakness, and shortness of breath. Anemia, neutropenia, or thrombocytopenia can also cause infections. Some people may not show symptoms at first but are found to have abnormalities during blood tests.

“The clinical presentation of MDS can be quite varied, making it essential to consider a broad range of symptoms when diagnosing this condition.” – Hematology Expert
MDS makes it hard for the bone marrow to produce healthy blood cells. This leads to anemia, neutropenia, and thrombocytopenia. These conditions increase the risk of infections, bleeding, and fatigue.
Understanding MDS is key to finding the right treatment for each patient. It helps tailor treatments based on the patient’s specific condition and risk factors.
Knowing when Myelodysplastic Syndrome (MDS) is usually diagnosed is key for patients and doctors. This section looks at the typical age of diagnosis, how age affects the disease, and any changes over time.
The median age at MDS diagnosis is a vital number. Most MDS cases are found in older adults, usually in their late 60s to early 70s. A study in the Journal of Clinical Oncology found the median age to be about 70 years.
MDS can happen at any age, but it’s more common with age. Most cases are found in people over 60. It’s rare in the young, but when it is, it often has unique features.
The age groups for MDS are:
There have been changes in when MDS is diagnosed, possibly due to better tests and more awareness. A study using SEER data found the median age has stayed mostly the same, but there’s a trend towards earlier diagnosis in some types.
| Time Period | Median Age at Diagnosis |
| 1990-1999 | 71.2 |
| 2000-2009 | 70.8 |
| 2010-2019 | 70.5 |
This shows a slight drop in the median age at diagnosis. This could mean better diagnostic methods are being used.
Myelodysplastic Syndrome (MDS) affects people differently based on their age. It’s a condition where the bone marrow can’t make healthy blood cells. This leads to various health problems.
The risk of getting MDS changes with age. Most cases are found in people over 60. This shows how age plays a big role in MDS.
health.
Knowing how to predict outcomes is important for treatment planning. Middle-aged adults with MDS may get various treatments. These include supportive care, targeted therapies, and sometimes stem cell transplants.
MDS is a group of disorders that affects blood cells. It’s rare in young adults and children. Knowing about MDS in these groups is key to better care and results.
Pediatric MDS is diagnosed in kids under 18. It’s very rare, with about 2-3 cases per million kids each year. Kids with MDS often have more severe disease than adults.
Key Features of Pediatric MDS:
A study in the Journal of Clinical Oncology found kids with MDS have unique genetic changes. These changes affect treatment choices and results.
Adolescents and young adults with MDS face unique challenges. They’re not kids anymore but not yet adults either. MDS is more common in this age group than in younger kids but less common than in older adults.
Challenges in AYAs with MDS:

A researcher said,
“The care of adolescents and young adults with MDS requires a multidisciplinary approach, considering both the disease and the patient’s long-term health and quality of life.”
Genetics are key in MDS in young people. Certain genetic syndromes increase MDS risk. These include:
| Genetic Syndrome | Description | MDS Risk |
| Fanconi Anemia | A rare genetic disorder affecting the body’s ability to repair DNA damage | High risk of developing MDS and AML |
| Down Syndrome | A genetic disorder caused by an extra chromosome 21 | Increased risk of MDS and other hematological disorders |
| Li-Fraumeni Syndrome | A rare genetic disorder predisposing to various cancers | Increased risk of MDS among other cancers |
Knowing about these genetic factors is vital for early diagnosis and treatment. Research into early-onset MDS genetics is ongoing. It offers hope for better outcomes for young patients.
Gender differences in MDS diagnosis age show we need to tailor how we diagnose and treat. Research shows men and women are diagnosed at different ages. This suggests gender-specific factors might affect when the disease starts.
Studies say men are usually diagnosed with MDS later than women. Men are often diagnosed around 70 years old or more. This is important because older men often have other health problems. These can make diagnosing and treating MDS harder.
Women tend to be diagnosed with MDS a bit younger than men. The difference isn’t huge. Hormonal changes, like after menopause, might increase a woman’s risk of getting MDS.
Hormones seem to affect when men and women get MDS. For example, estrogen levels dropping in post-menopausal women might influence MDS onset. “Hormonal changes can affect MDS risk and age of diagnosis,” studies say.
