Last Updated on November 26, 2025 by Bilal Hasdemir
Did you know that over 1.8 million people worldwide get cancer each year? Many of them go through chemotherapy as part of their treatment. This treatment can greatly affect the body, not just the cancer cells.Explore how affects chemotherapy before and after results
Exploring what happens to someone on chemotherapy is key. We need to understand the chemotherapy recovery process and the changes that happen before and after. We’ll look at how chemotherapy impacts the body and what patients can expect on this journey.
Key Takeaways
- Chemotherapy affects not just cancer cells but the overall well-being of the individual.
- Understanding the chemotherapy recovery process is key for patients.
- The effects of chemotherapy on the body can be significant.
- Changes occur before, during, and after chemotherapy treatment.
- Patients can prepare for the journey by knowing what to expect.
Understanding Chemotherapy: A Complete Overview
Chemotherapy is a treatment that uses drugs to kill cancer cells all over the body. It’s a key part of fighting cancer, helping when it has spread or is likely to spread. Knowing how chemotherapy works helps patients understand their treatment better.
What Is Chemotherapy and How Does It Work?
Chemotherapy uses drugs to target and kill cancer cells. These drugs stop cancer cells from dividing and growing, causing them to die. Chemotherapy can be given in different ways, like taking pills or getting shots, based on the cancer type and drugs used.
The success of chemotherapy depends on many things. These include the cancer type, its stage, and the patient’s health. Knowing the chemotherapy treatment timeline helps manage expectations and prepare for treatment.
Types of Chemotherapy Drugs and Their Mechanisms
There are many types of chemotherapy drugs, each working in its own way. These include:
- Alkylating agents, which damage DNA in cancer cells to stop them from reproducing.
- Antimetabolites, which block DNA and RNA production, stop cancer cell growth.
- Anthracyclines, which insert into DNA strands, stop DNA and RNA synthesis.
Knowing how these drugs work helps patients understand their treatment and why certain drugs are chosen.
Goals of Chemotherapy Treatment
The main goals of chemotherapy can change based on the treatment situation. These goals include:
- Curative intent: To cure the cancer by getting rid of all cancer cells.
- Control: To stop the cancer from growing or spreading.
- Palliative care: To ease symptoms and improve life quality when a cure is not possible.
Checking chemotherapy effectiveness means watching how the cancer responds to treatment. This includes looking at tumor size, cancer markers, and overall health. Managing chemotherapy side effects is also key, as it affects the patient’s quality of life.
Chemotherapy Before and After: Physical Changes to Anticipate
Chemotherapy brings about noticeable physical changes. Knowing these can help patients prepare and make better care choices.
Immediate Physical Changes During Early Treatment
Right when chemotherapy starts, patients notice changes. These can be fatigue, hair loss, and changes in appetite or skin.
“The first few sessions were the toughest,” he said. “I felt like I was running on empty all the time.”
These early changes are tough but part of treatment. We’ll help manage these side effects to improve life quality.
Long-Term Physical Changes Throughout Treatment
As treatment goes on, patients face more changes. These include ongoing hair loss, weight changes, and nail issues. Some might also feel neuropathy or other sensory problems.
Knowing these changes helps patients plan. Some might use wigs or change their diet and exercise to handle weight changes.
Recovery of Physical Appearance After Treatment
After treatment ends, many see their looks improve. Hair starts growing back in a few months, though it might be thinner or different. Nail health also gets better over time.
But recovery times vary. Some quickly get back to how they looked before, while others take longer. We’ll support patients, helping with any lasting side effects and improving their overall health.
The Chemotherapy Treatment Timeline

Knowing the timeline of chemotherapy is key for patients. It helps them get ready for what’s coming. Chemotherapy uses drugs to kill cancer cells or stop them from growing.
Understanding Treatment Cycles and Schedules
Treatment cycles let the body recover from chemotherapy. The schedule of sessions is planned to be effective yet gentle on the patient.
What Is a 21-Day Chemo Cycle?
A 21-day chemo cycle is common. It starts with chemotherapy on day one. Then, there are 20 days of rest before the next cycle. This cycle can be repeated many times.
Duration Variations Based on Cancer Type and Stage
Chemotherapy lasts differently for each cancer type and stage. Early-stage cancers might need fewer cycles than advanced ones.
How Long Does the Entire Chemotherapy Process Take?
