At Liv Hospital, we are dedicated to top-notch healthcare for all patients. We focus on breast cancer therapeutics with innovative and precise methods. This shows our commitment to fighting the disease effectively.
Targeted therapy attacks specific proteins on breast cancer cells. It helps kill cancer cells or slow them down. This method has changed how we treat breast cancer, bringing hope with tailored treatments.
Key Takeaways
- Targeted therapy is a precise approach to treating breast cancer.
- Liv Hospital is committed to providing world-class healthcare.
- Innovative methods are used to combat breast cancer.
- Targeted therapy uses medicines directed at specific proteins.
- Personalized medication offers new hope for patients.
The Science Behind Targeted Treatment for Breast Cancer
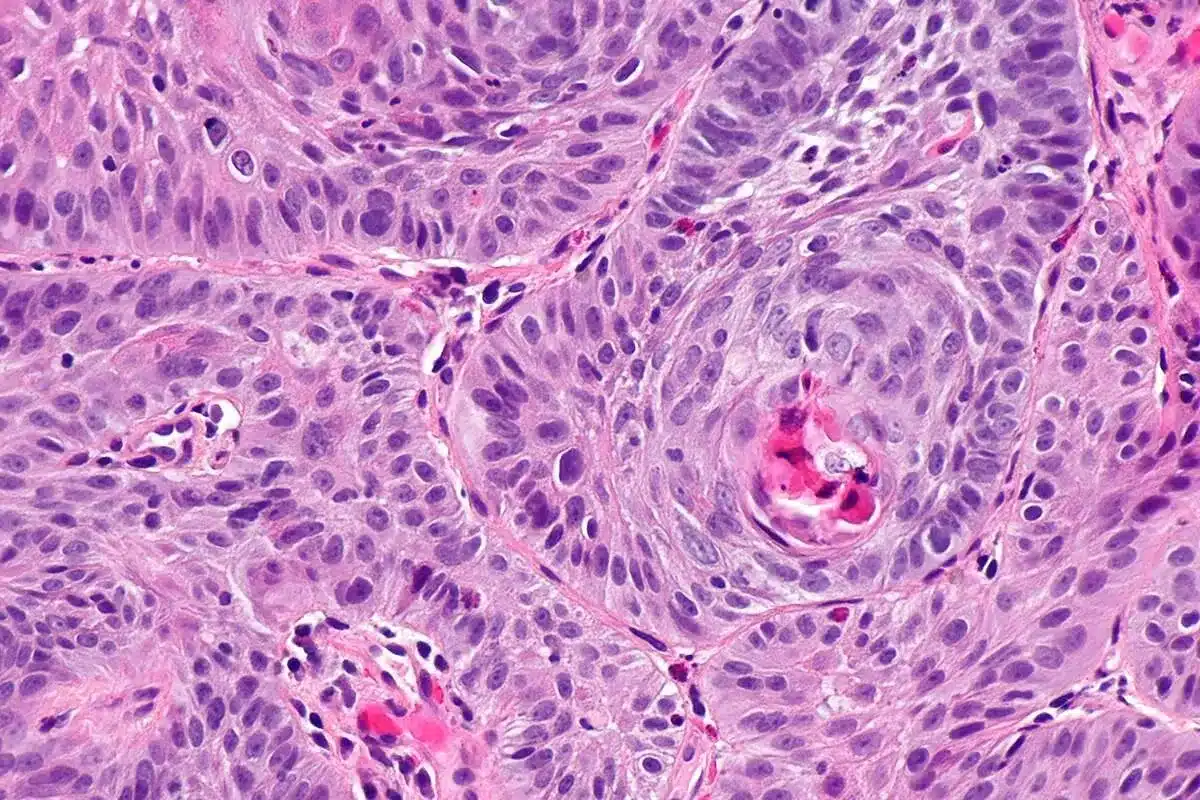
The science behind targeted treatment for breast cancer focuses on how tumors grow. These treatments aim to hit cancer cells hard, while keeping normal cells safe. This is a big step up from old chemotherapy methods.
How Precision Therapies Minimize Harm to Normal Cells
Precision therapies work by targeting specific proteins or genes in cancer cells. For example, monoclonal antibodies can find and mark cancer cells for destruction. This way, they cause less damage to healthy cells, leading to fewer side effects.
