Last Updated on November 26, 2025 by Bilal Hasdemir

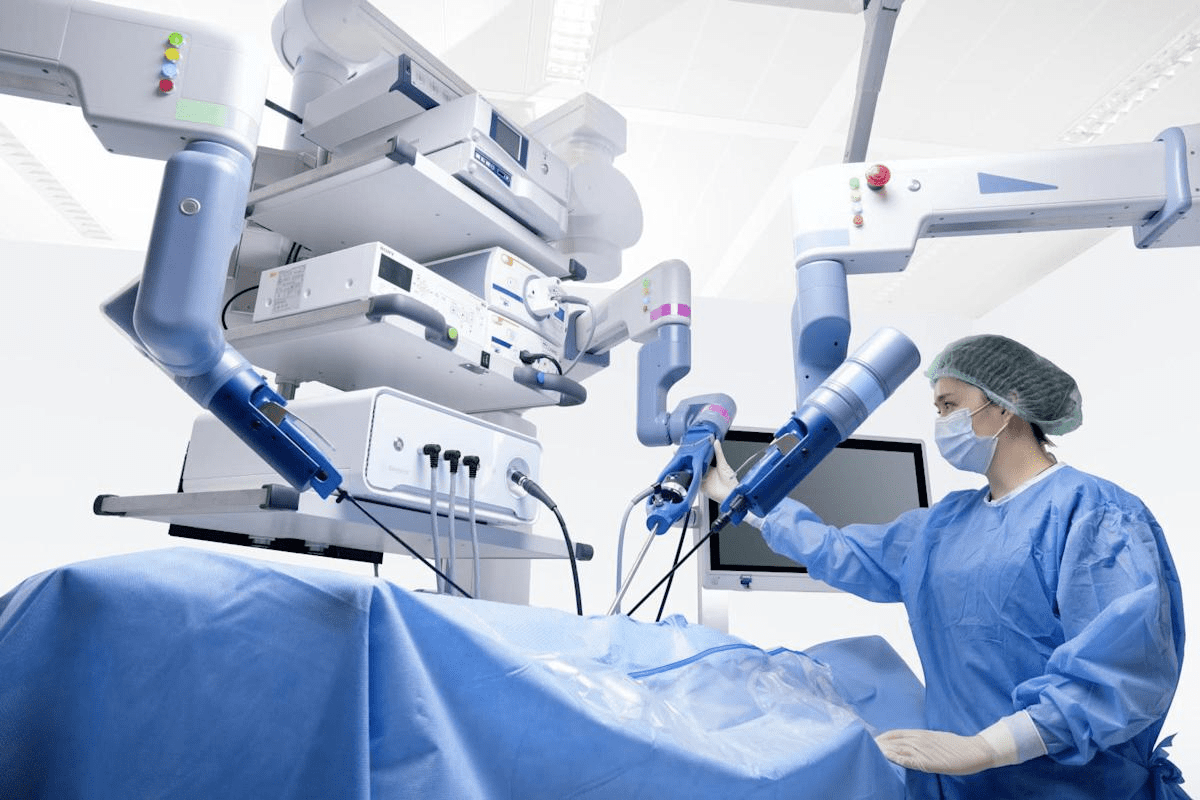
At Liv Hospital, we know cancer therapy is complex. After primary cancer therapy, like surgery, more care is needed to stop cancer from coming back. That’s where adjuvant therapy steps in.
Adjuvant therapy is key in cancer care. It aims to get rid of any cancer cells left after the first treatment. This helps lower the chance of cancer coming back, giving patients hope and confidence.
Key Takeaways
- Adjuvant therapy is given after primary treatment to reduce cancer recurrence risk.
- It is a critical component of cancer care, aimed at eliminating remaining cancer cells.
- Adjuvant therapy improves patient outcomes and reduces the risk of cancer recurrence.
- Liv Hospital’s internationally recognized team provides complete care using adjuvant therapy.
- Adjuvant therapy is a modern medical approach designed to prevent recurrence and improve outcomes.
What Is Adjuvant Treatment Definition in Oncology?
