Last Updated on November 27, 2025 by Bilal Hasdemir
A significant number of men have prostate surgery each year, and many wonder about their long-term survival prospects. Research shows that the life expectancy after prostate removal is generally high, giving hope to those diagnosed with prostate cancer. Studies indicate that the 20-year survival rate for prostate cancer patients is substantial, with many living well beyond 15 to 20 years following surgery, especially when diagnosed early and treated effectively. This positive outlook highlights the effectiveness of prostatectomy in managing prostate cancer and improving long-term outcomes.
It’s important to understand what affects life expectancy after prostate removal. Studies on omega-3 fatty acids and immune functions show the value of medical research. They help us understand patient outcomes and improve survival rates.
It’s important for patients to know about prostate gland removal procedure. Prostate surgery is done for different reasons. Mainly, it’s for treating prostate cancer or benign prostatic hyperplasia (BPH).
There are many types of prostate surgery. Each has its own reasons, benefits, and risks. The right surgery depends on the patient’s health and the cancer’s stage.
Radical prostatectomy removes the prostate gland and some nearby tissue. It’s mainly for treating prostate cancer that’s only in the prostate. There are open, laparoscopic, and robotic-assisted ways to do this surgery.
TURP helps with BPH by removing prostate tissue that blocks urine flow. It’s done through the urethra, so there are no big cuts. This makes it less invasive than radical prostatectomy.
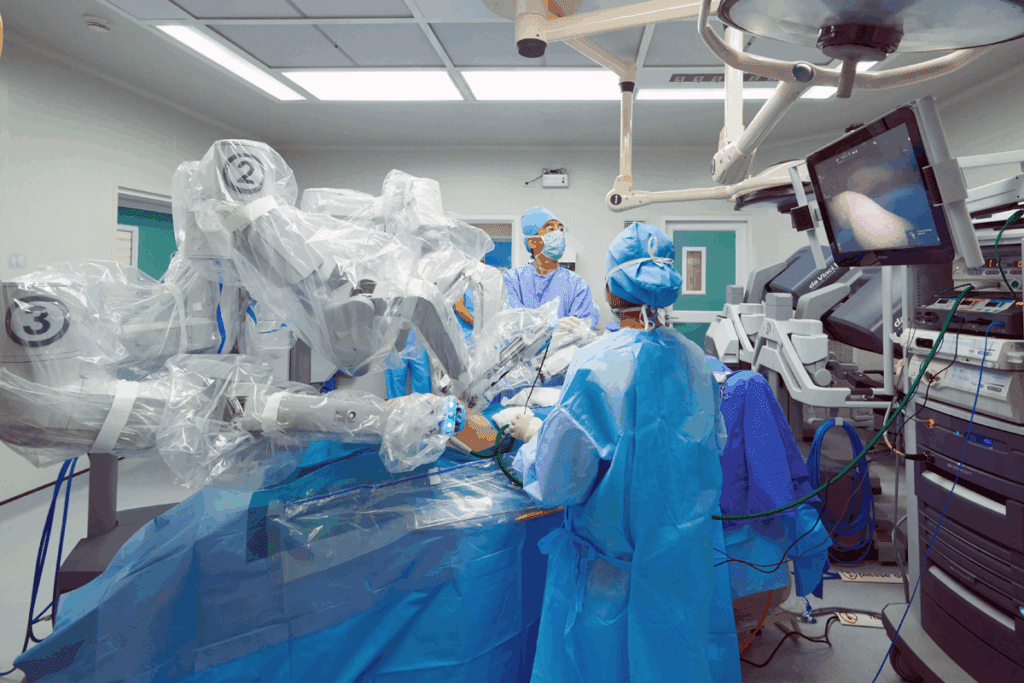
Robotic-assisted laparoscopic prostatectomy is a new, less invasive way to remove the prostate. It uses a robotic system to help the surgeon. This method might lead to fewer complications and a faster recovery than open surgery.