Tyrosine kinase inhibitors are another type of targeted therapy. They block enzymes that help cancer cells grow. By stopping these enzymes, the drugs slow down or stop cancer cell growth.
The Shift from Conventional to Targeted Approaches
The move to targeted therapies is a big change in treating breast cancer. Old treatments like chemotherapy and radiation had many side effects. But targeted therapies are more tailored to each patient’s needs.
This personalized approach makes treatments more effective and less harsh. As we learn more about breast cancer, we’ll see even better treatments come along.
The Evolution of Breast Cancer Therapeutics
Over the years, how we treat breast cancer has changed a lot. We now use treatments that are more focused and work better. This change is thanks to a better understanding of breast cancer biology.
The way we treat breast cancer has moved from general treatments to more specific ones. Targeted therapies are now key in fighting breast cancer. They give hope to patients all over the world.
Historical Perspective on Treatment Approaches
Old treatments for breast cancer included surgery, chemotherapy, and radiation. These methods are important but have their limits. This has led us to look for better ways to treat the disease.
In the 1970s and 1980s, hormone therapy was introduced. It was a big step towards treating breast cancer more precisely. Later, in the late 1990s, HER2-targeted therapies were developed. They greatly helped patients with HER2-positive breast cancer.
Recent Advancements Reducing Mortality Rates
In recent years, we’ve seen a lot of new treatments for breast cancer. This has helped lower death rates. New treatments like CDK4/6 inhibitors, PARP inhibitors, and antibody-drug conjugates have been added. They offer more tailored treatment options for patients.
| Therapeutic Approach | Mechanism of Action | Impact on Breast Cancer Treatment |
|---|---|---|
| CDK4/6 Inhibitors | Inhibit cell cycle progression | Improved outcomes in HR-positive, HER2-negative advanced breast cancer |
| PARP Inhibitors | Exploit DNA repair deficiencies in cancer cells | Effective in treating BRCA-mutated breast cancers |
| Antibody-Drug Conjugates | Deliver cytotoxic agents directly to cancer cells | Enhanced efficacy with reduced side effects in specific breast cancer subtypes |
These new treatments show how far we’ve come in fighting breast cancer. We’re moving towards treatments that are more precise and effective. As we keep researching, we expect to see even better results for patients.
Monoclonal Antibodies: The Cornerstone of HER2-Positive Treatment
Monoclonal antibodies have changed how we treat HER2-positive breast cancer. These targeted treatments have greatly improved results for patients. They focus on cancer cells that have too much of the HER2 protein.
These antibodies stick to specific proteins on cancer cells, stopping them from growing. For HER2-positive breast cancer, they target the HER2 protein. This protein is found in high amounts on cancer cells.
Trastuzumab (Herceptin): Mechanism and Clinical Applications
Trastuzumab was the first monoclonal antibody for HER2-positive breast cancer. It binds to the HER2 protein, stopping cells with too much HER2 from growing. Studies have shown it greatly improves survival and time without disease in patients.
Trastuzumab has changed how we treat HER2-positive breast cancer. It’s often used with chemotherapy to work better. It’s used in:
- Adjuvant treatment for early HER2-positive breast cancer
- Neoadjuvant treatment for locally advanced HER2-positive breast cancer
- Treatment of metastatic HER2-positive breast cancer
Pertuzumab (Perjeta): Enhancing HER2-Targeted Therapy
Pertuzumab targets the HER2 protein but in a different way than trastuzumab. It blocks HER2 signaling, helping to slow tumor growth.
Using pertuzumab with trastuzumab has shown great results in treating HER2-positive breast cancer. This combination has improved survival and time without disease in both metastatic and early stages.
Pertuzumab’s benefits include:
- Stronger blockage of HER2 signaling pathways
- Better results when used with trastuzumab and chemotherapy
- Potential for more complete responses in early treatment
Monoclonal antibodies like trastuzumab and pertuzumab have greatly improved HER2-positive breast cancer treatment. They target the HER2 protein, leading to better outcomes and becoming key parts of treatment plans.
