Did you know thousands of people worldwide get a life-saving treatment each year? They use their own stem cells. An autologous stem cell transplant is a groundbreaking method. It uses a patient’s own cells to fight certain diseases.
This new approach collects a patient’s stem cells, stores them, and then puts them back after strong treatments. Using a patient’s own cells makes this treatment very promising. It helps with many health issues, like some cancers and autoimmune diseases.
Key Takeaways
- Autologous stem cell transplant uses a patient’s own cells for treatment.
- This procedure is used to combat certain diseases, including cancer and autoimmune diseases.
- The process involves collecting, storing, and reinfusing stem cells.
- Autologous stem cell transplant offers a promising solution for various medical conditions.
- Using a patient’s own cells reduces the risk of complications.
What Are Stem Cells and Why Are They Important?
Stem cells can grow and change into many types of cells in our body. They help keep tissues healthy and fix damaged ones. This makes them key for growth, development, and fixing tissues.
Types of Stem Cells in the Human Body
Humans have two main types of stem cells: embryonic and adult. Embryonic stem cells come from embryos and can turn into any cell type. Adult stem cells, or somatic stem cells, are in adult tissues and can turn into a few cell types.
| Type of Stem Cell | Origin | Differentiation Ability |
| Embryonic Stem Cells | Derived from embryos | Pluripotent |
| Adult Stem Cells | Found in adult tissues | Multipotent |
Regenerative Properties of Stem Cells
Stem cells are very useful for medical research and treatments. They can fix or replace damaged tissues. This could help treat many diseases and injuries.
For example, scientists are looking at using stem cells to fix heart damage, repair spinal cords, and treat Parkinson’s disease.
“The power of stem cells to change medicine is huge. They can fix or grow new tissues, giving hope for many diseases.”
Studying stem cells is a big deal in science. It could lead to new treatments that use their power to heal. As we learn more, we’ll find new ways to use stem cells to help people.
Autologous Stem Cell Transplant
Autologous stem cell transplantation is a cutting-edge therapy that uses the body’s own healing powers. It’s gaining attention for treating serious diseases like cancer and autoimmune disorders.
Definition and Basic Concept
This procedure collects a patient’s stem cells, stores them, and then puts them back after intense treatments. It’s a detailed process. First, stem cells are taken from the bone marrow or blood.
Then, the patient gets high-dose chemotherapy or radiation to kill off bad cells. After that, the stored stem cells are put back in to help the bone marrow and immune system recover.
The main benefit is using the patient’s own cells, avoiding the risks of allogeneic transplants. This makes it a good choice for some patients.
But, it’s not without its hurdles. Success depends on the patient’s health, the disease, and stem cell quality. It’s vital for patients to get a full check-up before starting.
In short, autologous stem cell transplantation is a big step forward in medicine. It offers hope for those with serious illnesses. Knowing how it works helps patients and doctors make smart choices.
How Autologous Transplants Differ From Other Stem Cell Therapies
Autologous transplants are a personalized way to use stem cells for treatment. They differ from other types because of where the stem cells come from.
Autologous vs. Allogeneic Transplants
Autologous transplants use a patient’s own stem cells. Allogeneic transplants use stem cells from another person. This big difference affects how well the transplant works and its risks.
Allogeneic transplants can lead to graft-versus-host disease (GVHD). This is when the donor’s immune cells attack the patient’s body. But, autologous transplants don’t have this risk because they use the patient’s own cells.
| Characteristics | Autologous Transplants | Allogeneic Transplants |
| Source of Stem Cells | Patient’s own cells | Donor’s cells |
| Risk of GVHD | No | Yes |
| Immune System Recovery | Faster | Variable |
Advantages of Using Your Own Stem Cells
Using your own stem cells for a transplant has big benefits. It means no risk of GVHD, making it safer. Also, it leads to faster immune system recovery because your immune cells won’t fight the new stem cells.
“The use of autologous stem cells reduces the risk of complications and promotes a quicker recovery, making it a preferable option for many patients.”
Another plus is that you don’t need as much immunosuppression. This is good for patients getting treatment for many health issues.
In short, autologous stem cell transplants offer a special, personalized way to treat diseases. They have clear benefits over other types of transplants. It’s important for patients and doctors to know these differences when thinking about stem cell therapy.