Even though these surgeries work well, they can have prostatectomy complications. It’s key for patients to know about these risks. This helps them make better choices about their treatment.
Many wonder, “Can men live without a prostate?” Yes, men can live without a prostate. But, they might notice changes in how they pee and have sex. Getting used to life without a prostate means understanding these changes and how to handle them.
Men’s health is greatly affected by the prostate gland. It does more than just help with reproduction. The prostate gland is key to both urinary and reproductive health.
The prostate gland is about the size of a walnut. It’s located below the bladder, around the urethra. It has three main roles: reproductive health, urinary system involvement, and hormonal interactions.
The prostate gland is vital for reproductive health. It secretes fluids that make up semen. These fluids nourish and protect sperm, helping with fertility.
Key Functions in Reproductive Health:
The prostate gland surrounds the urethra, which carries urine out of the body. As men age, the prostate can grow, narrowing the urethra. This can affect how well urine flows.
| Urinary Symptoms | Possible Causes |
| Weak or interrupted urine flow | Enlarged prostate |
| Frequent urination | Prostate issues or other urinary tract problems |
| Difficulty starting urination | Prostate enlargement or urethral constriction |
The prostate gland interacts with hormones like testosterone and dihydrotestosterone (DHT). DHT is a strong form of testosterone that helps the prostate grow.
The balance between testosterone and DHT is key for prostate health. Imbalances can cause problems like BPH or prostate cancer.
Understanding the prostate gland’s role is vital for men’s health. While the prostate is important, the body can adjust without it. Knowing its functions helps manage side effects and maintain quality of life.
Many patients wonder if they can live normally after their prostate is removed. The prostate gland is key to the male reproductive system. But, removing it, or prostatectomy, might be needed for health issues like prostate cancer.
After the prostate is gone, the body makes changes. The urethra is connected to the bladder again. This lets men keep urinating, but they might notice changes in how they control it.
Men might face incontinence or urinary leakage right after surgery.
Even without the prostate, many functions stay the same. Men can have orgasms, but the ejaculation process is altered. This is because the prostate and seminal vesicles are either removed or their function is disrupted.
Most men can get back to their usual activities a few weeks to months after surgery.
Some systems need time to adjust after the prostate is removed. Urinary control is one, as men might need to do Kegel exercises to strengthen their pelvic floor muscles. They also might face changes in sexual function, like erectile dysfunction. This can be treated with various methods.
In summary, living without a prostate means some changes and adjustments. But, many men can live active and happy lives after prostate removal. Knowing what happens after surgery helps men prepare and manage their condition well.
Many things can affect how long you live after having your prostate removed. These include your overall health and the cancer’s stage when you’re diagnosed. Knowing these can help you understand what to expect after surgery.
Research shows that most men live a long time after prostate removal, if the cancer is caught early. In fact, over 98% of men with early-stage prostate cancer live for at least 10 years after surgery.
The outlook can change if the cancer has spread. Men with cancer that’s only in the prostate have a much better chance of survival than those with more advanced cancer.
Several things can affect how long you live after prostate removal. These include:
Studies suggest that men with early-stage prostate cancer live as long as the average man, if they don’t have other health problems. But, men with more advanced cancer may face a different future.
Talking to your doctor about your situation can help you understand your life expectancy after prostate removal.
The 20-year survival rate for prostate cancer is a key indicator of the disease’s outlook. It helps patients and doctors make better treatment choices.
Survival rates for prostate cancer change a lot based on the stage at diagnosis. Those with localized cancer have a much better chance of survival than those with more advanced cancer.
| Cancer Stage | 20-Year Survival Rate |
| Localized | 85-90% |
| Regional | 60-70% |
| Distant | 30-40% |
Table: 20-Year Survival Rates by Cancer Stage
Medical technology and treatment strategies have improved over time. This has led to better survival rates for prostate cancer patients. Early detection and more effective treatments have helped a lot.
Many things affect how long prostate cancer patients can live, like age, health, and treatment success. Lifestyle changes and ongoing care also matter a lot.