CDK4/6 Inhibitors: Controlling Cancer Cell Proliferation
CDK4/6 inhibitors are a new type of targeted therapy. They have shown great promise in fighting cancer. These drugs are key in treating hormone receptor-positive breast cancer, helping manage the disease well.
There have been big steps forward in CDK4/6 inhibitors. Three drugs stand out: palbociclib, ribociclib, and abemaciclib. They all work by stopping cyclin-dependent kinases 4 and 6. These are important for cells to grow and divide.
Palbociclib (Ibrance): First-in-Class CDK4/6 Inhibitor
Palbociclib was the first CDK4/6 inhibitor approved by the FDA. It’s a big win for treating hormone receptor-positive breast cancer. Studies showed it improved how long patients lived without their cancer getting worse when used with hormone therapy.
Palbociclib works by blocking CDK4 and CDK6. This stops the cell cycle from moving forward at the G1 phase. This leads to fewer cancer cells growing.
“The introduction of palbociclib has changed the landscape of breast cancer treatment, providing a new option for patients with hormone receptor-positive disease.”
Ribociclib (Kisqali) and Abemaciclib (Verzenio): Comparative Analysis
Ribociclib and abemaciclib are also effective against hormone receptor-positive breast cancer. They work like palbociclib but have different effects on the body and how they’re used.
| Drug | Dosing Schedule | Notable Side Effects |
|---|---|---|
| Palbociclib (Ibrance) | 21 days on, 7 days off | Neutropenia, fatigue |
| Ribociclib (Kisqali) | 21 days on, 7 days off | Neutropenia, QT prolongation |
| Abemaciclib (Verzenio) | Continuous dosing | Diarrhea, neutropenia |
Choosing between these drugs depends on the patient’s situation. Research is ongoing to better understand their roles in treatment.
Antibody-Drug Conjugates: Precision Delivery Systems
Antibody-drug conjugates are a big step forward in treating breast cancer. They deliver chemotherapy right to the cancer cells.
These new treatments use monoclonal antibodies and powerful drugs. They aim to harm cancer cells more and protect normal cells.
Trastuzumab Emtansine Structure and Function
Trastuzumab emtansine, or Kadcyla, is made for HER2-positive breast cancer. It’s a mix of trastuzumab and DM1, a drug that kills cells.
It works by targeting HER2-positive cancer cells. There, DM1 stops microtubules from working, killing the cells.
Key Benefits:
- Targeted delivery of chemotherapy
- Reduced harm to normal cells
- Effective against HER2-positive breast cancer
Sacituzumab Govitecan: Expanding Treatment Options
Sacituzumab govitecan, or Trodelvy, is a new hope for triple-negative breast cancer.
It’s made from an anti-Trop-2 antibody and SN-38, irinotecan’s active part. When it finds Trop-2-positive cells, it releases SN-38, killing them.
| Characteristics | Trastuzumab Emtansine | Sacituzumab Govitecan |
|---|---|---|
| Target | HER2 | Trop-2 |
| Cytotoxic Agent | DM1 | SN-38 |
| Indication | HER2-positive breast cancer | Triple-negative breast cancer |
Trastuzumab emtansine and sacituzumab govitecan are big steps in fighting breast cancer. They give patients better, more targeted treatments.
PARP Inhibitors: Exploiting DNA Repair Deficiencies
For those with BRCA-mutated breast cancers, PARP inhibitors are a new hope. These drugs target the DNA repair flaws in cancer cells with BRCA mutations. This makes treatment more precise.
PARP inhibitors are key in treating BRCA1 and BRCA2 mutations. They block the PARP enzyme. This stops cancer cells from fixing DNA damage, causing them to die.
Olaparib for BRCA-Mutated Breast Cancers
Olaparib (Lynparza) is a leading PARP inhibitor for BRCA-mutated breast cancers. Studies show it boosts survival in advanced cases.
Olaparib is a game-changer for those with germline BRCA mutations. It targets the genetic root of their cancer, providing a tailored treatment.
Talazoparib: Potent PARP Inhibition
Talazoparib (Talzenna) is another strong PARP inhibitor for BRCA-mutated breast cancers. Like olaparib, it blocks DNA repair but is more potent in tests.