The whole chemotherapy process can take months. It depends on the treatment plan and how well the patient responds.
| Cancer Type | Typical Number of Cycles | Duration per Cycle | Total Treatment Duration |
| Breast Cancer | 4-6 cycles | 21 days | 4-6 months |
| Colorectal Cancer | 6-12 cycles | 14 or 21 days | 3-6 months |
| Lymphoma | 3-8 cycles | 21 or 28 days | 3-8 months |
Knowing the chemotherapy timeline helps patients prepare. The treatment’s length and schedule are made just for them. They consider the cancer type, stage, and the patient’s health.
A Typical Chemotherapy Session Explained
Knowing what to expect during chemotherapy can help reduce anxiety. Chemotherapy uses drugs to kill cancer cells. We’ll look at how long a session lasts, who can visit, and how the drugs are given.
How Long Is a Chemo Session?
The time for a chemotherapy session varies. It depends on the cancer type, drugs used, and the patient’s plan. Sessions can last from a few minutes to hours.
Factors Influencing Session Length:
- Type of chemotherapy drugs
- Method of administration (e.g., intravenous, oral)
- Patient’s overall health and response to treatment
| Chemotherapy Drug Type | Typical Administration Time |
| Bolus Injection | A few minutes to 15 minutes |
| Short Infusion | 30 minutes to 1 hour |
| Continuous Infusion | Several hours to days |
What Happens During Administration
Healthcare professionals manage the chemotherapy process. It includes:
- Preparation: Checking the patient’s identity and medical history, and preparing the drugs.
- Administration: Giving the drugs through the chosen method (e.g., IV, orally).
- Monitoring: Watching for any bad reactions or side effects during and after.
Can You Have Visitors During Chemotherapy?
Visitor policies vary by treatment setting and patient condition. Having a support person can offer comfort. But it’s important to follow the facility’s visitor rules.
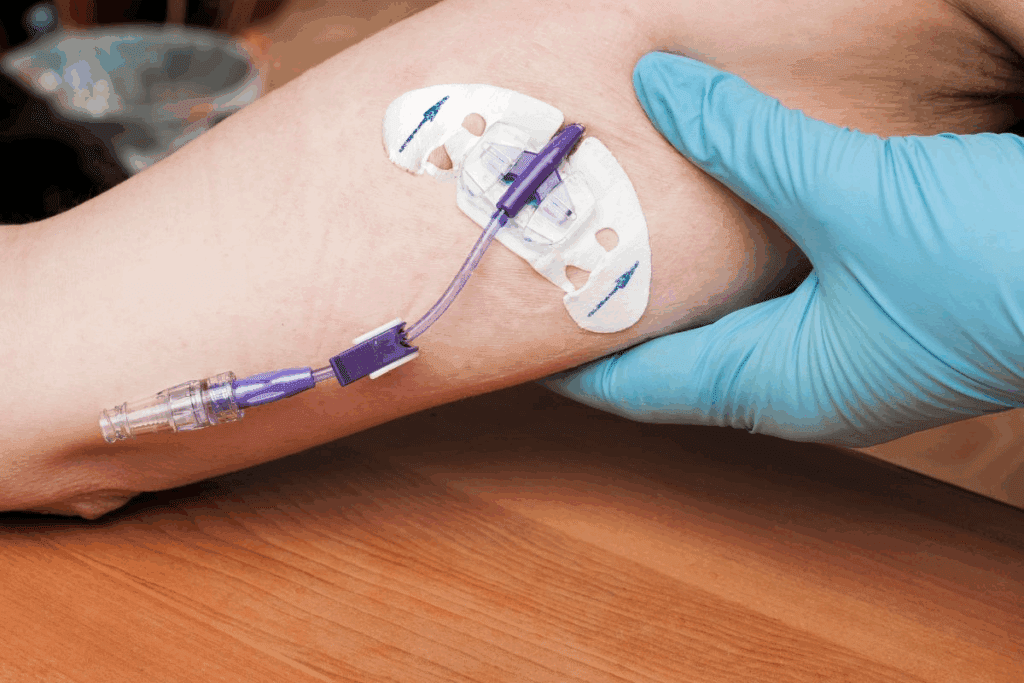
Different Methods of Chemotherapy Delivery
Chemotherapy can be given in several ways, each with its own benefits and challenges:
- Oral Chemotherapy: Taken in pill or liquid form, easy but requires strict following of the regimen.
- Intravenous (IV) Chemotherapy: Given directly into a vein, it allows for higher doses and quicker effect.
- Intraperitoneal Chemotherapy: Delivered directly into the abdominal cavity, used for certain cancers.
Knowing these methods helps patients prepare and make informed decisions about their care.
