We are seeing big changes in how we treat acute myeloid leukemia. New discoveries in precision medicine are giving hope to people all over the world. These breakthroughs have led to new treatments like targeted drugs and immunotherapies. They are changing how we care for AML medical patients.
At Liv Hospital, we aim to give top-notch healthcare to everyone. We make sure each patient gets the best treatment for acute myelogenous leukemia for them. Our goal is to keep improving care and find a way to cure AML leukemia.
Key Takeaways
- Precision medicine is revolutionizing acute myeloid leukemia treatment.
- Innovative therapies, including targeted drugs and immunotherapies, are being developed.
- Liv Hospital provides extensive support for international patients.
- Patient-centered care ensures effective treatment tailored to individual needs.
- Ongoing research aims to improve patient outcomes and achieve an AML cure.
Understanding AML Leukemia in 2025
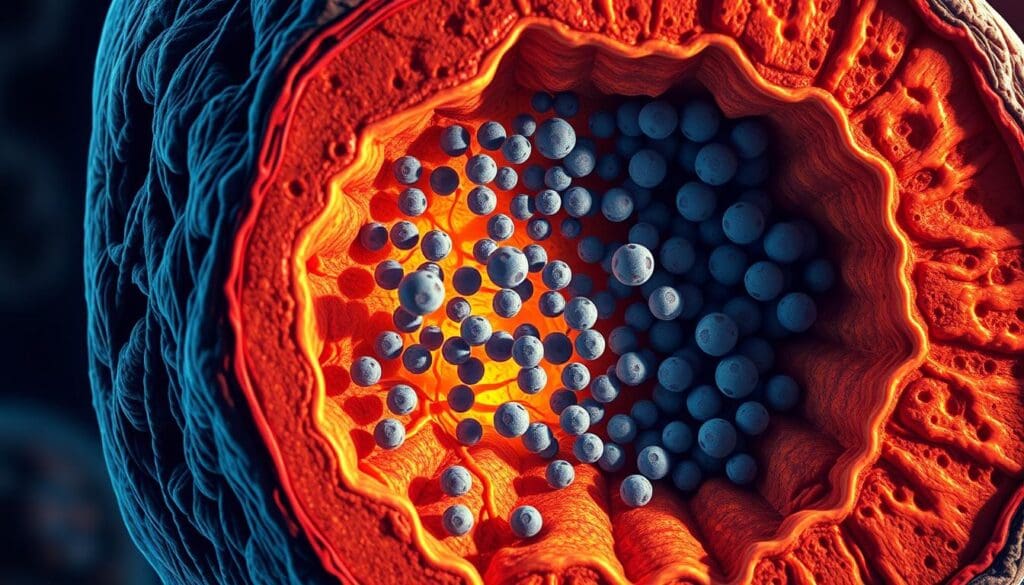
In 2025, understanding Acute Myeloid Leukemia (AML) is key for both patients and doctors. AML is a blood cancer where abnormal white blood cells grow fast. They stop normal blood cells from being made.
What is Acute Myeloid Leukemia?
AML is a fast-growing cancer that starts in the bone marrow and spreads to the blood. It can also go to other parts like the lymph nodes, liver, spleen, and even the brain. This cancer messes up blood cell making, causing anemia, infections, and bleeding.
Current Prevalence and Statistics
AML is not very common but is the top leukemia in adults. It’s more common in older adults. For the latest on AML research, check out Blood Cancer United.
Why Traditional Treatments Are Being Replaced
Old treatments like intensive chemotherapy have been used for years. But, new, targeted therapies are now preferred because they work better and are safer. This change to precision medicine is making AML treatment better and more tailored to each patient.
AML treatment is changing fast, thanks to new research and targeted therapies. This progress is making treatments more effective and helping manage this complex disease better.
The Evolution of AML Leukemia Treatments: From Chemotherapy to Precision Medicine
AML leukemia treatments have changed a lot. They moved from old chemotherapy to new, precise methods. This change shows we now understand the disease better and need better treatments.
Today, we’re moving away from the old “one treatment fits all” idea. Now, we’re using treatments that match each patient’s disease better.
Historical Treatment Approaches
In the past, AML treatment mostly used strong chemotherapy. These treatments were tough on the body but didn’t work for everyone.
