Last Updated on November 25, 2025 by
The Prostate-Specific Antigen (PSA) test has been key in prostate cancer screening for years. But, its use is now debated due to its limits and risks.
Understanding what PSA stands for and its implications is key for men thinking about this test. The National Cancer Institute says the PSA test checks the blood for prostate-specific antigen. High levels might mean prostate cancer.
But, a high PSA level doesn’t always mean cancer. It can also show other prostate problems. As we look into the PSA test debate, we must consider its benefits and risks. Risks include overdiagnosis and unnecessary treatments.
Knowing how PSA helps in cancer screening is key for good prostate health. The Prostate-Specific Antigen (PSA) test checks PSA levels in blood. But, what does it really tell us about our prostate?
The PSA test looks at the prostate-specific antigen, a protein from the prostate gland, in blood. High PSA levels might show prostate problems, like cancer, prostatitis, or BPH. Yet, a high PSA doesn’t always mean cancer. It’s just one clue doctors look at for prostate health.
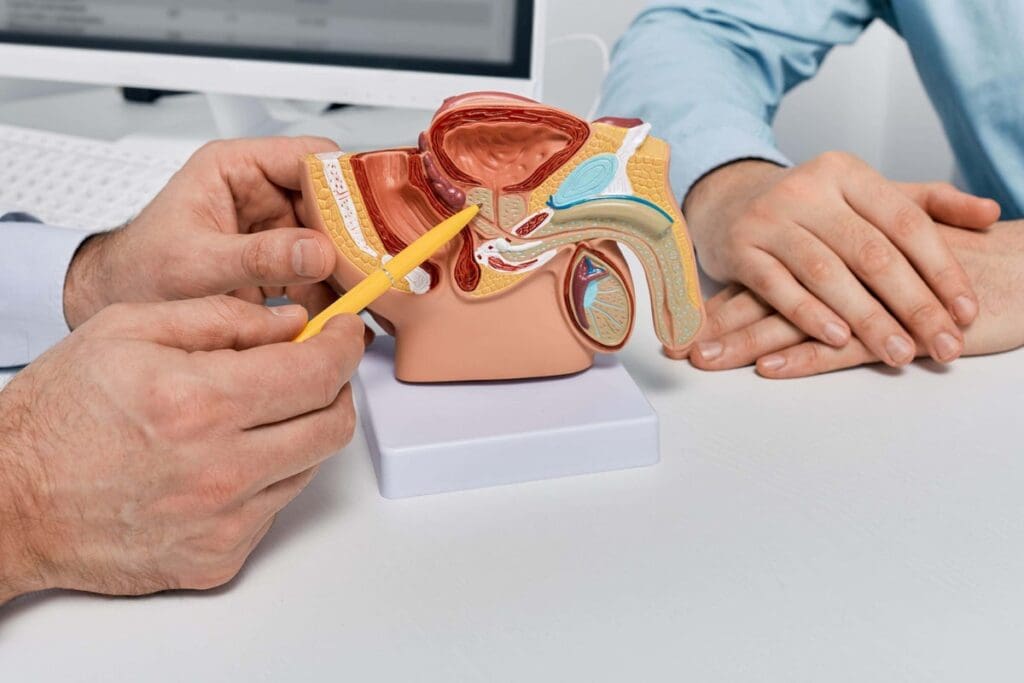
The PSA test goes hand-in-hand with a digital rectal exam (DRE). Together, these tests help find possible issues that need more checking.
Doctors use the PSA test as part of a big plan to find prostate cancer. They look at many things, like age, health history, and overall health, when they see PSA test results. A very high PSA might lead to more tests, like a biopsy, to see if there’s cancer.
Talking about PSA test results with a doctor is very important. Knowing what a dangerous PSA level is can change based on many things. A doctor can give advice based on your test results and health.
Recent studies have shown PSA testing’s limits in cancer diagnosis. The stats on PSA screening accuracy are quite alarming. They need a closer look.
The false-positive rate for PSA testing is about 6-7% in each round. This means a lot of men get false-positive results. They face unnecessary anxiety and more tests.
These false positives can come from things like benign prostatic hyperplasia or inflammation. They don’t always mean cancer.
Also, only 25% of men who get biopsies after a positive PSA test have cancer. This shows the problem of overdiagnosis and the risk of overtreatment.
The other 75% of biopsies don’t find cancer. Yet, these men face the risks of biopsy procedures.

These numbers show we need a better way to screen for prostate cancer. We should think about each person’s risk and the good and bad of testing.
Deciding on a PSA test is complex due to its limits and risks. We explore the challenges of prostate cancer screening. Several key concerns question the usual PSA testing approach.
Many PSA tests show high levels without cancer. This causes worry and more tests, like biopsies. The high rate of false positives shows we need a better way to screen for prostate cancer.