What Chemotherapy Does to Your Body
Chemotherapy affects the body in many ways, touching different cells and systems. It’s made to kill fast-growing cancer cells. But it also hits other cells and systems in the body.
Immediate Effects on Cells and Systems
Chemotherapy targets cells that grow fast. This means it hits not just cancer cells but also some healthy ones. The immediate effects can include damage to the bone marrow, hair follicles, and the lining of the digestive system. These cells grow quickly.
How Chemotherapy Distinguishes Between Healthy and Cancer Cells
Chemotherapy aims to kill cancer cells, but it doesn’t always get it right. The treatment affects any rapidly dividing cells, whether they are cancerous or healthy. The problem is, some healthy cells grow fast too, making them vulnerable to chemotherapy’s effects.
Cumulative Effects of Multiple Treatments
Getting multiple rounds of chemotherapy can really take a toll. With each cycle, the body’s ability to recover is tested. Over time, the effects on the body’s systems can grow, leading to more side effects and health strain.
Impact on Immune System Function
Chemotherapy’s effect on the immune system is a big deal. The treatment can weaken the immune system by affecting the bone marrow’s ability to produce white blood cells. These cells are key in fighting off infections. This makes patients more likely to get sick during and after treatment.
Common Side Effects and Their Timeline
Chemotherapy is a strong tool against cancer, but it has many side effects. These side effects vary in timing and how long they last. Knowing when these side effects happen can help patients through their treatment.
Immediate Side Effects (Hours to Days)
Some side effects show up right after treatment starts. These can include:
- Fatigue
- Nausea and vomiting
- Hair loss
- Mouth sores
These quick effects happen because chemotherapy drugs target fast-growing cells. This includes both cancer cells and some healthy cells.
Short-Term Side Effects (Days to Weeks)
As treatment goes on, patients may face side effects that last from days to weeks. These can be:
- Increased risk of infection
- Anemia
- Bleeding or bruising easily
- Changes in appetite
It’s key to manage these side effects to keep the patient’s quality of life up during treatment.
Long-Term Side Effects (Months to Years)
Some side effects can stick around or show up months to years after treatment ends. These long-term effects can include:
- Heart problems
- Nerve damage (neuropathy)
- Secondary cancers
- Cognitive changes (“chemo brain”)
It’s important to watch and manage these long-term side effects after treatment.
Chemo Every 3 Weeks: Side Effects Pattern
For those getting chemotherapy every 3 weeks, the side effects pattern is clear. The cycle of treatment and recovery can make patients feel better and worse in a pattern. Knowing this pattern helps in planning and managing side effects.
| Timeframe | Common Side Effects |
| Hours to Days | Fatigue, Nausea, Hair Loss |
| Days to Weeks | Infection Risk, Anemia, Bleeding |
| Months to Years | Heart Problems, Neuropathy, Secondary Cancers |
Understanding the timeline of chemotherapy side effects helps patients prepare and manage their treatment. It’s vital to work closely with healthcare providers to lessen these effects and make treatment better.
Managing Chemotherapy Side Effects
Managing side effects from chemotherapy is key to a patient’s quality of life. Chemotherapy affects not just cancer cells but also healthy ones. This leads to various side effects.
Medical Interventions for Side Effect Management
Medical treatments are vital in managing chemotherapy side effects. These can range from medications for nausea and pain to treatments for low blood counts.
Some common medical interventions include:
- Anti-nausea medications to control chemotherapy-induced nausea and vomiting
- Pain management strategies, including medications and alternative therapies
- Blood cell growth factors to prevent or treat low blood counts
- Antibiotics or antivirals to prevent or treat infections
| Medical Intervention | Purpose | Examples |
| Anti-nausea medications | Control nausea and vomiting | Ondansetron, Metoclopramide |
| Pain management | Manage pain | Opioids, NSAIDs, nerve blocks |
| Blood cell growth factors | Prevent or treat low blood counts | Filgrastim, Pegfilgrastim |
Lifestyle Adjustments That Help Minimize Discomfort
Lifestyle changes are key in reducing discomfort from chemotherapy side effects. These changes help patients manage symptoms better and improve their quality of life.
Some beneficial lifestyle adjustments include:
- Dietary changes to manage nausea and maintain nutrition
- Regular, gentle exercise to maintain strength and reduce fatigue
- Stress management techniques, such as meditation or yoga
- Adequate rest and sleep help the body recover
Complementary Therapies That May Provide Relief
Complementary therapies can offer extra relief from chemotherapy side effects. These therapies are used alongside conventional treatments and can improve patient outcomes.