Adjuvant therapy is a cancer treatment given after the main treatment to lower the chance of cancer coming back. It’s a key part of oncology, helping to make main treatments work better.
The Fundamental Concept of Post-Primary Therapy
Adjuvant treatment is given after the main treatment, like surgery, to kill any cancer cells left behind. This is because even after main treatment, tiny cancer cells might stay, which could cause cancer to come back.
This therapy targets these leftover cells to lower the chance of cancer returning. It helps improve patient outcomes and survival rates. The choice to use adjuvant therapy depends on the cancer type and stage, and the patient’s health.
Distinguishing Adjuvant from Neoadjuvant and Palliative Care
It’s important to know the difference between adjuvant therapy and other cancer treatments, like neoadjuvant and palliative care. Neoadjuvant therapy is given before main treatment to make tumors smaller, making them easier to remove. Adjuvant therapy, on the other hand, is given after main treatment.
Palliative care is about easing symptoms and stress of cancer, not treating the cancer itself. While it’s vital for improving life quality, adjuvant therapy is focused on stopping cancer from coming back.
Knowing the differences between these therapies helps patients and doctors make better choices about cancer treatment. It shows how important adjuvant therapy is in treating cancer fully.
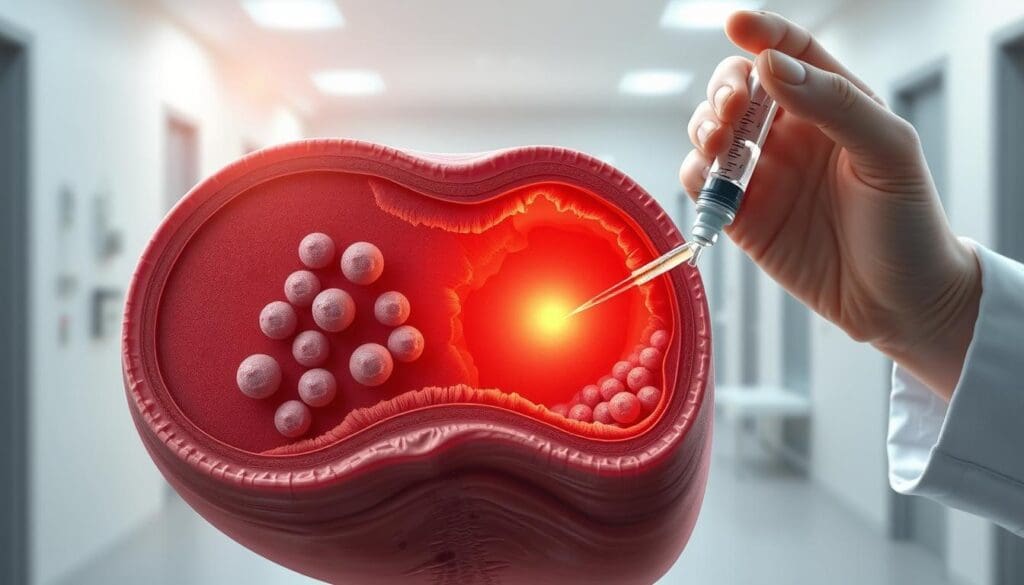
Key Fact #1: Adjuvant Therapy Targets Microscopic Disease
Adjuvant therapy is key in cancer treatment. It targets microscopic disease left after primary treatment. Even after main treatments like surgery, microscopic cancer cells might spread. These cells, called micrometastases, can grow into new tumors.
Understanding Micrometastases and Residual Cancer Cells
Micrometastases are tiny cancer cells that break off and spread. They’re too small for CT scans or MRIs to find. Residual cancer cells stay at the original tumor site after treatment. Both can cause cancer to come back if not treated.
Why Imaging Cannot Detect These Cancer Remnants
Imaging tests can’t find microscopic disease well. They can’t spot tiny cancer cell clusters. So, even if a patient seems cancer-free, microscopic disease might be there. Adjuvant therapy aims to find and treat these hidden cells.