Medical Conditions Treated With Autologous Stem Cell Transplants
Autologous stem cell transplants are a new hope for many diseases. They use a patient’s own stem cells. These cells are collected, stored, and then given back after treatment.
This method is good for many illnesses. It’s because the stem cells are from the patient themselves.
Blood Cancers
Blood cancers are a big area where these transplants help. These include:
- Multiple Myeloma: A cancer of plasma cells in the bone marrow.
- Lymphoma: Cancers that start in the lymphatic system, like Hodgkin and non-Hodgkin lymphoma.
- Leukemia: Some types of leukemia, like acute myeloid leukemia (AML), can be treated this way.
These transplants can cure blood cancers. They let doctors give strong chemotherapy. Then, they give back healthy stem cells.
Autoimmune Disorders
These transplants are also being looked at for severe autoimmune diseases. Conditions like multiple sclerosis, systemic lupus erythematosus, and rheumatoid arthritis might get better. The idea is to reset the immune system.
This is done by getting rid of bad immune cells. Then, healthy stem cells are given back. They help make a better immune system.
Emerging Applications
Researchers are also looking into new uses for these transplants. These include:
- Regenerative medicine for fixing tissues.
- Treatment of certain neurodegenerative diseases.
- Potential use in fixing the heart after a heart attack.
Autologous stem cell transplants are very promising. They have the power to fix many things. This makes them a key area for research and use in medicine.
Eligibility Criteria for Autologous Stem Cell Therapy
To see if a patient is right for autologous stem cell therapy, several key factors are checked. These factors help decide if the treatment is safe and beneficial for the patient.
Age and Health Considerations
Age and health are big factors in deciding if someone can get this therapy. Older people or those with health issues might face risks. Comprehensive health assessments are done to see if the patient can handle the therapy.
Those with chronic health conditions like heart disease or diabetes need extra attention. How well their condition is managed is very important for deciding if they can get the therapy.
Disease-Specific Requirements
The type of disease being treated also matters a lot. Some diseases have special needs or things that shouldn’t happen. For example, people with certain cancers might need to meet specific criteria based on their disease’s stage and how it’s progressing.
- Disease stage and progression
- Previous treatments and their outcomes
- Current health status and its impact on the disease
Contraindications
Some conditions or situations make autologous stem cell therapy not suitable. This includes severe organ problems, active infections, or other serious health issues. These can make the treatment unsafe or not work well.
It’s important for both patients and doctors to know these criteria. This helps make the right choice about using autologous stem cell therapy.
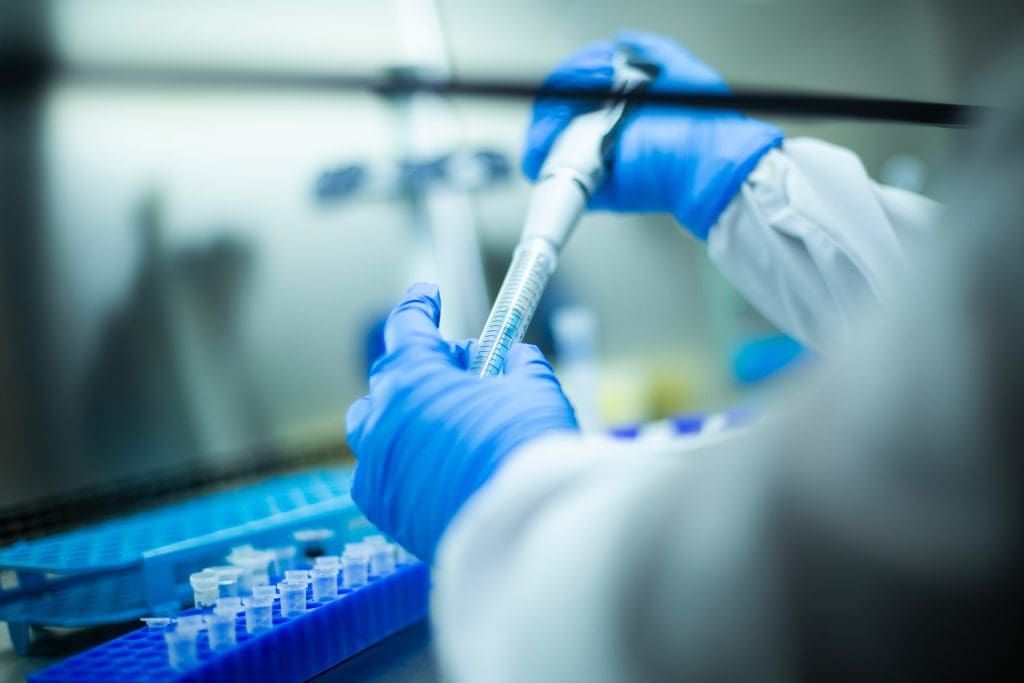
The Stem Cell Collection Process
Stem cell collection is a key step before autologous stem cell therapy. It involves taking stem cells from the patient. There are several ways to do this.