Some complementary therapies that may be beneficial include:
- Acupuncture to manage pain and nausea
- Massage therapy to reduce stress and improve well-being
- Aromatherapy to alleviate nausea and promote relaxation
- Mind-body therapies, such as meditation and guided imagery
By combining medical interventions, lifestyle adjustments, and complementary therapies, patients can better manage chemotherapy side effects. This improves their quality of life during treatment.
Nutrition and Physical Activity During Chemotherapy
Nutrition and exercise are key during chemotherapy. A balanced diet and regular exercise can help manage side effects. They also help keep strength up and improve life quality.
Dietary Recommendations During Treatment
It’s important to eat a diet full of nutrients during chemotherapy. Focus on:
- Lean proteins like chicken, fish, and legumes support muscle mass.
- Complex carbohydrates, such as whole grains, fruits, and vegetables, are used for energy.
- Healthy fats found in nuts, seeds, and avocados for overall health.
Avoid foods that can cause discomfort or interact with your treatment.
Safe Exercise Guidelines for Chemotherapy Patients
Exercise during chemotherapy can reduce fatigue and improve mood. We suggest consulting with your healthcare team before starting any new exercise program.
- Choosing low-impact activities like walking, yoga, or swimming.
- Listening to your body and adjusting the intensity and duration based on how you’re feeling.
Managing Appetite Changes and Nausea
Chemotherapy can affect your appetite and cause nausea. To manage these side effects, we suggest:
- Eating smaller, more frequent meals to ease digestion.
- Avoiding strong-smelling foods that can trigger nausea.
- Staying hydrated by sipping on clear fluids throughout the day.
Staying Hydrated During Treatment
Hydration is key during chemotherapy. Drink plenty of fluids like water, clear broths, or electrolyte-rich beverages. Check your urine output and color to make sure you’re hydrated.
| Hydration Tips | Benefits |
| Drink at least 8-10 glasses of fluid per day | Helps flush out toxins |
| Include electrolyte-rich beverages | Replenishes lost salts |
| Monitor urine color | Ensures proper hydration level |
Emotional and Psychological Effects of Chemotherapy
Patients going through chemotherapy face many emotional and psychological challenges. The mental health impact can be as big as the physical one.
Common Emotional Responses Throughout Treatment
Chemotherapy can make people feel anxious, scared, sad, and frustrated. These feelings can change a lot during treatment.
Some common feelings include:
- Anxiety about the future and treatment outcomes
- Fear of the unknown or fear of side effects
- Sadness and depression due to the loss of normalcy and changes in body image
- Frustration with the limitations imposed by treatment
Strategies for Maintaining Mental Wellbeing
Keeping your mind healthy during chemotherapy is key. Ways to do this include:
- Staying connected with friends and family
- Engaging in activities that bring joy and relaxation
- Practicing mindfulness or meditation
- Seeking support from mental health professionals
Using these strategies can help patients deal with chemotherapy’s emotional challenges.
When to Seek Professional Mental Health Support
Knowing when to get help for emotional issues during chemotherapy is important. Signs you might need help include:
- Persistent feelings of sadness or hopelessness
- Anxiety that interferes with daily life
- Difficulty managing emotions or coping with treatment
Getting help from mental health experts can give patients the tools they need to face these challenges.
“Chemo Brain”: Cognitive Changes During Treatment
“Chemo brain” is when some patients experience cognitive changes during and after chemotherapy. These changes can include:
| Cognitive Change | Description |
| Memory Problems | Difficulty remembering details or events |
| Concentration Issues | Trouble focusing on tasks or conversations |
| Processing Speed | Slower processing of information |
Knowing that “chemo brain” is a common side effect can help patients and their families understand these changes.
Signs That Chemotherapy Is Working
Figuring out if chemotherapy is working can be tricky. It involves looking at different signs and tests. Doctors watch how well the treatment is working by checking several things.
Clinical Indicators of Treatment Effectiveness
There are key signs to see if chemotherapy is effective. These include:
- Reduction in tumor size: If the tumor gets smaller, it’s a good sign.
- Improvement in symptoms: Feeling less pain, tiredness, or breathing problems is a positive sign.
- Normalization of tumor markers: When tumor markers in the blood go down, it means treatment is working.
