Last Updated on November 27, 2025 by Bilal Hasdemir
Ionizing radiation, like X-rays and gamma radiation, is known to cause cancer. It can damage DNA, which might lead to cancer. In some cases, prolonged or unnecessary exposure can increase the risk of cancer from xray and other ionizing sources.
At Liv Hospital, patient safety is our main goal. X-rays and gamma radiation can harm DNA, causing serious damage. Our medical team ensures that every imaging test is performed only when necessary to minimize any potential risk, including the risk of cancer from X-ray exposure.
It’s important for patients to know about the risks of ionizing radiation. This is true for tests that use X-rays and gamma radiation. Patients should think if these tests are really needed and talk to their doctors about any worries regarding cancer from X-ray or radiation safety.
Key Takeaways
- Ionizing radiation, including X-rays and gamma radiation, is a recognized human carcinogen.
- Exposure to ionizing radiation can cause DNA damage, potentially leading to cancer.
- Diagnostic tests involving X-rays and gamma radiation should be used judiciously.
- Patient safety is a top priority at healthcare facilities like Liv Hospital.
- Understanding the risks associated with ionizing radiation is critical for patients.
The Nature of Ionizing Radiation

Ionizing radiation affects living things in complex ways. It involves high-energy particles hitting biological tissues. This includes alpha (α), beta (β), and gamma (γ) radiation, X-rays, and positrons. All can harm living cells.
Physical Properties of X-Rays and Gamma Rays
X-rays and gamma rays are types of electromagnetic radiation. They have lots of energy and short wavelengths. This lets them go through many materials, like human tissue.
The main difference is where they come from. X-rays are made when electrons change states. Gamma rays come from changes in the nucleus of an atom.
How Ionizing Radiation Interacts with Human Tissue
Ionizing radiation interacts with human tissue in two ways: excitation and ionization. Ionization is more serious. It can create free radicals that damage DNA and other cell parts.
The risk of getting cancer from radiation depends on the dose. More radiation means a higher chance of genetic changes that can cause cancer. Knowing how radiation works helps us understand its risks.
| Characteristics | X-Rays | Gamma Rays |
| Origin | Electron transitions | Nuclear transitions |
| Energy Level | Variable, generally lower than gamma rays | High |
| Penetration Power | Moderate | High |
Understanding Cancer From X-Ray and Other Radiation Sources

Ionizing radiation, like X-rays, can harm DNA in cells, possibly causing cancer. High levels of exposure are clearly linked to more cancer, as this radiation creates many DNA lesions.
DNA Damage Mechanisms
Ionizing radiation can damage DNA in two ways. Direct effects happen when radiation directly ionizes DNA, causing breaks in DNA strands. Double-strand breaks are very harmful because they can lead to genetic mutations if not fixed right.
The indirect effects involve radiation ionizing water molecules around DNA, creating free radicals that damage DNA. This can cause different types of DNA damage, like base damage and single-strand breaks.
Mutation and Carcinogenesis Pathways
When DNA damage isn’t fixed right, it can cause mutations. These mutations can mess up normal cell functions, possibly leading to cancer. The process of making cancer involves several steps: initiation, promotion, and progression.
Initiation happens when a cell mutates, giving it a growth advantage. Promotion is when initiated cells grow more, and progression is when more genetic changes happen, leading to cancer.
Knowing these steps is key to understanding the cancer risk from radiation exposure, like from X-rays and other sources.
Dose-Response Relationship in Radiation Exposure
It’s important to know how radiation affects the body. This is key to understanding cancer risk. The dose-response relationship helps us see how radiation can harm us.
Measuring Radiation Doses: Sieverts and Gray Units
Radiation doses are measured in Gray (Gy) and Sievert (Sv). The Gray shows how much radiation energy is absorbed by the body. One Gray is one joule of radiation energy per kilogram of matter.
The Sievert, on the other hand, considers the type of radiation and its power. It’s used to measure the effective dose. This helps us understand the biological effects of different types of radiation.
For example, X-rays or gamma radiation doses are adjusted to Sieverts. This shows their biological harm. Most medical imaging uses very low doses, often in millisieverts (mSv). One mSv is 0.001 Sv.