BPH, a non-cancerous prostate growth, affects many older men. It’s behind 86% of non-cancer PSA increases. This makes it hard to know if a high PSA means cancer or not.
PSA screening only slightly lowers prostate cancer death rates. Only 1.3 deaths are avoided per 1,000 men screened over 13 years. This makes us wonder if PSA testing is worth it, considering the risks of more tests and treatments.
PSA tests can lead to unnecessary biopsies. These can cause pain, bleeding, and infection. These problems lower quality of life and increase healthcare costs. The risks make choosing to get a PSA test harder.
In summary, while PSA tests are used to screen for prostate cancer, their limits and risks mean we should be careful. Understanding these issues helps people make better health choices.
It’s important to know the possible side effects of treatments after PSA screening. While PSA screening can find prostate cancer early, the treatments can have big side effects.
Sexual problems are a big issue for many men after prostate cancer treatment. About 50 out of 80 men face sexual issues, which really affects their life quality.
Urinary incontinence is another big problem, hitting about 15 out of 80 men. It can be anything from a little leak to not being able to control your bladder. This might mean using special clothes and can really change your daily life.
A positive PSA test can start a chain of more tests and treatments. Each step has its own risks and side effects. This adds to the patient’s overall burden.
We need to think about these possible problems when we decide if PSA screening is right. Knowing what a positive test might mean helps men make better choices for their health.
Not everyone benefits equally from PSA testing. Some people should be more cautious. The decision to get tested should consider age, health, and risk for prostate cancer.
Men over 70 should be cautious about PSA testing, clinical experts say. The benefits may not be worth the risks for them. At this age, screening can lead to unnecessary treatments that harm quality of life.
For men over 70, the risks of PSA testing often outweigh the benefits. Older men often have other health issues that make treatment decisions harder. The focus should be on maintaining quality of life, not aggressive cancer treatments.
For those at low risk of prostate cancer, watchful waiting is better than immediate PSA testing. These individuals usually have no significant family history of prostate cancer and good health indicators.
“For men at low risk of prostate cancer, the harms of PSA screening, including overdiagnosis and overtreatment, can outweigh the benefits.” – Expert Opinion on Prostate Cancer Screening
Watchful waiting involves monitoring PSA levels over time without immediate intervention. This method allows for early detection of changes in PSA levels. It avoids the risks of unnecessary biopsies and treatments.
In conclusion, men over 70 and those at low risk for prostate cancer should be cautious about PSA testing. Understanding the risks and benefits helps make informed decisions for their health and well-being.
PSA testing is a complex issue that needs careful thought. We must weigh the benefits and limitations of prostate cancer screening. The National Cancer Institute suggests talking to a healthcare provider about PSA testing.
Understanding PSA testing’s role in cancer screening is key. It’s also important to know about test accuracy and treatment risks. By considering these, men can make a choice that fits their situation.
The decision to get a PSA test should be well-informed. We urge men to talk to their healthcare provider. This way, they can find the best option for their health.
PSA stands for Prostate-Specific Antigen. It’s a protein made by the prostate gland.
A PSA test is a blood test. It checks the level of Prostate-Specific Antigen in your blood. It’s used to screen for prostate cancer.
Normal PSA levels change with age. Generally, a level below 4 ng/mL is normal. But, the normal range can differ based on the lab and your age.
A PSA level above 4 ng/mL is usually high. It might mean prostate cancer. But, it can also show other conditions like Benign Prostatic Hyperplasia.
PSA testing screens for prostate cancer by checking PSA levels in the blood. High levels might mean cancer. But, a biopsy is needed to confirm it.
PSA testing has some big limitations. It can have a high false-positive rate. It can’t tell the difference between cancer and non-cancer. It might lead to unnecessary biopsies and treatments.
Men at high risk of prostate cancer should think about PSA testing. This includes those with a family history or African American men. But, the decision to test should be made with a healthcare provider.
PSA testing can have risks. These include unnecessary biopsies, pain, bleeding, and infection. There’s also a chance of overdiagnosis and overtreatment.
Watchful waiting means monitoring PSA levels and symptoms without immediate treatment. It’s often suggested for men with low-risk prostate cancer or a short life expectancy.
Ilic, D., Neuberger, M. M., Djulbegovic, M., & Dahm, P. (2021). Screening for prostate cancer. Cochrane Database of Systematic Reviews, 2021(6), CD004720. https://doi.org/10.1002/14651858.CD004720.pub3
Schröder, F. H., Hugosson, J., Roobol, M. J., Tammela, T. L. J., Ciatto, S., Nelen, V., … Auvinen, A. (2012). Screening and prostate cancer mortality in a randomized European study. New England Journal of Medicine, 366(11), 1‑10. (ERSPC trial)
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!