Diagnostic Tests Used to Monitor Progress
There are many tests to check how chemotherapy is doing. These include:
| Test Type | Description | Purpose |
| CT Scans | Imaging tests that provide detailed pictures of the body’s internal structures. | To assess changes in tumor size and detect any new tumors. |
| Biopsy | A procedure that involves removing a sample of tissue for examination. | To check for cancer cells and assess the effectiveness of treatment. |
| Blood Tests | Tests that measure various substances in the blood, including tumor markers. | To monitor changes in tumor markers and overall health. |
Understanding Partial vs. Complete Response
Chemotherapy can lead to a partial or complete response. A partial response means the tumor is smaller but not gone. A complete response means the tumor is gone. Knowing the difference is important for treatment planning.
What to Expect After 2nd Chemo Treatment
After the second treatment, doctors will check how you’re doing. They might talk about side effects, look at test results, and change the treatment plan if needed.
Chemotherapy can be tough, but we’re here to help. Our team offers full care and support during treatment.
What to Expect After Your Last Chemotherapy Treatment
Finishing chemotherapy is a big deal, but it’s just the start. Knowing what to expect in the recovery phase is key. You’ll go through physical, emotional, and mental changes as you move from treatment to recovery.
Immediate Post-Treatment Period (First Month)
The first month after your last treatment is very important. Your body starts to heal from chemotherapy’s effects. But you might face some side effects. Here are common ones:
- Fatigue: Feeling very tired or weak
- Nausea and vomiting: These might be less severe than during treatment
- Hair loss: You might lose more hair or see changes in texture
- Emotional changes: Mood swings, anxiety, or depression
It’s vital to follow your doctor’s advice for care after treatment. This includes any follow-up visits and medication.
Medium-Term Recovery (1-6 Months)
In the next few months, you’ll likely see health improvements. But some side effects might stick around, or new ones could show up. Key things to focus on include:
- Physical recovery: Slowly getting back to normal activities and strength
- Emotional well-being: Keeping stress and emotional changes in check
- Nutritional balance: Eating well to help your recovery
Long-Term Recovery (6+ Months)
After six months, most people see big health improvements. But some might face lingering side effects or new challenges. Important things to keep in mind include:
- Follow-up care: Keeping up with scheduled appointments and screenings
- Reintegration: Getting back to work, social life, and normal activities
- Ongoing health monitoring: Being aware of late effects from chemotherapy
Post-Treatment Care Plan
A good care plan is essential for recovery. It should include:
- A detailed schedule of follow-up appointments and tests
- Guidance on managing late effects of chemotherapy
- Advice on staying healthy, like diet and exercise
- Support for emotional and psychological well-being
By knowing what to expect after treatment and following a detailed care plan, you can better handle the recovery process.
Chemotherapy Follow-Up Care and Monitoring
After chemotherapy, the next step is monitoring and follow-up care. This is key to check if the treatment worked and to handle any new issues.
Typical Follow-Up Schedule After Completing Treatment
The follow-up schedule changes based on the cancer type, stage, and treatments. At first, patients see their doctor every few months. This frequency may slow down over time.
During these visits, the healthcare team checks overall health. They look for signs of cancer coming back and deal with any side effects or worries.
Ongoing Tests and Screenings
Follow-up care includes regular tests and screenings. These might include:
- Blood tests to check for tumor markers or other health indicators
- Imaging tests like CT scans, MRI scans, or PET scans to watch for cancer return
- Physical exams to check overall health and catch problems early
These tests help find problems early, when they’re easier to handle.
Managing Late-Appearing Side Effects
Some chemotherapy side effects show up months or years later. These can include neuropathy, cognitive changes, or a higher risk of secondary cancers.
Managing these side effects needs ongoing monitoring and talking with the healthcare team. Patients should tell their doctors about any new or worsening symptoms right away.
Transitioning to Survivorship Care
As time goes on after chemotherapy, care shifts to survivorship. This involves working together between the patient, primary care doctors, and oncologists for long-term care.
Survivorship care plans cover ongoing needs. This includes managing late effects, watching for recurrence, and promoting health and well-being.
Chemotherapy Success Rates and Factors Affecting Outcomes
Chemotherapy’s success depends on many things. It’s key to know what affects it.
Understanding Success Metrics in Cancer Treatment
Chemotherapy success is measured in several ways. These include reducing cancer cells, improving survival rates, and improving life quality. Overall response rate (ORR), progression-free survival (PFS), and overall survival (OS) are important metrics.
A study in the Journal of Clinical Oncology found that chemotherapy success varies. It ranges from 20% to 80% across different cancers.
“The variability in response rates shows why personalized treatment is so important.”