Talazoparib works for both germline and somatic BRCA mutations. This means more people can benefit from this therapy. It’s a promising addition to cancer treatment.
Olaparib and talazoparib are big steps forward in treating BRCA-mutated breast cancers. They offer targeted, effective treatments that improve patient outcomes.
PI3K Inhibitors: Targeting a Critical Signaling Pathway
The discovery of PI3K inhibitors has changed how we treat breast cancer. This is true for cases where the PIK3CA gene is mutated. These inhibitors block a key pathway that cancer cells use to grow and survive.
Alpelisib for PIK3CA-Mutated Breast Cancer
Alpelisib, also known as Piqray, is a PI3K inhibitor that works well for PIK3CA-mutated breast cancer. It targets the alpha isoform of PI3K, which is often mutated in breast cancer. Studies show that alpelisib, when paired with endocrine therapy, boosts survival time for patients with hormone receptor-positive, HER2-negative advanced breast cancer with PIK3CA mutations.
The approval of alpelisib is a big step forward in treating breast cancer. It offers a targeted treatment for patients with specific genetic changes. By blocking the PI3K pathway, alpelisib tackles a major driver of tumor growth in PIK3CA-mutated cancers.
Combination Approaches with Endocrine Therapy
Using PI3K inhibitors like alpelisib with endocrine therapy is a promising strategy. Endocrine therapy targets hormone receptor-positive breast cancer cells. PI3K inhibitors block a key pathway that can make these cells resistant to endocrine therapy. This combination can help overcome resistance and improve patient outcomes.
Studies have shown that alpelisib with endocrine therapy, like letrozole or fulvestrant, can slow disease progression more than endocrine therapy alone. This combo is most beneficial for patients with PIK3CA-mutated, hormone receptor-positive breast cancer.
As research keeps advancing, combining PI3K inhibitors with other targeted therapies is being looked into. This could lead to even better treatment results and care for patients.
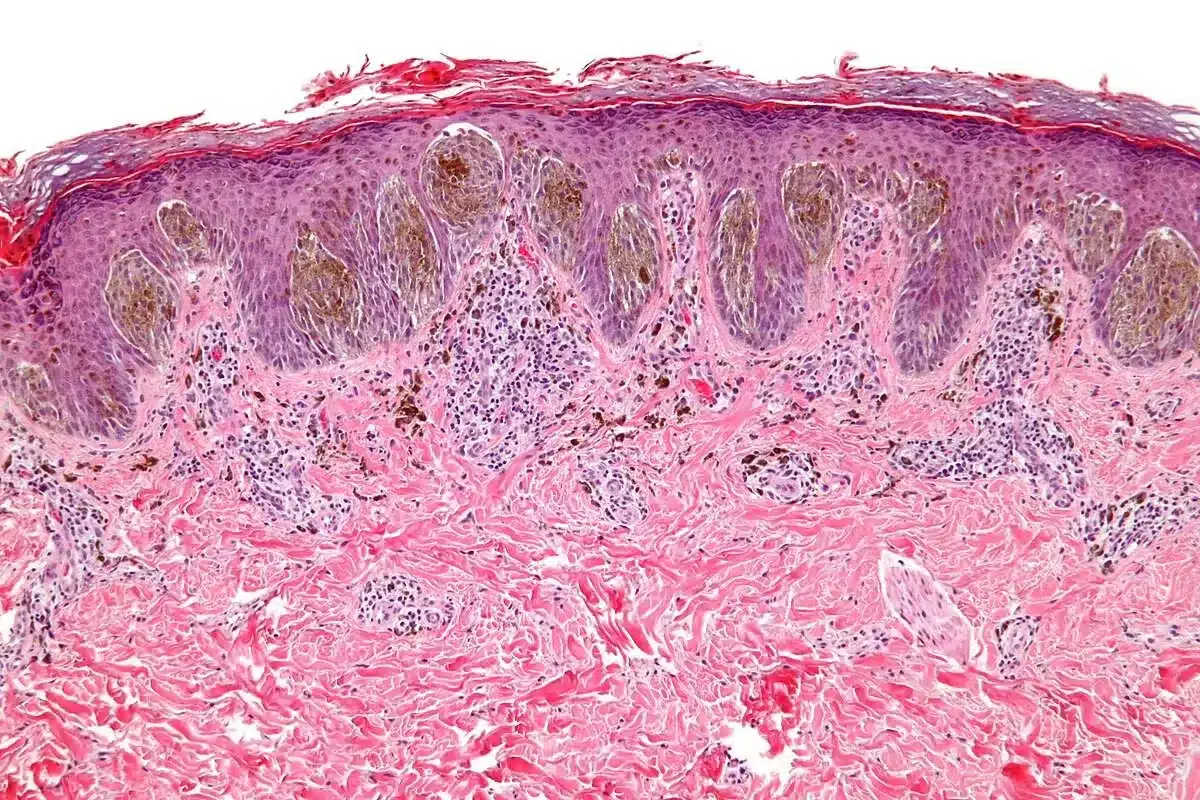
Personalized Medicine Approaches in Breast Cancer Treatment
Genetic testing and biomarker analysis are changing how we treat breast cancer. At Liv Hospital, we focus on creating treatment plans that meet each patient’s unique needs.
