Last Updated on November 27, 2025 by Bilal Hasdemir

Prostate cancer is a big worry for men, mainly in the United States. The American Cancer Society says it’s the second leading cause of cancer death in men. Surgery is a common choice for treatment. But, knowing the possible outcomes and regret rates for prostate surgery is key.Learn about what is the regret rate for prostate surgery, with stats, patient reviews, and images to help you make informed treatment decisions.
A study in the Journal of Clinical Oncology showed a 14.6% regret rate for prostate surgery. The Gleason scale is very important for prostate cancer treatment. It helps predict the outcome and treatment plan.
Prostate cancer is a big problem in America, with over 190,000 new cases in 2020. It affects not just the men who get it, but also their families and communities.
The risk of getting prostate cancer changes based on who you are. The American Cancer Society says age, family history, and ethnicity play a big role. Men over 65 and those with a family history are at higher risk.
African American men face a higher risk and death rate from prostate cancer. Knowing this helps doctors target prevention and treatment better. They can give more tailored care to those at higher risk.
Getting a prostate cancer diagnosis can deeply affect a man. It can cause anxiety, fear, and uncertainty about the future. It also affects his loved ones.
Support groups and counseling are key in helping patients deal with their diagnosis. Healthcare providers should offer care that addresses both physical and emotional needs.
The problem of prostate cancer overtreatment is also a big worry. Overtreatment can cause unnecessary side effects and harm quality of life. It’s important to find the right balance in treatment to avoid overtreatment.
Knowing about the Gleason score is key for prostate cancer patients. The Gleason scoring system grades prostate cancer by looking at tumor tissue under a microscope.
Pathologists look at prostate tissue to grade it. They use the Gleason score, which adds the grades of two cell growth patterns. Grades range from 1 (most like normal tissue) to 5 (most abnormal).
The score is a sum of these grades, from 2 to 10. For example, a score of 7 might be 3+4. This helps figure out how aggressive the cancer is.
“The Gleason score remains one of the most powerful prognostic factors for prostate cancer, helping guide treatment decisions.”
Gleason scores play a big role in deciding how to treat prostate cancer. Lower scores (like 6 or less) mean less aggressive cancer. This might mean watching and waiting, or surgery or radiation.
Higher scores (like 8 or higher) mean more aggressive cancer. This usually means more urgent and aggressive treatments.
| Gleason Score | Cancer Aggressiveness | Typical Treatment Approach |
| 6 or less | Less aggressive | Active surveillance, surgery, or radiation |
| 7 | Moderately aggressive | Surgery or radiation, potentially with hormone therapy |
| 8 or higher | More aggressive | Surgery, radiation, hormone therapy, or a combination |
The Gleason scoring system is vital for figuring out the prognosis and treatment plan for prostate cancer patients.
When you’re diagnosed with prostate cancer, knowing about surgery is key. Removing the prostate gland is a common treatment for early cancer. It helps get rid of the cancer while trying to keep your urinary and sexual functions.
Radical prostatectomy is a surgery to remove the prostate gland. It aims to get rid of prostate cancer by taking out the gland and some nearby tissue. The goal is to remove the cancer and keep your urinary and sexual functions as good as they can be.
Key aspects of radical prostatectomy include:
There are two main ways to do radical prostatectomy: open surgery and robotic-assisted laparoscopic surgery. The choice depends on your health, the surgeon’s skill, and the cancer’s details.
| Aspect | Open Surgery | Robotic-Assisted Surgery |
| Incision | Single, larger incision in the abdomen or perineum | Several small incisions for laparoscopic instruments |
| Blood Loss | Generally more | Less due to precise dissection |
| Recovery Time | Typically longer | Shorter, with less post-operative pain |
Recovery from prostate surgery varies. Knowing the general timeline helps manage your expectations. Your recovery depends on the surgery type, your age, and health.
The recovery process includes:
Talking to your healthcare provider about your situation and concerns is important. They can give you personalized advice on what to expect during recovery.
Radiation therapy is a key treatment for prostate cancer. It uses high-energy rays to kill cancer cells or slow their growth. This is a non-surgical option for men with prostate cancer.