Knowing these factors helps patients make better choices about their treatment. This can improve their long-term outlook.
It’s important for patients to know about the possible complications after prostatectomy. This surgery is done to treat prostate cancer or an enlarged prostate by removing part or all of the gland. While it’s often effective, it can cause different issues.
Right after surgery, patients might face infections, bleeding, or reactions to anesthesia. These problems are common and usually handled well by doctors. But, they can slow down recovery and affect the surgery’s success.
Patients may struggle with urinary incontinence, erectile dysfunction, and pain or discomfort at the surgery site in the short term. These issues are usually temporary but can last differently for everyone.
| Challenge | Description | Typical Duration |
| Urinary Incontinence | Loss of bladder control | Several weeks to months |
| Erectile Dysfunction | Difficulty achieving or maintaining an erection | Varies, potentially long-term |
| Surgical Site Discomfort | Pain or discomfort at the site of surgery | Several weeks |
Long-term side effects can include ongoing urinary incontinence, erectile dysfunction, and changes in how you urinate. How these side effects affect you can vary a lot.
Managing Long-term Side Effects: Patients can work with their doctors to manage these side effects. This can include treatments and changes in lifestyle. Knowing about these long-term effects is key to making the right choice about prostatectomy.
Life after prostate surgery brings many changes that affect a man’s quality of life. The removal of the prostate gland, for cancer or other reasons, is a big change. It impacts a man’s health and well-being in many ways.
Prostate removal changes how men urinate. They might leak urine or need to go more often. But, many men get better with time and exercises.
Some men leak urine when they cough or sneeze. To manage this, they might need to change their lifestyle or get medical help.
Prostate removal can also affect a man’s sex life and ability to have children. Erectile dysfunction is a common side effect. The surgery’s method can affect how much it impacts a man’s sex life.
It can also make it hard to ejaculate. But, nerve-sparing techniques can help keep some sexual functions.
The emotional and psychological effects of prostate removal are important. Men might feel anxiety or depression due to the changes and adjusting to life without a prostate.
Support from doctors, family, and support groups is key. It helps men deal with these feelings. Talking openly with healthcare providers is also important.
In summary, prostate removal surgery changes a man’s life a lot. But, understanding these changes and getting support can help improve life after surgery.
Understanding life expectancy after prostate removal and radiation is key. It requires a deep look into how treatments work together.
When prostate cancer is treated with surgery and radiation, the goal is to increase survival chances. This method is often chosen for high-risk or advanced cancer cases.
The choice to use both surgery and radiation depends on several factors. These include the cancer’s stage and grade, the patient’s health, and the risk of cancer coming back.
Adjuvant radiation therapy is given after surgery. It aims to kill any cancer cells left behind, lowering the chance of cancer coming back.
Neoadjuvant therapy involves radiation or hormone treatment before surgery. It helps shrink the tumor, making it easier to remove.
Research shows that adjuvant radiation therapy can boost survival rates for some patients. This is true for those with certain cancer features.
A study in a major medical journal found that adjuvant radiation therapy improved survival. It did so for patients with prostate cancer.
The use of adjuvant therapy has been linked to better outcomes for high-risk prostate cancer patients. This highlights the value of combining treatments.
It’s vital to manage side effects from combined treatments to keep patients’ quality of life high.
Side effects include urinary issues, erectile dysfunction, and bowel problems. A team of specialists helps manage these. They include urologists, radiation oncologists, and supportive care experts.
Patients should talk to their healthcare team about side effects. This ensures the best possible results.
Understanding the effects of combined treatments on life expectancy and quality of life is important. It helps patients and doctors make informed treatment choices.
Living without a prostate means making some changes. But many men find it easy to adjust. Knowing what to expect helps make the transition smoother.
After prostate surgery, staying active is key. It helps you regain strength and boosts your health. Walking, swimming, and cycling are great exercises to start with.
Start slow and gradually increase your workout intensity and time. Always talk to your doctor before starting any new exercise. They can make sure it’s right for you.