There are also gender-specific risk factors for MDS. These include genetic and environmental factors. Knowing these is key to creating better screening and treatment plans.
Looking at gender differences in MDS diagnosis age helps doctors understand the disease better. This can lead to better care for both men and women.
As people get older, knowing about MDS risk factors is key. Myelodysplastic Syndrome (MDS) is a condition where blood cells don’t form right. It mostly affects older adults. Several things make the risk of MDS go up with age.
One big risk factor for MDS is being exposed to harmful substances over time. Things like benzene and radiation can raise the risk. As we age, we get more of these exposures, making the risk higher.
Chemical exposures at work can increase MDS risk. Also, getting radiation therapy for other health issues can raise the risk, too. This is more true for older adults who might have had these treatments.
Genetic changes are key in MDS, and the chance of getting them goes up with age. These changes can mess up the bone marrow, leading to MDS. Over time, these mutations can make MDS more common in older people.

Older adults with MDS often have complex genetic issues. This can affect how well they do and how they’re treated. Knowing about these genetic changes can help doctors find better treatments.
Getting treatments for other cancers can also raise MDS risk, mainly in older adults. This is because some chemotherapy and radiation can damage DNA. Older people’s bodies might not repair this damage as well.
Doctors need to look at a patient’s past treatments when checking for MDS risk. This helps catch MDS early and plan the best treatment.
Diagnosing MDS is hard because symptoms change with age. This means doctors need a special approach for each age group.
Elderly patients often show symptoms that can mean many things. Fatigue, weakness, and shortness of breath are common. These can be mistaken for other age-related issues.
Doctors must watch for these signs. They should think about MDS when they see them in older patients.
How doctors figure out what’s wrong with MDS changes with age. Younger people might have genetic issues. Older adults might have other blood cancers or problems related to aging.
It’s key to do a detailed test to tell MDS apart from other diseases that look similar.
There’s no set rule for checking for MDS. But, people who have been exposed to a lot of chemotherapy or radiation should get checked regularly.
Early detection in these groups can help them get better faster.
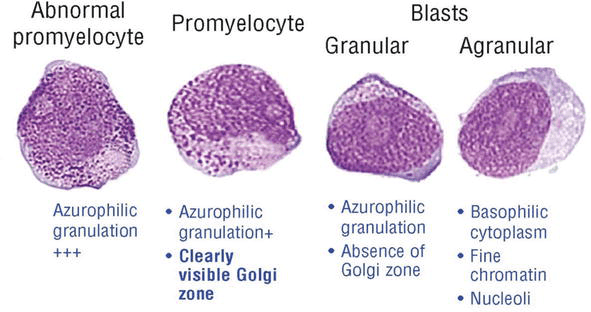
Testing for MDS includes a CBC, bone marrow biopsy, and looking at cells under a microscope.
The tests should fit the patient’s needs. This means considering their age, other health issues, and more.
Myelodysplastic Syndrome (MDS) is diagnosed differently in various age groups. Each subtype and genetic feature has its own pattern. Knowing how MDS subtypes and age are linked is key for correct diagnosis and treatment.
MDS is a complex group of disorders. Its subtypes change with age. For example, refractory anemia with ring sideroblasts (RARS) is more common in older adults. On the other hand, de novo MDS is often seen in younger patients.
Looking at how MDS subtypes vary with age can help us understand the disease better. Research shows that certain subtypes are more common in specific age groups. This reflects differences in genetic and environmental factors.
Cytogenetic abnormalities are important in diagnosing and predicting MDS outcomes. These abnormalities change with age. Older patients often have more of these, which can affect treatment and prognosis.
Common abnormalities include deletions of chromosomes 5 and 7, and trisomy 8. The type and number of these abnormalities can influence how the disease progresses and the patient’s survival.
Molecular profiling is key in understanding MDS and guiding treatments. The molecular profiles of MDS patients change with age. Certain genetic mutations are more common in specific age groups.
For example, mutations in the SF3B1 gene are more common in older MDS patients, like those with RARS. Younger patients are more likely to have mutations in genes such as RUNX1 and ASXL1.
Knowing the molecular profiles of MDS patients across different ages helps doctors tailor treatments more effectively.
Age is key in picking the right treatment for MDS patients. MDS is complex and changes with age. So, treatments must be tailored for each patient.