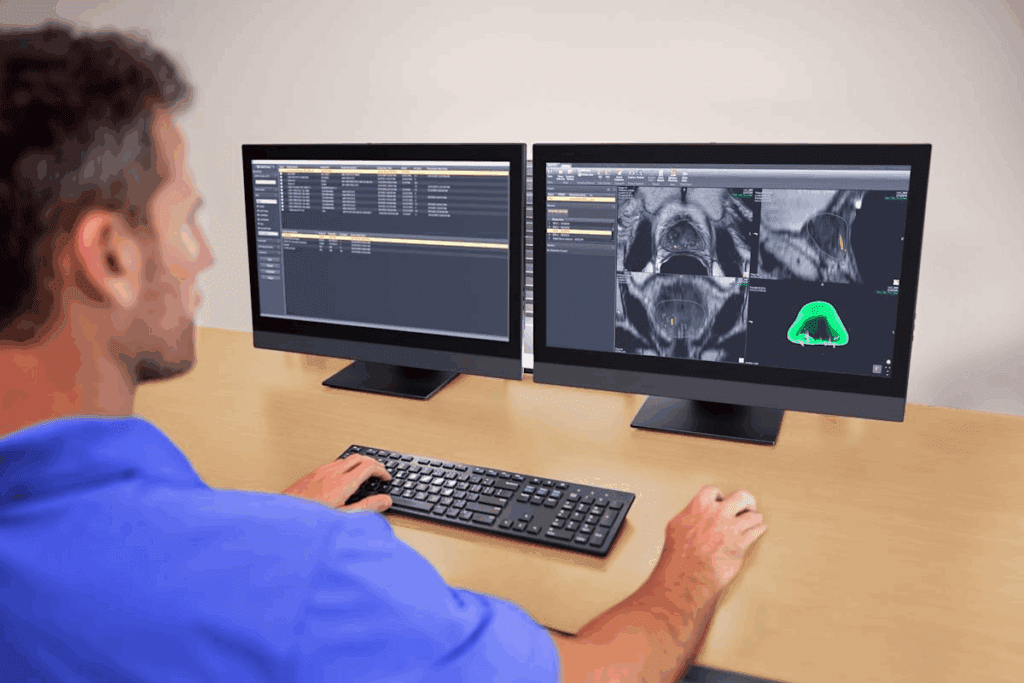
External Beam Radiation Therapy (EBRT) is a common treatment for prostate cancer. It uses high-energy beams from outside the body to target and destroy cancer cells. Treatments are given five days a week for several weeks.
Benefits of EBRT: It can treat the prostate and surrounding tissues where cancer might have spread. Advanced techniques like IMRT and IGRT help deliver precise doses to the tumor while protecting healthy tissues.
Brachytherapy involves placing small radioactive seeds in the prostate gland. These seeds emit radiation that kills cancer cells over time. There are two types: permanent (low-dose rate) and temporary (high-dose rate).
“Brachytherapy offers a highly effective treatment for localized prostate cancer, with the advantage of delivering radiation directly to the tumor site, reducing side effects.” -American Cancer Society
Advantages of Brachytherapy: It delivers a high dose of radiation directly to the prostate, minimizing damage to surrounding tissues. The procedure is quick, and many men can go home the same day.
Proton therapy uses protons instead of X-rays to kill cancer cells. It is useful for tumors close to sensitive areas, as it delivers a high dose to the tumor while sparing surrounding tissues.
| Therapy Type | Description | Benefits |
| EBRT | External beam radiation targeting cancer cells | Non-invasive, can treat larger areas |
| Brachytherapy | Internal radiation via radioactive seeds | Direct delivery to tumor, fewer side effects |
| Proton Therapy | Proton beam radiation for precise targeting | High precision, spares sensitive tissues |
Each radiation therapy approach has its own benefits and drawbacks. The choice depends on the cancer’s stage and grade, the patient’s health, and personal preferences. It’s important to consult with a healthcare provider to find the best treatment plan.
Understanding the regret rate for prostate surgery is key for men with prostate cancer. Making treatment choices is big, and knowing about regret can help patients decide better.
Treatment regret in prostate cancer means feeling unhappy or regretful after a treatment, like surgery. It covers physical effects, emotional health, and how it affects daily life.
Research shows regret comes from not meeting expectations, unexpected side effects, or health changes after treatment. Doctors need to understand this to help patients better.
A study in the Journal of Clinical Oncology found a 14.6% regret rate for prostate surgery in long-term survivors. This shows how important it is to listen to patients and measure treatment success by how they feel.
More research is coming, giving deeper insights into what causes regret and how it affects different people.
Some factors are linked to more regret after prostate surgery. These include age, starting health, and cancer stage.
Younger men and those with good health before surgery might regret more because side effects hit them harder. Older men or those with advanced cancer might have different feelings about regret.
It’s important to know the regret rates for surgery and radiation in prostate cancer. Patients with localized prostate cancer have to choose between these two main treatments.
Studies have looked at how happy patients are with surgery and radiation for prostate cancer. A review of 14 studies found 20% of patients with localized prostate cancer regret their choice. This shows regret rates can vary a lot.