Genetic Testing and Biomarker Analysis
Genetic testing and biomarker analysis are key in finding the best treatments for breast cancer patients. They help us understand the cancer’s aggressiveness and how it will react to different therapies.
Some key benefits of these tests include:
- Identifying patients with BRCA1 and BRCA2 mutations, who may benefit from targeted therapies such as PARP inhibitors.
- Detecting HER2-positive breast cancers, which can be treated with HER2-targeted therapies.
- Analyzing PIK3CA mutations, which can inform the use of PI3K inhibitors.
Treatment Decision Frameworks for Clinicians
Clinicians use treatment decision frameworks to plan personalized care for breast cancer patients. These frameworks consider many factors, including:
- Genetic and biomarker profiles
- Tumor characteristics, such as size, grade, and receptor status
- Patient preferences and overall health
By combining these factors, clinicians can create effective, personalized treatment plans. This approach improves patient outcomes.
At Liv Hospital, we are committed to leading in personalized medicine for breast cancer treatment. Our team works together to ensure each patient gets the best care.
Liv Hospital’s Innovative Protocols for Targeted Therapy
Liv Hospital is changing how we treat breast cancer. We keep our treatment plans up to date with the latest research. This ensures our patients get the best care possible.
Evidence-Based Treatment Guidelines
At Liv Hospital, we use evidence-based treatment guidelines for each patient. Our team looks at new studies and clinical trials to guide our care. For example, we’ve added a new targeted therapy based on a study in a top medical journal (source).
- We update our treatment plans with the latest research.
- We create personalized plans based on each patient’s needs and genetic profile.
- Our team works together to ensure complete care.
Multidisciplinary Approach to Personalized Care
Our multidisciplinary approach brings together experts like oncologists and surgeons. This team works together to create care plans that fit each patient’s needs.
Our approach includes:
- Our team discusses each case to find the best treatment.
- We use a mix of treatments, like surgery and targeted therapy.
- We educate and support our patients every step of the way.
By using innovative protocols and a team effort, Liv Hospital offers top-notch care. Our patients get the best results because of it.
Emerging Targeted Therapies in Clinical Development
The world of breast cancer treatment is changing fast. New targeted therapies are being developed. These treatments aim at specific parts of cancer cells, making care more effective and tailored.
Novel Drug Classes on the Horizon
New drug classes are being tested in clinical trials. Antibody-drug conjugates (ADCs) aim to hit cancer cells hard but spare healthy ones. PI3K inhibitors target a key pathway that helps cancer grow and survive.
Researchers are also looking into cyclin-dependent kinase inhibitors and PARP inhibitors. These new agents might work alone or with other treatments to boost their power.
Promising Combination Strategies
Combining treatments is seen as a key way to beat breast cancer. By mixing targeted therapies with chemotherapy, hormone therapy, or immunotherapy, doctors hope to get better results. This approach aims to overcome cancer’s defenses and lead to lasting benefits.
For example, adding CDK4/6 inhibitors to hormone therapy has helped hormone receptor-positive breast cancer patients a lot. Also, pairing PI3K inhibitors with other treatments or chemotherapy is being studied to tackle cancer’s complex signals.