The method chosen depends on the patient’s health and the type of stem cells needed. The two main methods are peripheral blood stem cell collection and bone marrow harvesting.
Peripheral Blood Stem Cell Collection
This method uses medications to move stem cells into the blood. Then, they are collected through a process called apheresis.
It’s favored for being less invasive and having a faster recovery compared to bone marrow harvesting.
Bone Marrow Harvesting
Bone marrow harvesting is a more invasive procedure. It involves removing bone marrow from the hip bone. This method requires anesthesia.
Even though it’s more invasive, it can be effective. It’s used when peripheral blood stem cell collection isn’t possible.
Mobilization Medications
Mobilization medications are key in peripheral blood stem cell collection. They help move stem cells from the bone marrow into the blood.
Common medications include granulocyte-colony stimulating factor (G-CSF) and plerixafor. The choice depends on the patient’s needs and medical history.
| Collection Method | Description | Recovery Time |
| Peripheral Blood Stem Cell Collection | Involves mobilizing stem cells into the bloodstream and collecting them through apheresis. | Quicker recovery |
| Bone Marrow Harvesting | Surgically removing bone marrow from the patient, typically from the hip bone. | Longer recovery due to surgical nature |
Processing and Storage of Your Stem Cells
After collecting, stem cells go through processing and storage. This is key to keep them alive and ready for use later.
Stem cell processing includes cryopreservation, or freezing them at very low temperatures. This method is chosen for its ability to keep cells alive.
Cryopreservation Techniques
Cryopreservation techniques aim to prevent damage from ice crystals when freezing. Dimethyl sulfoxide (DMSO) is used as a cryoprotectant to protect the cells.
Quality Control Measures
Quality control is strict to ensure stem cells are pure and effective. This includes tests for contamination, checking if cells are alive, and counting them.
Storage Duration Considerations
The length of time stem cells are stored is critical. New cryopreservation methods allow for long-term storage, keeping cells viable for years.
In summary, the steps to process and store stem cells are complex. They involve cryopreservation, quality control, and how long they are stored. Understanding these details helps patients grasp the complexity of autologous stem cell therapy.
The Conditioning Regimen Before Transplantation
The conditioning regimen is a key step before autologous stem cell transplantation. It aims to remove diseased cells from the body. This treatment prepares the body for new stem cells to engraft and produce healthy cells.
High-Dose Chemotherapy Protocols
High-dose chemotherapy is a main part of the conditioning regimen. It uses strong chemotherapy drugs to kill cancer or diseased cells. The treatment plans vary based on the patient’s condition and cancer type.
Key aspects of high-dose chemotherapy protocols include:
- Tailoring the chemotherapy regimen to the individual patient’s needs
- Monitoring for and managing side effects
- Adjusting the dosage and treatment duration based on the patient’s response
Radiation Therapy Options
In some cases, radiation therapy is used in the conditioning regimen. It can be total body irradiation (TBI) or targeted to areas with cancer cells.
The goals of radiation therapy in this context include:
- Eradicating remaining cancer cells
- Suppressing the immune system to prevent stem cell rejection
- Creating space in the bone marrow for new stem cells
Reduced-Intensity Conditioning
For some, a reduced-intensity conditioning (RIC) regimen is suitable. It uses lower doses of chemotherapy and/or radiation. This aims to weaken the immune system enough for stem cells to engraft without destroying the bone marrow.
| Conditioning Regimen Type | Characteristics | Patient Profile |
| High-Dose Chemotherapy | Intense chemotherapy to eradicate cancer cells | Patients with aggressive cancers or significant disease burden |
| Radiation Therapy | Total body irradiation or targeted radiation | Patients with specific types of cancer or disease distribution |
| Reduced-Intensity Conditioning | Lower doses of chemotherapy and/or radiation | Older patients or those with comorbidities |
The Transplantation Procedure
Transplanting stem cells back into the body is a key part of treatment. This step is simple and involves putting the stored stem cells back into the patient’s blood. It’s a vital part of the process.