Comparative studies show both treatments have good and bad sides. A study in the Journal of Clinical Oncology found differences in how patients feel after surgery or radiation. These differences affect urinary, sexual, and bowel functions.
Regret can happen soon after treatment or years later. Short-term regret often comes from side effects like incontinence or erectile dysfunction after surgery.
Long-term regret might come from how well the treatment lasts and late side effects. A study found regret rates can go down as patients get used to their treatment outcomes.
PROMs are key in seeing how well prostate cancer treatments work from the patient’s view. They track symptoms, function, and quality of life. This gives insights into surgery and radiation outcomes.
PROMs are vital in comparative effectiveness research. They help show the real differences in outcomes that patients care about. Understanding PROMs helps doctors support patients in choosing the right treatment.
It’s important to know why some people regret having prostate surgery. Deciding on prostate cancer treatment is complex. Many factors can affect how satisfied a patient is with their choice.
Urinary incontinence is a big side effect of prostate surgery. Studies have shown many patients deal with incontinence after surgery. This can really change their life.
“The loss of bladder control can be distressing and affect daily activities,” notes a study on post-prostatectomy incontinence.
Erectile dysfunction (ED) is another common issue after prostate surgery. How much ED varies, but it’s a big worry for many. The risk of erectile dysfunction is a critical factor in the decision-making process for men considering prostate surgery.
Pain and recovery issues can also lead to regret. Some patients face long recovery times or chronic pain. This can be hard to deal with.
“Pain management after prostate surgery is critical, and unrelieved pain can significantly affect a patient’s recovery and overall satisfaction with their treatment choice.”
The psychological effects of prostate surgery are important. Changes in how you pee and have sex can cause depression, anxiety, and lower your quality of life. Support from healthcare providers and support groups is key in dealing with these changes.
In conclusion, prostate surgery is a treatment option for prostate cancer. But, knowing the possible regrets is key. Understanding issues like incontinence, erectile dysfunction, pain, and mental health impacts helps patients make better choices.
In the United States, the treatment of prostate cancer is a big topic. People wonder if men prefer surgery or radiation therapy. Choosing between these treatments is complex and depends on many factors.
Recent studies show most men with localized prostate cancer choose surgery. In the United States, surgery, like radical prostatectomy, is a top choice for treating prostate cancer.
Many choose surgery because it seems to remove cancer well. But, radiation therapy, like EBRT and brachytherapy, is also a good option for many patients.
| Treatment Type | Percentage of Patients | Average Recovery Time |
| Surgery (Radical Prostatectomy) | 55% | 6-12 weeks |
| Radiation Therapy | 35% | Varies by type |
| Active Surveillance | 10% | Ongoing monitoring |
Many things affect whether someone chooses surgery or radiation. These include the cancer’s stage and grade, the patient’s age and health, and what they prefer in terms of side effects and recovery time.
Key factors influencing treatment preferences include:
It’s important for patients and doctors to understand these factors. This helps make informed decisions about prostate cancer treatment.
Overtreatment of prostate cancer is a big problem. It affects patients’ quality of life and the healthcare system. It happens when men with low-risk prostate cancer get too aggressive treatments. These treatments might not really help them live longer.
Overtreatment is when the risks of treatment are too high, like in low-risk prostate cancer. This cancer is low-risk if the Gleason score is low, PSA levels are low, and the tumor is small. Men with these signs might not need aggressive treatment right away.
Active surveillance is often suggested for low-risk prostate cancer. It means watching the cancer closely with PSA tests, exams, and biopsies. But, some men might choose or be advised to get more serious treatments like surgery or radiation.
The Skid Row Cancer Study showed that some groups get too much treatment for prostate cancer. It found that men from tough backgrounds often get aggressive treatments, even if their cancer is low-risk. This shows we need fair access to care and to make informed choices.
“The overtreatment of prostate cancer is a complex issue, influenced by various factors including patient and physician preferences, as well as healthcare system characteristics.” -Expert Opinion
Overtreatment of prostate cancer has big costs. It costs a lot of money and can make men feel anxious, depressed, and lower their quality of life. This is because of the side effects from treatments.
It’s important to know the risks and benefits of treatments. Men should talk to their doctors about their own situation. This way, they can avoid getting too much treatment.
Active surveillance is becoming a smart choice for managing low-risk prostate cancer. It focuses on watching the cancer instead of treating it right away. This method is best for men with prostate cancer that’s not a big threat to their lives.
Not every man with prostate cancer is right for active surveillance. It’s mainly for those with low-risk cancer. This means a low Gleason score, low PSA level, and small tumor size.
Choosing active surveillance means weighing many things. These include the patient’s health, how long they might live, and what they want. It’s a choice that needs a lot of confidence in watching the cancer and knowing the risks and benefits.