Let’s look at how adjuvant therapy works:
| Cancer Type | Risk of Micrometastases | Adjuvant Therapy Benefit |
|---|---|---|
| Breast Cancer | High | Significant reduction in recurrence |
| Colorectal Cancer | Moderate to High | Improved survival rates |
| Lung Cancer | High | Reduced risk of distant recurrence |
The table shows adjuvant therapy’s benefits. It targets microscopic disease in many cancers. Knowing about micrometastases and residual cancer cells highlights adjuvant therapy’s role in cancer care.
Key Fact #2: The 5 Major Types of Adjuvant Cancer Treatments
There are many ways to fight cancer with adjuvant treatments. These treatments are given after the main treatment to stop cancer from coming back. Each type targets different parts of cancer biology.
We use different treatments to meet each patient’s needs. Knowing about these treatments helps patients make better choices for their care.
Chemotherapy: Systemic Elimination of Cancer Cells
Chemotherapy is key in fighting cancer, mainly for cancers at high risk of spreading. It uses drugs to kill any cancer cells left behind.
Radiation Therapy: Localized Treatment Approach
Radiation therapy is also vital, focusing on the area where cancer is. It uses rays to kill any cancer cells left in the tumor area, lowering the chance of cancer coming back.
Hormone Therapy: Blocking Cancer Growth Signals
Hormone therapy is effective for cancers that grow because of hormones. It stops the body’s hormones from helping cancer grow, slowing down cancer cell growth.
Targeted Therapies: Precision Medicine in Action
Targeted therapies are a more precise way to fight cancer. They aim at specific things in cancer cells that make them grow, giving a more focused treatment.
Choosing the right treatment depends on many things. These include the cancer type and stage, and the patient’s health. Knowing these helps us give the best treatment for each person.
| Treatment Type | Mechanism of Action | Primary Use |
|---|---|---|
| Chemotherapy | Systemic elimination of cancer cells | Cancers with high risk of systemic recurrence |
| Radiation Therapy | Localized killing of cancer cells | Local control of cancer |
| Hormone Therapy | Blocking cancer growth signals | Hormone receptor-positive cancers |
| Targeted Therapies | Precision targeting of cancer abnormalities | Cancers with specific molecular targets |
Key Fact #3: Adjuvant Chemotherapy’s Specific Role in Cancer Care
Adjuvant chemotherapy is a key part of cancer treatment. It targets tiny cancer cells left after the first treatment. This helps lower the chance of cancer coming back.
How Cytotoxic Drugs Work in the Adjuvant Setting
Cytotoxic drugs are the main part of adjuvant chemotherapy. They stop cancer cells from growing by messing with their DNA. These drugs are given after the first treatment to kill any cancer cells left behind.
Mechanism of Action: These drugs attack fast-growing cells, like cancer cells. This stops tumors from getting bigger. It also lowers the chance of cancer coming back.
Common Regimens and Their Selection Criteria
Choosing the right adjuvant chemotherapy depends on many things. These include the cancer type, its stage, and the patient’s health and wishes. Common treatments mix drugs like anthracyclines, taxanes, and platinum-based compounds.
- Cancer Type: Different cancers do better with certain drugs.
- Patient Health: How well the patient can handle certain drugs is important.
- Biomarkers: Some biomarkers help pick the right treatment.
Measuring Efficacy in Reducing Relapse Risk
How well adjuvant chemotherapy works is shown by how it lowers cancer coming back. Studies and trials have proven it can improve survival rates and lower recurrence in many cancers.
Survival Analysis: Survival analysis is used to see how well adjuvant chemotherapy works. It compares results between treated and untreated groups.
Understanding adjuvant chemotherapy’s role in cancer care shows its importance in treatment plans.
Key Fact #4: Cancer Types Most Benefiting from Adjuvant Treatment
Adjuvant treatment is key in fighting many cancers, helping patients live longer. Each cancer type reacts differently to this treatment. It’s vital to know how it helps each one.
Breast Cancer: Protocols and Personalized Approaches
Breast cancer often gets better with adjuvant treatment. We create special plans for each patient, based on their cancer details. This might include chemotherapy, hormone therapy, or targeted therapy to lower the chance of cancer coming back.