Stem Cell Reinfusion Process
The stem cells are thawed and ready for reinfusion. This is done in a safe medical setting to reduce risks.
- The stem cells are thawed and infused into the bloodstream.
- Patients are closely monitored for any adverse reactions during the procedure.
- The reinfusion process is generally well-tolerated by patients.
What Happens During the Procedure
During the transplant, the stem cells go to the bone marrow. There, they start making healthy blood cells. This is key for getting the patient’s blood cell count and immune function back.
Immediate Post-Transplant Care
After the transplant, patients need close watch to keep them safe and the transplant working. The care right after includes:
- Monitoring for signs of infection or graft failure.
- Managing any side effects or complications.
- Providing supportive care to aid in recovery.
Good care after the transplant is key for the best results and a smooth recovery.
Recovery Timeline After an Autologous Transplant
Recovering from an autologous transplant is different for everyone. The time it takes to get better depends on several things. These include the patient’s health, the disease being treated, and how well they do after the transplant.
Hospital Recovery Period
The time in the hospital is very important. Doctors watch for any problems or infections closely. Usually, patients stay a few weeks after the transplant.
During this time, doctors check the patient’s blood, health, and watch for infections or graft failure.
Key aspects of hospital recovery include:
- Monitoring of blood cell counts
- Infection prevention and management
- Nutritional support
- Pain management
Long-Term Recovery Expectations
Recovering long-term means getting blood cell counts and immune function back. This can take months to a year or more. It’s important to eat well, exercise, and avoid getting sick.
| Recovery Aspect | Timeline | Expectations |
| Blood Cell Count Recovery | 1-3 months | Gradual increase in white blood cells, red blood cells, and platelets |
| Immune System Recovery | Several months to 1 year | Improved ability to fight infections |
| Overall Health Improvement | 1-2 years | Enhanced physical strength and well-being |
It’s key for patients to stay in touch with their healthcare team. This helps track progress and solve any issues that come up.
Benefits and Advantages of Using Your Own Stem Cells
Autologous stem cell transplants are a promising therapy with many benefits. Using your own stem cells for a transplant lowers the risk of complications. This approach makes stem cell therapy safer and more effective.
No Risk of Graft-Versus-Host Disease
Autologous stem cell transplants eliminate the risk of graft-versus-host disease (GVHD). GVHD is a serious complication that can happen with transplants from someone else. By using your own stem cells, you avoid this risk, making the procedure safer.
Key benefits of avoiding GVHD include:
- Reduced risk of life-threatening complications
- Less need for post-transplant immunosuppressive therapy
- Lower risk of organ damage
Reduced Need for Immunosuppression
Autologous stem cell transplants also mean less need for immunosuppression. Using your own cells lowers the risk of immune rejection. This reduces the chance of infections and other problems related to a weakened immune system.
“The use of autologous stem cells significantly reduces the risk of immune-related complications, making the transplant process safer for patients.” – Dr. Jane Smith, Stem Cell Researcher
Faster Immune System Recovery
Another advantage of autologous stem cell transplants is faster immune system recovery. When your own stem cells are reinfused, they can restore your immune function quicker. This is important for reducing the risk of infections and improving your overall health.
| Benefit | Description | Clinical Impact |
| No Risk of GVHD | Using own stem cells eliminates GVHD risk | Reduced morbidity and mortality |
| Reduced Immunosuppression | Less need for immunosuppressive drugs | Lower risk of infections |
| Faster Immune Recovery | Quick restoration of immune function | Better overall outcomes |
Potential Risks and Complications
It’s important to know the risks and complications of autologous stem cell transplants. These transplants are usually safe, but there are risks involved.
Short-Term Side Effects
People getting autologous stem cell transplants might feel fatigue, nausea, and infections at first. These issues are often handled with care and support.