Active surveillance means watching the cancer closely. This is to catch any changes that might mean it’s time for more treatment. The monitoring includes regular PSA tests, biopsies, and sometimes MRI scans.
“Active surveillance isn’t for everyone,” says a urologist. “It needs to be tailored to each patient’s cancer and health.”
Many men on active surveillance are very happy with their choice. They like avoiding the side effects of aggressive treatments. This is a big reason for their happiness.
Active surveillance also gives men a sense of control. They’re involved in watching their cancer and making decisions about it.
One patient said, “Choosing active surveillance was freeing. It let me skip the side effects of surgery or radiation, while keeping an eye on my cancer.”
Choosing between removing the prostate or radiation therapy is a big decision for men with prostate cancer. It depends on the cancer’s stage, the patient’s health, and what they prefer. This includes looking at possible side effects and treatment results.
Oncological outcomes measure how well a treatment works against cancer. Both surgery and radiation can treat prostate cancer well. But, results can differ based on the cancer and the patient’s health.
A study showed both surgery and radiation can fight prostate cancer effectively. The right choice depends on the cancer’s stage, the patient’s health, and other factors.
Key Considerations:
Both removing the prostate and radiation therapy have side effects that can affect life quality. Knowing these side effects is key to making a good choice.
Surgery can cause trouble with urination and sex. Radiation might lead to tiredness, urinary issues, and bowel problems. How bad these side effects are can vary a lot.
“The decision between surgery and radiation therapy should be based on a thorough discussion between the patient and his healthcare provider, considering the patient’s preferences, the cancer’s characteristics, and the possible side effects of each treatment.”
Personalized decision-making looks at each patient’s unique situation. This includes their health, cancer details, and personal values.
Decision-making frameworks help by listing important factors and possible outcomes. They help patients and doctors make choices that fit each person’s needs.
Steps in Personalized Decision-Making:
By carefully thinking about these points and using decision-making frameworks, patients can make choices that are right for them.
When you face prostate cancer, choosing the right treatment is key to avoid regret later. Men with this disease can greatly benefit from knowing their options and what each might bring.
Talking thoroughly with your healthcare team is vital. Asking the right questions helps you understand your treatment choices. Here are some important ones to ask:
Getting a second opinion is very helpful. It lets you check your diagnosis and treatment plan with another expert. This can reveal new options or confirm the first plan.
Being part of support groups and using patient resources is also key. These places offer advice and support from others who’ve been through similar things. They provide both emotional and practical help.
By being proactive and well-informed, men with prostate cancer can reduce regret. This approach can also enhance their overall health and happiness.
It’s important for men with prostate cancer to know about the regret rate for surgery. Choosing between surgery and radiotherapy is tough. It depends on the cancer stage, health, and personal choices.
Studies show that both treatments have good and bad sides. The regret rate differs for each patient. Things like urinary issues, erectile problems, and life quality changes matter a lot.
Men facing this decision should talk openly with their doctors. They should think about the advantages and disadvantages of each choice. Getting a second opinion and joining support groups can also help.
In short, surgery or radiotherapy are both valid options for treating prostate cancer. Knowing the possible outcomes and regret rates helps patients make better choices. This can lead to a better life and more satisfaction with treatment.
The Gleason scale grades prostate cancer based on tumor tissue appearance. It ranges from 2 to 10. Higher scores mean more aggressive cancer.
Regret rates for prostate surgery vary. Most men are happy with their choice. But, urinary issues, erectile problems, and recovery issues can affect regret.
In the U.S., both surgery and radiation are common for prostate cancer. The choice depends on cancer stage, health, and personal preference.
Choosing between surgery and radiation depends on personal circumstances. Both have benefits and drawbacks. Consider oncological outcomes and side effects when deciding.
Overtreatment happens when men with low-risk cancer get aggressive treatment. The Skid Row Cancer Study showed its economic and psychological costs.
Active surveillance is for men with low-risk cancer. It involves regular monitoring instead of immediate treatment. It’s good for avoiding unnecessary treatment.
Gleason scores are key in prostate cancer treatment. Higher scores mean more aggressive cancer. Treatment plans often depend on the score.
Common regrets include urinary issues, erectile dysfunction, pain, and recovery problems. The psychological impact is also a factor. Knowing these can help in making treatment choices.
Men can reduce regret by asking doctors questions, getting second opinions, and using support groups. This helps make choices that fit their needs and preferences.
Radical prostatectomy removes the prostate gland surgically. Radiation therapy kills cancer cells with high-energy rays. Both have benefits and drawbacks, depending on individual circumstances.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!