Acute vs. Chronic Exposure Effects
Radiation’s impact on health changes with acute or chronic exposure. Acute exposure is a high dose over a short time. It can cause immediate health problems, like radiation sickness.
Chronic exposure is lower doses over a long time. It can lead to long-term risks, like cancer. The dose, duration, and number of exposures affect health.
Understanding these differences is key to assessing cancer risk. For example, patients getting repeated imaging need to consider the total dose over time.
The Linear No-Threshold (LNT) Model and Its Implications
The Linear No-Threshold (LNT) model says any radiation dose, no matter how small, can cause cancer risk. This idea is the basis for radiation protection rules all over the world.
Scientific Basis and Historical Development
The LNT model is simple. It says the risk of cancer from radiation is directly tied to the dose, with no safe level. Studies, like those on Hiroshima and Nagasaki survivors, support this model.
The LNT model’s history is linked to the growth of radiation safety policies. It was first used as a safe approach to radiation. Now, it’s key in setting limits for workers and the public.
Key aspects of the LNT model include:
- Direct proportionality between radiation dose and cancer risk
- No threshold dose below which risk is considered zero
- Application in setting radiation protection standards
Regulatory Applications in Radiation Protection
The LNT model helps set dose limits for work exposure. It also guides safety rules in radiation-related industries.
Groups like the Nuclear Regulatory Commission (NRC) in the U.S. use the LNT model. They set rules to reduce radiation exposure. This includes rules for nuclear plants, medical use of radiation, and industries with radioactive materials.
The LNT model’s effects also reach public health policy. It shapes how communities are protected in nuclear accidents or emergencies.
Historical Evidence of Radiation Carcinogenesis
Ionizing radiation’s role in cancer has been shown through major events. These events have given us key data on radiation’s health effects.
Survivor Studies from Hiroshima and Nagasaki
The atomic bombings in Hiroshima and Nagasaki in 1945 exposed many to radiation. The Life Span Study (LSS) on survivors has helped us understand radiation’s long-term health effects. It shows a clear link between radiation doses and cancer rates.
“The LSS cohort has provided the most detailed data on radiation’s health effects, a key for assessing radiation risks.”
Nature Reviews Cancer
Looking closely at the LSS data, we see a strong link between radiation and cancer risk. This is true for cancers like leukemia, breast, and thyroid.
| Cancer Type | Excess Relative Risk per Sv |
| Leukemia | 2.51 |
| Breast Cancer | 1.23 |
| Thyroid Cancer | 1.17 |
Nuclear Industry Worker Cohort Data
Studies on nuclear industry workers have also shown radiation’s health effects. These workers have been monitored for decades, giving us insights into radiation risks at work.
Key findings from nuclear worker studies include:
- Increased risk of leukemia and other cancers of the blood
- Higher rates of solid cancers like lung and breast cancer
- Risk varies with dose rate and how long one is exposed
Chernobyl and Fukushima Aftermath
The nuclear accidents at Chernobyl in 1986 and Fukushima in 2011 released radioactive material. This exposed many to ionizing radiation. The health effects of these accidents have been studied a lot.
The rise in thyroid cancer among children exposed to radioactive iodine from Chernobyl is a clear example of radiation-induced cancer. Studies are also looking at the long-term health effects of Fukushima residents and workers.
These events highlight the need to understand radiation carcinogenesis to lessen its health impacts.
Medical Diagnostic X-Rays and Cancer Risk
The link between medical X-rays and cancer is complex. It depends on the dose of radiation and how likely a person is to get cancer. Knowing this helps us understand the good and bad sides of using X-rays for tests.
Typical Radiation Doses from Common Procedures
X-rays are a key tool in medicine, used for many tests. The doses from these tests vary a lot. For example, a chest X-ray gives about 0.1 millisieverts (mSv), while a CT scan of the abdomen and pelvis can give around 10 mSv.
For comparison, we all get about 3 mSv of background radiation each year from nature.
Common Diagnostic Procedures and Their Doses:
- Chest X-ray: 0.1 mSv
- Mammogram: 0.4 mSv
- CT scan (abdomen and pelvis): 10 mSv
- Barium enema: 15 mSv
These doses are low, and the chance of getting cancer from them is small. But, getting many tests over time can be a worry, more so for younger people.