Colorectal Cancer: Stage-Specific Recommendations
For colorectal cancer, treatment depends on the cancer’s stage. Stage III colon cancer usually gets chemotherapy to kill any left-over cancer cells. We also consider treatment for high-risk stage II patients. The right chemotherapy depends on the patient’s health and the cancer’s specifics.
Lung Cancer: Tailored Post-Surgical Strategies
Lung cancer patients, mainly those with non-small cell lung cancer (NSCLC), might get adjuvant therapy after surgery. We choose treatments based on the cancer’s stage and molecular details. Often, chemotherapy is used, and sometimes targeted therapy or immunotherapy is recommended.
Other Cancers Responsive to Adjuvant Therapy
Other cancers like ovarian, gastric, and some sarcomas can also benefit from adjuvant treatment. We decide on treatment based on clinical trials, the cancer type, stage, and the patient’s health.
| Cancer Type | Common Adjuvant Treatments | Factors Influencing Treatment |
|---|---|---|
| Breast Cancer | Chemotherapy, Hormone Therapy, Targeted Therapy | Hormone Receptor Status, HER2 Expression |
| Colorectal Cancer | Chemotherapy | Stage, Tumor Characteristics |
| Lung Cancer (NSCLC) | Chemotherapy, Targeted Therapy, Immunotherapy | Stage, Molecular Characteristics |
Knowing how adjuvant therapy helps different cancers lets us give more personalized care. Our care is based on the latest research and tailored to each patient’s needs.
Key Fact #5: Timing and Duration Considerations
The timing and length of adjuvant therapy are key to success. It’s not a one-size-fits-all solution. Each cancer type and patient needs a custom plan.
The Critical Window for Treatment Initiation
Starting adjuvant therapy at the right time is vital. For many cancers, it must begin soon after surgery. Waiting too long can let cancer cells grow, making treatment less effective. We start when the patient is well enough to handle it.
Optimal Duration for Different Adjuvant Modalities
The length of adjuvant therapy varies by treatment and cancer. Chemotherapy can last months to years. Hormone therapy for breast cancer might go on for 5 to 10 years. Adjusting treatment length based on patient risk and response is key to success.
Consequences of Delayed or Interrupted Treatment
Stopping or delaying treatment can harm patient outcomes. It can reduce treatment success, increase recurrence risk, and worsen prognosis. We help patients manage side effects and stick to the plan, aiming to avoid breaks.
In summary, the timing and length of adjuvant therapy are essential for cancer treatment. By focusing on these aspects and customizing plans, we can improve patient outcomes and survival chances.
Key Fact #6: Adjuvant Treatment Reduces Recurrence by Up to 30%
Adjuvant treatment is key in cancer care, cutting recurrence risk in many cancers. This drop in recurrence boosts patient outcomes and survival chances. We’ll look at the stats backing adjuvant therapy’s success, what affects recurrence rates, and how these numbers help patients.
Statistical Evidence Across Cancer Types
Many studies show adjuvant therapy cuts recurrence rates by up to 30% in some cancers. For example, in breast cancer, adjuvant chemo lowers recurrence risk in high-risk cases. In colorectal cancer, adjuvant chemo boosts survival rates. The data shows adjuvant treatment works well across many cancers.
Factors Influencing Recurrence Reduction Rates
The benefit of adjuvant therapy is clear, but how much it helps varies. It depends on the cancer type and stage, the treatment used, the patient’s age and health, and biomarkers. Knowing these factors helps doctors tailor treatments for each patient, aiming for the best recurrence reduction.
Translating Statistics to Individual Patient Outcomes
Turning stats into patient results needs a careful look at each person’s situation. While big data shows adjuvant therapy’s benefits, results can differ for each person. We focus on each patient, using the latest research and their unique needs to guide treatment.
Key Fact #7: Evidence-Based Protocols Drive Success
The success of adjuvant treatment depends on using evidence-based protocols. These protocols come from clinical trials that check how well and safely treatments work.
How Clinical Trials Shape Treatment Guidelines
Clinical trials are key in making treatment guidelines for adjuvant therapy. They test different treatments to see what works best for certain patients.
- Randomized controlled trials give strong evidence on the best adjuvant treatments.