Journal of Clinical Oncology
Factors That Influence Treatment Effectiveness
Many things can affect how well chemotherapy works. These include the cancer type and stage, the patient’s health, and the chemotherapy used. Genetic mutations in cancer cells also play a role.
| Factor | Description | Impact on Chemotherapy |
| Cancer Type | The specific type of cancer being treated. | Different cancers respond differently to chemotherapy. |
| Cancer Stage | The extent or spread of the cancer. | Early-stage cancers may respond better to chemotherapy. |
| Patient’s Health | The patient’s overall health and presence of comorbidities. | Patients with better overall health may tolerate and respond better to chemotherapy. |
Realistic Expectations About Outcomes
Patients should have clear expectations about chemotherapy. It can cure some cancers but control symptoms or slow the disease in others.
Combining Chemotherapy with Other Treatments
Using chemotherapy with other treatments like surgery, radiation therapy, or immunotherapy can improve results. This approach attacks cancer from all sides.
- Surgery can remove the bulk of the tumor.
- Radiation therapy can target specific areas where cancer cells may remain.
- Immunotherapy can stimulate the immune system to fight cancer cells more effectively.
Understanding what affects chemotherapy success and combining treatments can lead to better care. Healthcare providers can tailor treatment to each patient’s needs.
Conclusion: Life After Chemotherapy
Finishing chemotherapy is a big win for cancer patients. We’ve talked about the journey through treatment, managing side effects, and staying healthy. Life after chemotherapy starts a new chapter, focusing on recovery and care.
Survivors often share their stories of strength and hope. They show that life after chemotherapy can be rewarding. Recovery from chemotherapy needs ongoing care and support.
Survivorship care plans are key for monitoring health, managing late side effects, and moving into long-term recovery.
Patients must keep following their doctor’s advice for follow-up care and monitoring. This includes regular check-ups, tests, and screenings to keep them healthy.
Understanding the value of survivorship care and recovery helps patients prepare for life after treatment. We urge patients to stay informed, seek help when needed, and focus on their health as they move forward.
FAQ
What is chemotherapy, and how does it work?
Chemotherapy is a treatment for cancer that uses drugs. It targets cells that grow fast, like cancer cells. It tries to harm these cells less than healthy ones.
How long is a typical chemotherapy session?
Chemotherapy sessions can last from a few minutes to hours. This depends on the drugs and your treatment plan.
What are the common side effects of chemotherapy?
Side effects include nausea, fatigue, hair loss, and a higher risk of infection. The side effects and how bad they are can vary.
Can I have visitors during chemotherapy?
Yes, you can have visitors, but follow the rules of the healthcare facility. This helps prevent infections.
How long does the entire chemotherapy process take?
Chemotherapy’s length varies a lot. It depends on the cancer type, stage, and how well you respond. It can last months to years.
What happens during a chemotherapy treatment cycle?
A cycle includes treatment and rest. For example, a 21-day cycle might have treatment on day one and 20 days of rest before starting again.
How does chemotherapy affect the immune system?
Chemotherapy weakens the immune system by lowering white blood cells. This makes you more likely to get infections. You might need to avoid crowded places or sick people.
What are the signs that chemotherapy is working?
Signs include smaller tumors, better symptoms, and positive test results. These show that the treatment is effective.
What can I expect after my last chemotherapy treatment?
After your last treatment, your body will need time to recover. You’ll manage side effects, have follow-up appointments, and slowly get back to normal.
How is follow-up care managed after chemotherapy?
Follow-up care includes regular check-ups and tests. It also involves managing any late side effects.
What factors affect the success of chemotherapy?
Success depends on the cancer type, stage, your health, and how well the treatment works.
Can chemotherapy be combined with other treatments?
Yes, chemotherapy is often used with surgery, radiation, or targeted therapy. This can make treatment more effective.
How can I manage chemotherapy side effects?
Managing side effects involves medical help, lifestyle changes, and complementary therapies. This includes medicines for nausea, dietary changes, and rest.
What dietary recommendations are there during chemotherapy?
Eat a balanced diet, stay hydrated, and adjust your diet for nausea and appetite changes during chemotherapy.
Is exercise safe during chemotherapy?
Generally, yes, exercise is safe during chemotherapy. But talk to your healthcare team about the right amount and type of exercise for you.
References
- Van Soom, T. (2020). The effects of chemotherapy on energy metabolic aspects: A systematic review. Clinical Nutrition ESPEN, 37, 1-9. https://pubmed.ncbi.nlm.nih.gov/31420208/