Population-Based Studies on Diagnostic Imaging
Big studies have looked at how X-rays might raise cancer risk. They compare patients who have had many tests to the general population. Some studies found a slight increase in cancer risk, but others didn’t see a big difference.
It’s hard to figure out the exact doses and other risks in these studies. But, most agree that the good from these tests is more than the bad, when used right.
The importance of justification and optimization in diagnostic imaging cannot be overstated. It’s key to make sure each test is really needed and doses are as low as possible (ALARA) to lower risks.
Pediatric Patients and Elevated Cancer Risk Concerns
Radiation exposure in pediatric patients is a big worry because it raises cancer risk. Kids are more at risk because their bodies are growing and they have more years to face radiation’s effects.
Biological Sensitivity Factors in Children
Children are very sensitive to radiation because of their fast-growing cells and developing tissues. This makes them more likely to suffer from radiation’s harmful effects, like X-rays and gamma rays.
Getting exposed to radiation for a long time, or many times, can be even riskier for kids. Their growing bodies are more likely to get damaged by radiation, leading to genetic changes and a higher cancer risk.
Long-Term Risk Projections and Monitoring
Looking at the long-term risks for kids exposed to radiation means checking if they might get cancer later. It’s important to keep an eye on them and catch any health problems early.
Research shows that kids who have many CT scans or other imaging tests face a higher cancer risk. So, it’s key to think carefully about the need for imaging tests and use the least amount of radiation needed.
By knowing how radiation affects kids and finding ways to lower their exposure, doctors can help reduce the risks of cancer from radiation.
Occupational Radiation Exposure and Cancer Surveillance
Workers in certain jobs face a big risk from radiation. They get exposed to different levels of radiation. This can raise their chance of getting cancer.
Healthcare Workers and Radiologists
Healthcare workers, like radiologists, face radiation risks during their work. Radiologists are at high risk because they often use X-rays and other imaging tech. They might get cancers like leukemia and brain cancer more often.
“Radiologists and other healthcare workers who use radiation in their practice are at increased risk of cancer, highlighting the need for strict radiation safety protocols.”
A study in the Journal of the American College of Radiology found something scary. Radiologists who started working before 1950 face a much higher cancer risk than other doctors.
| Occupation | Average Annual Radiation Dose (mSv) | Cancer Risk |
| Radiologists | 0.5-1.0 | Higher risk of leukemia and brain cancer |
| Nuclear Medicine Technologists | 1.0-2.0 | Increased risk of thyroid cancer |
Nuclear Industry Personnel
People working in the nuclear industry face radiation risks. Workers in nuclear power plants and research facilities are at risk. They might get cancers like lung cancer and leukemia more often.
Airline Crew and Cosmic Radiation
Airline crew members get cosmic radiation on long flights. This radiation is a big worry for them, as it can increase cancer risk. They might get cancers like melanoma and breast cancer more often.
It’s very important to watch for cancer in these high-risk jobs. Regular health checks can catch cancer early. This can help improve treatment chances.
Cumulative Effects of Multiple Radiation Exposures
It’s key to know how radiation adds up over time to understand health risks. Getting exposed to radiation more than once can up the chance of getting cancer. So, it’s important to keep track of how much radiation someone gets over their lifetime, mainly for those who need lots of imaging tests.
Tracking Lifetime Radiation Dose
For people who get lots of imaging tests, keeping a record of all radiation doses is a must. This includes X-rays and other tests. Keeping these records helps doctors see the total risk and decide if more tests are needed.
A study in the National Center for Biotechnology Information shows why tracking radiation is so important. It stresses the need to watch and manage how much radiation people get over time.
Risk Assessment for Patients Requiring Repeated Imaging
Those who need lots of imaging tests face a bigger risk of getting too much radiation. Doctors look at their medical history, how often they get tests, and how much radiation they get. This helps doctors find ways to lower radiation exposure without losing the test’s usefulness.