- Phase III trials compare standard treatments with new ones.
- These trials help update guidelines, making sure patients get the best care.
Evidence-based protocols are vital in adjuvant care. They make treatment consistent, which improves results.
Liv Hospital’s Approach to Protocol Implementation
At Liv Hospital, we stick to evidence-based protocols in our adjuvant treatment. Our teams look at the latest trial data to keep our guidelines current and effective.
We take a personalized approach to adjuvant care. We tailor treatment plans to each patient’s needs. This includes the cancer type, stage, and overall health.
Quality Standards in Adjuvant Care Delivery
Keeping adjuvant care high-quality is essential. This means following evidence-based protocols and focusing on patient-centered care with compassion.
Quality adjuvant care includes:
- Starting treatment on time to make it most effective.
- Watching and managing side effects closely.
- Working together with all healthcare providers for a smooth treatment experience.
By focusing on these, we aim to improve outcomes and quality of life for our patients.
Managing Side Effects During Adjuvant Treatment
Managing side effects is key in adjuvant therapy. It helps patients handle treatment well and get the best results. Adjuvant care means more than just treating cancer. It also includes helping patients deal with side effects.
Common Side Effects by Treatment Type
Each adjuvant therapy has its own side effects. For example, chemotherapy can cause tiredness, hair loss, and nausea. Radiation therapy might lead to skin problems and tiredness. Hormone therapy can cause hot flashes, mood swings, and sexual issues. Knowing these side effects is important for managing them well.
Some common side effects include:
- Fatigue: Feeling very tired that affects daily life.
- Nausea and Vomiting: Often seen with chemotherapy, but can be helped with medicine.
- Hair Loss: Caused by chemotherapy, but usually grows back.
- Skin Reactions: Radiation can cause skin irritation, dryness, and peeling.
Supportive Care Strategies for Patients
Supportive care is vital for managing side effects and improving patient outcomes. It includes:
- Symptom Management: Using medicines and other methods to reduce symptoms.
- Nutritional Support: Helping patients eat well to stay strong and healthy.
- Psychological Support: Providing counseling and resources to help with emotional issues.
- Physical Activity: Encouraging patients to stay active to fight fatigue and feel better.
When Side Effects Require Treatment Modification
Severe side effects might mean changing the treatment plan. This could mean reducing doses, delaying treatment, or switching therapies. Our healthcare team watches patients closely and works with them to make the best decisions.
Good side effect management is key to adjuvant therapy success. By knowing the side effects of treatments and using supportive care, we can help patients tolerate therapy better. This leads to better outcomes for them.
Patient Selection: Who Should Receive Adjuvant Therapy?
Choosing who gets adjuvant therapy is complex. We look at many factors to make sure it’s effective.
Risk Assessment Tools and Biomarkers
Assessing risk is key in picking patients for adjuvant therapy. We use tools and biomarkers to see if cancer might come back. This helps us find those at high risk who need extra treatment.
Biomarkers are very important. They tell us about the tumor’s biology. For example, in breast cancer, biomarkers like ER, PR, and HER2 status help decide treatment.
| Biomarker | Cancer Type | Implication for Adjuvant Therapy |
|---|---|---|
| ER/PR Positive | Breast Cancer | Indicates hormone therapy might help |
| HER2 Positive | Breast Cancer | Points to targeted therapies like trastuzumab |
| KRAS Mutation | Colorectal Cancer | May affect choice of chemotherapy or targeted therapy |
Weighing Benefits Against Possible Harms
We must think about the good and bad of adjuvant therapy. We look at how likely cancer will come back without treatment. Then we compare that to how much treatment might reduce that risk.
We also consider side effects and long-term problems. Some treatments can have big side effects, while others might cause damage in one area.
Shared Decision-Making in Treatment Planning
Shared decision-making is important in choosing adjuvant therapy. We talk with patients to understand their needs and values. This way, we make sure treatment fits them well.
This teamwork helps us create plans that meet medical needs and respect the patient’s life and choices. By using risk assessment, weighing benefits and harms, and making decisions together, we make sure adjuvant therapy is used wisely. This helps our patients the most.