As these new therapies and combinations move forward, they could make breast cancer treatment even better. This brings new hope for both patients and doctors.
Conclusion: The Future of Precision Oncology in Breast Cancer
The way we treat breast cancer is changing with precision oncology. Targeted therapies are making treatments more effective. At Liv Hospital, we’re always looking for the latest and best treatments for our patients.
Research is key to making targeted therapy even better. We’re looking into new drugs and ways to mix them. This will help us tailor treatments to each patient’s needs.
Genetic testing and personalized medicine are becoming more important. They help us make treatments that work best for each person. This is how we’re improving care for breast cancer patients.
By using precision oncology, we’re making treatments more effective. This also means our patients can live better lives. The future of treating breast cancer looks very promising.
What is targeted therapy for breast cancer?
Targeted therapy for breast cancer uses drugs that target cancer cells. This helps avoid harming normal cells. It has changed how we treat breast cancer, giving patients new hope.
How do monoclonal antibodies work in treating HER2-positive breast cancer?
Monoclonal antibodies, like trastuzumab and pertuzumab, target the HER2 protein on cancer cells. They help slow or stop cancer growth. This has greatly improved survival and quality of life for those with HER2-positive breast cancer.
What are CDK4/6 inhibitors, and how are they used in breast cancer treatment?
CDK4/6 inhibitors, including palbociclib, ribociclib, and abemaciclib, control cancer cell growth. They treat hormone receptor-positive breast cancer. These drugs are key in managing the disease.
What are antibody-drug conjugates, and how do they work?
Antibody-drug conjugates, such as trastuzumab emtansine and sacituzumab govitecan, combine antibodies with chemotherapy. They deliver the drug directly to cancer cells, making treatment more precise.
How do PARP inhibitors work in treating BRCA-mutated breast cancers?
PARP inhibitors, like olaparib and talazoparib, target DNA repair issues in BRCA-mutated cancers. They help stop cancer cell growth. These treatments have shown great promise in trials.
What is the role of PI3K inhibitors in breast cancer treatment?
PI3K inhibitors, such as alpelisib, target a key signaling pathway in breast cancer. They offer new options for patients with PIK3CA mutations. Combining them with endocrine therapy has shown promising results.
How is personalized medicine approached in breast cancer treatment?
Personalized medicine in breast cancer treatment uses genetic testing and biomarker analysis. It tailors treatment to each patient. Clinicians use frameworks to ensure care is effective and personalized.
What are the benefits of targeted therapy for breast cancer treatment?
Targeted therapy improves treatment outcomes and reduces side effects. It enhances quality of life. At Liv Hospital, we provide world-class healthcare and support for international patients, using the latest targeted therapy advancements.
What are some of the emerging targeted therapies in clinical development for breast cancer?
New targeted therapies and combination strategies are emerging. They offer hope for more effective care. Ongoing research and development are leading to innovative treatments that will improve outcomes.
How does Liv Hospital approach targeted therapy for breast cancer?
At Liv Hospital, we follow evidence-based guidelines and take a multidisciplinary approach. We ensure patients get tailored and complete treatment. Our team works together to achieve the best outcomes for our patients.
References
- Breastcancer.org. (2025, June 10). Targeted Therapy Medicines: What They Are and How They Work. Retrieved from https://www.breastcancer.org/treatment/targeted-therapy BreastCancer.org
- National Breast Cancer Foundation. (2025, April 17). Targeted Therapy. Retrieved from https://www.nationalbreastcancer.org/breast-cancer-targeted-therapy/ National Breast Cancer Foundation
- Breast Cancer Research Foundation. (n.d.). Targeted Therapy for Breast Cancer. Retrieved from https://www.bcrf.org/about-breast-cancer/targeted-therapy-breast-cancer/
- Masoud, V., et al. (2017). Targeted therapies in breast cancer: New challenges to treatment resistance. [Review]. PMC. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5385433/ pmc.ncbi.nlm.nih.gov
- Cancer Research UK. (n.d.). Targeted & immunotherapy drugs for breast cancer. Retrieved from https://www.cancerresearchuk.org/about-cancer/breast-cancer/treatment/targeted-immunotherapy-drugs