The table below shows what doctors consider when assessing risk for those needing lots of imaging:
| Factor | Description | Impact on Risk |
| Medical History | Previous medical conditions and treatments | High |
| Imaging Frequency | Number of imaging procedures over time | High |
| Radiation Dose | Amount of radiation received per procedure | High |
| Alternative Modalities | Use of non-ionizing imaging alternatives | Low |
Understanding these factors helps doctors find ways to lower radiation exposure. They might use different imaging methods, make tests more efficient, or only do tests when really needed.
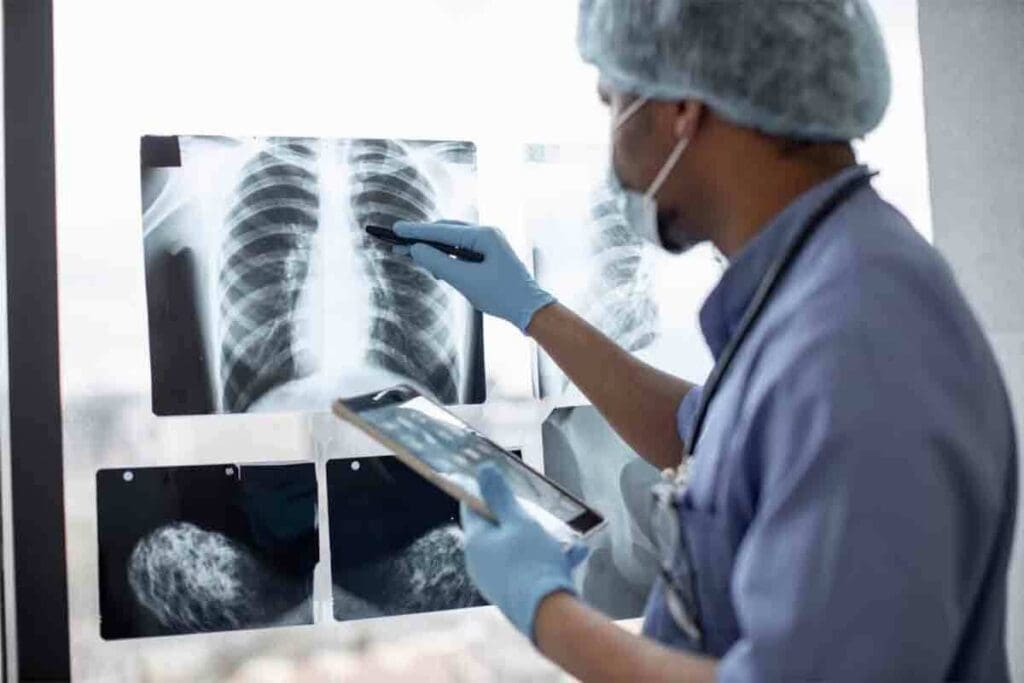
Risk-Benefit Analysis in Medical Imaging
Medical imaging is key for diagnosing and treating diseases. But, we must balance its benefits against the risks of radiation. It’s important to make sure patients get the right info without harm.
Justification Criteria for Radiological Procedures
Deciding if a radiological procedure is needed is based on weighing its benefits against risks. We look at other ways to diagnose and if the imaging will help in treating the patient.
Justification criteria include:
- The clinical condition of the patient
- The availability of alternative diagnostic techniques
- The chance for the imaging to improve patient outcomes
The International Commission on Radiological Protection (ICRP) says, “The use of ionizing radiation for medical purposes should be justified by the expectation that it will improve the health or well-being of the individual patient.”
The ALARA Principle in Clinical Practice
The ALARA principle means keeping radiation doses as low as possible. This is key in protecting patients from radiation.
| Principle | Description | Application in Medical Imaging |
| ALARA | Minimize radiation dose | Optimize imaging protocols, use dose-reduction technologies |
| Justification | Ensure benefits outweigh risks | Use alternative imaging when possible, justify each procedure |
Following the ALARA principle means using new tech and good judgment. This helps keep radiation doses low.
By using the right criteria and following ALARA, doctors can make imaging safer. This way, patients get the most benefit with the least risk.
Technological Advances Reducing Radiation Exposure
New technologies in medical imaging are changing the game by cutting down on radiation doses. This change comes from better low-dose imaging and new non-ionizing methods instead of X-rays.