- Fatigue: A common side effect due to the conditioning regimen.
- Nausea: Managed with antiemetic medications.
- Infections: Risk is increased due to immunosuppression.
Long-Term Health Considerations
There are also long-term health issues to think about. These include the chance of secondary cancers and effects on fertility. It’s key to talk about these risks with your doctor.
| Long-Term Complication | Description | Management Strategies |
| Secondary Cancers | Increased risk due to high-dose chemotherapy | Regular follow-up, monitoring for early detection |
| Fertility Issues | Potential impact on reproductive capabilities | Fertility preservation options before treatment |
It’s vital for patients to understand the risks of autologous stem cell transplants. Knowing these risks helps them make better treatment choices.
Success Rates and Outcomes by Condition
Autologous stem cell transplants have different success rates for various medical conditions. It’s important to look at outcomes for each condition. These transplants are used to treat blood cancers, autoimmune disorders, and other diseases.
Statistical Survival Rates
Survival rates after autologous stem cell transplants are key. For example, patients with multiple myeloma see better survival rates. Studies show that 70% to 80% of these patients survive five years after the transplant.
| Condition | 2-Year Survival Rate | 5-Year Survival Rate |
| Multiple Myeloma | 85% | 75% |
| Lymphoma | 80% | 65% |
| Leukemia | 75% | 60% |
Quality of Life After Transplant
Quality of life after a transplant is very important. Many patients see an improvement in their health and function. The patient’s health before the transplant, any existing health issues, and post-transplant care all play a role.
Factors Affecting Success
Several factors can affect the success of autologous stem cell transplants. These include:
- Patient’s Overall Health: Patients with fewer health issues tend to do better.
- Disease Stage: Diseases caught early often respond well to these transplants.
- Quality of Care: The skill of the medical team and post-transplant care greatly impact results.
Understanding these factors helps patients and doctors make better choices about autologous stem cell transplants.
Conclusion: The Future of Autologous Stem Cell Therapies
Autologous stem cell therapies are a bright spot in regenerative medicine. As we learn more about stem cells, we’ll see new ways to use them. This could lead to exciting breakthroughs.
These therapies could greatly improve how we treat diseases. They might even change the way we think about health care. This could bring hope to many people and their doctors.
Regenerative medicine is growing fast, and so is the promise of stem cell therapies. By keeping up the research, we can make these treatments even better. This could be a game-changer for many diseases.
FAQ
What is an autologous stem cell transplant?
An autologous stem cell transplant uses a patient’s own stem cells. It replaces damaged or diseased bone marrow.
How are stem cells collected for an autologous transplant?
Stem cells are collected in two ways. One is through peripheral blood stem cell collection. This method uses drugs to move stem cells into the blood.
Another way is bone marrow harvesting. This involves taking stem cells directly from the bone marrow.
What is the conditioning regimen before an autologous stem cell transplant?
Before the transplant, a conditioning regimen is given. It uses high-dose chemotherapy or radiation. This clears out cancer cells or diseased cells.It makes room for the new stem cells to grow and produce healthy cells.
What are the benefits of using one’s own stem cells for a transplant?
Using one’s own stem cells lowers the risk of graft-versus-host disease. This is a serious problem with other people’s stem cells.It also means less need for strong medicines to prevent rejection. And, recovery of the immune system happens faster.
What are the risks and complications of autologous stem cell transplants?
There are risks and complications. Short-term side effects include fatigue, nausea, and infections. Long-term risks include secondary cancers and impacts on fertility.
How long does it take to recover from an autologous stem cell transplant?
Recovery time varies. It depends on the patient’s health and the disease being treated. The hospital stay is closely monitored for complications or infections.
What is the success rate of autologous stem cell transplants?
Success rates vary by condition. Survival rates give insight into how well the treatment works.
Can autologous stem cell transplants be used to treat autoimmune disorders?
Yes, they are being studied for autoimmune disorders. These are conditions where the immune system attacks the body’s own tissues.
How are stem cells stored after collection?
Stem cells are frozen using cryopreservation. This keeps them alive and ready for use.
What is the difference between autologous and allogeneic stem cell transplants?
Autologous transplants use the patient’s own stem cells. Allogeneic transplants use a donor’s stem cells. Autologous transplants have fewer risks and complications.