Treatment plans for MDS change with age and health. Younger patients might get stronger treatments like chemotherapy and stem cell transplants. Older patients might get treatments that focus on managing symptoms and improving quality of life.
A study in the Journal of Clinical Oncology shows age matters in MDS treatment. Older patients often face tougher challenges because of health issues and less tolerance to strong treatments.
“The treatment of MDS in older adults requires a careful balance between the benefits and risks of therapy.”
– Journal of Clinical Oncology
Stem cell transplants can be a cure for MDS, but age and health matter a lot. Younger patients are usually better candidates for this treatment.
| Age Group | Transplant Eligibility | Considerations |
| <60 years | High | Generally considered for transplant if healthy |
| 60-70 years | Moderate | Decided on a case-by-case basis, based on health |
| >70 years | Low | Usually not considered due to high risk of death from treatment |
Supportive care is key for MDS management, mainly for older patients or those not fit for strong treatments. It includes blood transfusions, growth factors, and managing complications.
The field of MDS treatment is growing, with new therapies and trials giving hope to patients. These include targeted treatments, immunomodulatory drugs, and other innovative methods.
As research keeps improving, age will continue to play a big role in MDS treatment. This ensures the best outcomes for patients of all ages.
Age is a big factor in how well MDS patients do. Knowing how age affects the disease and survival rates helps both patients and doctors.
MDS can progress differently in people, with age being a key factor. Older patients face a higher risk of the disease getting worse. This is because they have more genetic changes and other health issues.
A study found that getting older increases the risk of MDS. It said, “The aging process is associated with an increased risk of clonal hematopoiesis, which can evolve into MDS or other hematologic malignancies.”
“The aging bone marrow microenvironment may contribute to the development and progression of MDS.”
Survival rates for MDS patients change with age. Younger patients usually do better than older ones. Data shows that those under 60 have a much higher 5-year survival rate than those over 80.
Quality of life is key for MDS patients, but it’s even more important for older adults. It’s important to manage symptoms, reduce the need for blood transfusions, and lower treatment side effects.
Supportive care is vital. This includes blood transfusions, growth factor support, and iron chelation therapy.
Long-term monitoring is a must for MDS patients of all ages. Regular check-ups with a hematologist/oncologist are needed. This helps track the disease, adjust treatments, and handle new problems quickly.
Understanding prognosis and survival rates by age helps doctors tailor care to each patient. This improves outcomes and quality of life.
Myelodysplastic syndrome (MDS) is a complex disorder with a varied age of diagnosis. The mds diagnosis age range is broad, with incidence rates increasing significantly with age. Understanding the mds incidence by age is key for early detection and effective management.
The myelodysplastic syndrome age of diagnosis has big implications for treatment and prognosis. Older adults are more likely to be diagnosed with MDS. The disease’s progression can be more aggressive in this age group.
Recognizing the age-related trends in MDS diagnosis helps healthcare providers tailor treatment approaches. By understanding the mds diagnosis age range and its implications, patients can get more effective care. This improves their quality of life and survival rates.
Most people with MDS are diagnosed in their early 70s. This shows that MDS mainly affects older adults.
MDS is a bit more common in men. Studies show a ratio of about 1.3 men for every woman.
Yes, MDS can happen in kids and young adults, but it’s rare. Kids with MDS often have unique genetic and clinical features.
Main risk factors for MDS include being older, exposure to toxins, genetic mutations, and past treatments like chemotherapy or radiation.
Age greatly impacts MDS outcomes. Older patients face poorer outcomes due to health issues, less physical strength, and more genetic risks.
Yes, some MDS subtypes are more common in certain age groups. For example, RARS is common in older adults, while RCC is seen in kids.
Diagnosing MDS can be tough across different ages. It’s due to different symptoms, health issues, and possible diagnoses. A detailed diagnostic process, including bone marrow biopsy and genetic tests, is key for accurate diagnosis.
MDS treatments include supportive care, immunosuppressive therapy, and stem cell transplantation. The treatment choice depends on age, health, and disease type. Older patients often need more personalized and less intense treatments.
Stem cell transplantation can be a cure for MDS, but it’s limited in older adults. This is due to health issues, less physical strength, and higher treatment risks. Choosing the right patients and adapting treatments for older adults is critical.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!