Low-Dose Imaging Protocols
Today’s CT scanners and X-ray machines have smart software for low-dose imaging protocols. These adjust the dose based on the patient’s size and what’s needed for the scan, lowering exposure a lot.
Using low-dose protocols is now common in many radiology departments. For example, iterative reconstruction techniques help keep image quality high while cutting the dose.
| Technology | Description | Radiation Reduction |
| Iterative Reconstruction | Technique that improves image quality | Up to 50% |
| Low-Dose CT Scanners | Scanners designed to minimize radiation | Up to 70% |
| Digital X-Ray | Direct digital capture of X-ray images | Up to 90% |
Non-Ionizing Alternatives to X-Rays
There’s also a big move towards non-ionizing imaging modalities like ultrasound and MRI. These options are safer because they don’t use ionizing radiation, which is great for patients needing many scans.
Ultrasound has gotten much better, giving clear images without radiation. MRI, though not for every case, shows detailed inside pictures without ionizing radiation.
Thanks to better hardware and software, these new technologies are being used more in clinics. This makes imaging safer and more precise.
Conclusion: Contextualizing Radiation Risk in Modern Medicine
Understanding radiation risk is key for making smart choices in medicine. We must weigh the risks of cancer from radiation against the benefits of medical treatments. Many patients don’t fully grasp the risks of radiation from tests like CT scans and X-rays.
A study showed that only 22% of patients knew CT scans can increase cancer risk. And 88% thought the risk was lower than it actually is. This highlights the need for better communication about radiation risks and benefits.
By understanding the risks and benefits, patients and doctors can make better choices. The data shows we need to talk more about radiation risks. This way, we can give patients the care they need while keeping radiation exposure low.
As medical technology gets better, we must stay up to date on radiation risks and benefits. This approach helps create a safer, more informed medical environment. It also helps reduce radiation risks and improve health outcomes for patients.
FAQ
Do X-rays cause cancer?
X-rays are a type of ionizing radiation. They can damage DNA and might lead to cancer. But, the risk is usually low for most medical scans.
How do X-rays and gamma radiation contribute to cancer risk?
X-rays and gamma radiation can damage DNA, leading to mutations and cancer. The risk depends on how much and for how long you’re exposed.
What is the Linear No-Threshold (LNT) model, and how does it relate to radiation exposure?
The LNT model says there’s no safe level of radiation. Even small amounts can increase cancer risk. It helps set rules for radiation safety.
Are children more sensitive to radiation from X-rays?
Yes, kids are more vulnerable to X-rays. Their bodies are growing, and they have more years to develop cancer from radiation.
How can cumulative radiation exposure be managed?
To manage radiation exposure, keep track of total doses over time. Use safer imaging when you can. Follow the ALARA principle to lower doses.
What is the ALARA principle in clinical practice?
The ALARA principle means using the least amount of radiation needed. It helps keep patients and staff safe by using the lowest dose possible.
Can gamma radiation cause cancer?
Yes, gamma radiation can cause DNA damage and lead to cancer, just like X-rays.
How are radiation doses measured?
Doses are measured in Sieverts (Sv) and Gray (Gy). These units show how much radiation is absorbed and its effects on the body.
What are the risks associated with occupational radiation exposure?
People in jobs like healthcare and nuclear work face radiation risks. It’s important to monitor and control their exposure to prevent cancer.
Are there non-ionizing alternatives to X-rays?
Yes, non-ionizing methods like ultrasound and MRI are safer alternatives. They can replace X-rays for some tests, reducing radiation exposure.
How do low-dose imaging protocols reduce radiation exposure?
Low-dose protocols adjust X-ray settings to use less radiation. This keeps image quality high while lowering patient exposure.
Can repeated X-ray exposures increase cancer risk?
Yes, getting X-rays often can add up radiation doses. It’s key to manage and justify each exposure to lower cancer risk.
What is the justification criteria for radiological procedures?
Justification criteria check if the benefits of a scan outweigh the risks. This ensures exposures are kept as low as possible.
Reference
- American Cancer Society. (2022, November 3). Do X-rays and Gamma Rays Cause Cancer? https://www.cancer.org/cancer/risk-prevention/radiation-exposure/x-rays-gamma-rays/do-xrays-and-gamma-rays-cause-cancer.html