Emerging Innovations in Adjuvant Treatment
The field of adjuvant treatment is changing fast with new ideas. Medical research is leading to better ways to help patients and lower cancer risk.
Genomic Testing for Treatment Customization
Genomic testing is changing how we treat cancer. It lets doctors tailor treatments based on a tumor’s genes. This precision medicine makes treatments more effective for each patient.
For example, it helps decide if early-stage breast cancer patients need chemotherapy. This way, treatments are more targeted and side effects are reduced.
Novel Agents and Combination Approaches
New drugs and combinations are big steps forward in adjuvant treatment. Scientists are finding drugs that target cancer cells better and with fewer side effects. They’re also looking at mixing different treatments to improve results.
One promising mix is combining immunotherapy with chemotherapy. Trials are finding the best ways to use these together. This could make treatments more effective.
De-escalation Strategies for Lower-Risk Patients
For patients at lower risk, treatments are getting less intense. This means fewer side effects without losing effectiveness. It’s great for patients with good chances of recovery.
Some research suggests skipping radiation for some early cancers. But it’s important to pick the right patients and watch them closely. This way, treatments are safer and more effective.
These new ideas are set to change cancer care a lot. With genomic testing, new drugs, and less intense treatments, we’re moving towards better, more tailored care for everyone.
Conclusion: The Evolving Landscape of Adjuvant Cancer Care
Adjuvant treatment is key in cancer care, aiming to reduce the chance of cancer coming back. It’s important for improving outcomes in many cancers, like breast, colorectal, and lung cancer. This shows how vital it is for better patient care.
The future of adjuvant care looks bright, thanks to new research and ideas. We’re seeing more use of genetic testing, new drugs, and combining treatments. These changes could make adjuvant therapy even more effective, giving patients better, tailored treatments.
It’s important to know what adjuvant treatment is. It includes chemotherapy, radiation, hormone therapy, and targeted treatments. These aim to get rid of any cancer cells left behind. As we keep learning, sticking to proven methods and high standards in care is more important than ever.
At Liv Hospital, we’re dedicated to top-notch healthcare for international patients. Our approach to adjuvant care is based on the latest research and focuses on the patient. We’re excited to see how new treatments and personalized care will keep improving adjuvant cancer care in the future.
FAQ
What is adjuvant treatment?
Adjuvant treatment is therapy given after primary treatments, like surgery. It aims to get rid of any leftover cancer cells and lower the chance of cancer coming back.
How does adjuvant therapy differ from neoadjuvant therapy?
Adjuvant therapy comes after the main treatment. Neoadjuvant therapy is given before to shrink the tumor.
What is the purpose of adjuvant chemotherapy?
Adjuvant chemotherapy kills tiny cancer cells left after surgery. This helps prevent cancer from coming back.
What are the common types of adjuvant cancer treatments?
Common treatments include chemotherapy, radiation, hormone therapy, targeted therapies, and immunotherapy.
How is the decision made to use adjuvant therapy?
Decisions are based on the cancer type, stage, patient factors, and clinical trial results.
What are the benefits of adjuvant therapy?
It greatly lowers the chance of cancer coming back. This improves patient outcomes and survival rates.
How is the efficacy of adjuvant chemotherapy measured?
Its success is seen in how well it prevents cancer from coming back. This is checked through clinical trials and stats.
What are the common side effects of adjuvant treatment?
Side effects depend on the treatment. They can include fatigue, nausea, hair loss, and a higher risk of infections.
How are side effects managed during adjuvant treatment?
Managing side effects involves supportive care. This includes medication, lifestyle changes, and adjusting treatments when needed.
What is the role of evidence-based protocols in adjuvant therapy?
Evidence-based protocols guide treatments. They use clinical trial results to ensure safe and effective care, making adjuvant therapy successful.
What are the emerging innovations in adjuvant treatment?
New developments include genomic testing for personalized care, new agents, and combining treatments. There’s also a focus on using less treatment for lower-risk patients.
References
Wikipedia: Adjuvant therapy
National Cancer Institute (NCI): Adjuvant Therapy (Cancer Terms)