Eating right is important for recovery and health after prostate surgery. Increasing fiber intake helps with bowel changes. Eating foods high in antioxidants, like fruits and veggies, is good too.
Try to avoid foods that might upset your stomach or cause urinary problems. Drinking lots of water is also key.
Prostate removal can change how you feel about sex and intimacy. Talking to a doctor can help you understand these changes. Nerve-sparing techniques during surgery might help keep sexual function intact.
Talking openly with your partner about your feelings and needs can strengthen your bond. Getting help from counselors or support groups can also be helpful.
Remember, intimacy is more than just sex. Exploring new ways to connect with your partner can keep your relationship strong.
The field of prostate surgery is changing fast. New technologies and better surgical methods are helping patients. Now, there are more effective and less invasive treatments available.
New tech has greatly improved prostate surgery. Robotic-assisted surgery is a big hit because it’s precise and doesn’t hurt as much. It lets surgeons do tricky operations with better results, making recovery faster and outcomes better.
“The use of technology in prostate surgery has changed the game,” says a top urologist. “Robotic systems give surgeons amazing control and vision. This means they can save more tissue and cut down on problems.”
Nerve-sparing surgery has made a big difference. It lowers the chance of problems like incontinence and impotence. This method carefully keeps the nerves around the prostate safe, which is key for bladder and sex functions.
The nerve-sparing prostatectomy has been a game-changer. It helps patients keep a better quality of life after surgery. Research shows that those who get this surgery are more likely to stay continent and potent.
New treatments are giving prostate cancer patients hope. Focal therapy focuses on specific parts of the prostate, causing less damage. Other new treatments include immunotherapy and targeted therapy. These aim to use the body’s immune system and target cancer cells more precisely.
As research keeps going, these new treatments will likely be key in prostate cancer care. They offer patients more tailored and effective options.
Knowing how long you might live after having your prostate removed is key for those with prostate cancer. The chances of survival and how well you’ll feel after surgery are big worries for both patients and doctors.
Thanks to new medical tech and treatments, more people are beating prostate cancer. How long you might live after surgery depends on when you were diagnosed and your overall health.
After surgery, some men might face changes in how they pee and have sex. But, with the right care, many men can live happy, active lives. Understanding these factors helps people make better choices about their treatment.
Yes, living without a prostate is possible. The prostate gland is important for reproductive health and urine flow. But, removing it doesn’t affect how long you live.
The time you live after prostate surgery depends on many things. These include the cancer’s stage, your health, and the treatment you get. Studies show men can live as long as others after surgery.
After prostate surgery, some common issues are trouble with urine, sex problems, and bowel issues. Right after surgery, you might face bleeding, infection, or reactions to anesthesia.
Removing the prostate can change how you urinate, leading to leaks or incontinence. But, many men see their urine function improve with time and the right care.
The 20-year survival rate for prostate cancer changes based on when you’re diagnosed. Men with cancer that’s only in the prostate have a good chance of survival. But, those with more advanced cancer face a tougher road.
Yes, many men can have a normal sex life without a prostate. Surgery can affect sex, but there are treatments to help. Erectile dysfunction is common, but it’s not the end.
Robotic-assisted surgery for the prostate has many benefits. It means smaller cuts, less blood loss, and a quicker recovery. It also lowers the risk of problems and can lead to better results.
Radiation therapy can help improve outcomes after removing the prostate. Its effect on life expectancy depends on the cancer’s stage and your overall health.
Eating well is key to life without a prostate. Focus on fruits, veggies, and whole grains. You might also need to adjust your diet for better urine and bowel health.
Yes, new treatments for prostate cancer are being developed. These include new surgeries, radiation methods, and targeted therapies. They aim to better outcomes and fewer side effects.
Men can keep their relationships strong after prostate surgery by talking openly with their partner. Seeking counseling and exploring treatments for sex problems can also help.
The prostate gland is vital for reproductive health, helping sperm. It also plays a role in the urinary system, surrounding the urethra.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!