The Genomic Revolution in AML Care
Genomics has changed AML care a lot. It lets us find the exact genetic problems in the disease. This has led to new, targeted treatments that work better.
How Treatment Selection Has Changed
Choosing treatments for AML patients is now more complex. We consider many things to find the best therapy for each patient.
Risk Stratification Approaches
- Genetic profiling to identify high-risk mutations
- Assessment of patient-specific factors, such as age and comorbidities
- Evaluation of response to initial therapy
Minimal Residual Disease Monitoring
Checking for minimal residual disease (MRD) is key in AML care. It helps catch relapse early and treat it quickly.
With these new tools, we can give aml therapies that really fit each acute myeloid leukemia patient.
Treatment #1: Venetoclax Combination Therapies
Venetoclax, when paired with hypomethylating agents or low-dose cytarabine, has shown better results in AML patients. This combo therapy is a big hope for those who didn’t do well with usual treatments.
How BCL-2 Inhibition Transforms AML Treatment
BCL-2 inhibition with venetoclax changes how we treat AML. It targets the BCL-2 protein, helping cancer cells die naturally. This method is very effective against AML, as it stops cancer cells from avoiding death.
Venetoclax with Hypomethylating Agents
Studies show that venetoclax and hypomethylating agents work great together. Hypomethylating agents turn on genes cancer silences, and venetoclax makes sure these cells die. This combo has led to better survival rates and more complete remissions for AML patients.
Venetoclax with Low-Dose Cytarabine
Venetoclax also pairs well with low-dose cytarabine. Low-dose cytarabine stops cancer cells from growing by messing with their DNA. Together, they’ve shown better results, even for older or sicker patients.
Patient Selection Criteria
Choosing the right patients for these treatments is key. Age, genetic makeup, and health are important. For example, those with IDH1 or IDH2 mutations might get more benefits.
- Age and overall health status
- Presence of specific genetic mutations
- Previous treatment history
Managing Side Effects and Toxicities
Even with promising results, managing side effects is vital. Common issues include low blood counts and stomach problems. Regular checks and supportive care help manage these and ensure the best results.
Key strategies for managing side effects include:
- Regular blood count monitoring
- Prophylactic antibiotics and antifungals
- Dose adjustments as necessary
Treatment #2: FLT3 Inhibitors – Quizartinib and Beyond
The creation of FLT3 inhibitors, like quizartinib, is a big step forward in AML treatment. FLT3 mutations are common in AML patients and often mean a worse prognosis. Targeting these mutations is a key strategy in treating AML.
The Critical Role of FLT3 Mutations in AML
FLT3 mutations are found in about 30% of AML patients. These mutations activate the FLT3 tyrosine kinase, helping leukemic cells grow and survive. FLT3 inhibitors aim to block this pathway, providing a more precise treatment.
Quizartinib: Mechanism and Clinical Outcomes
Quizartinib is a strong and selective FLT3 inhibitor that works well in AML patients with FLT3-ITD mutations. It stops FLT3 tyrosine kinase activity, causing leukemic cells to die. Studies show quizartinib can lead to remissions and better survival rates.
Comparing First and Second-Generation FLT3 Inhibitors
First-generation FLT3 inhibitors, like midostaurin, have been effective in AML treatment. Second-generation inhibitors, including quizartinib and gilteritinib, are more potent and specific. Comparative studies are underway to see which is better.
Resistance Patterns and Management Strategies
Resistance to FLT3 inhibitors can happen through secondary mutations in the FLT3 gene. To fight resistance, doctors use combination therapies and are working on new FLT3 inhibitors.
Combination Approaches with Chemotherapy
Using FLT3 inhibitors with chemotherapy seems to improve treatment results. Researchers are working to find the best ways to combine these treatments to help patients more.
Treatment #3: KMT2A-Targeted Therapies Including Ziftomenib
KMT2A-targeted therapies, like ziftomenib, are changing AML treatment. About 5-10% of AML patients have KMT2A rearrangements. These rearrangements create proteins that make the disease worse.
KMT2A Rearrangements and Their Significance
KMT2A rearrangements make fusion proteins that mess with gene expression. This is key to understanding how to target treatments.
Ziftomenib: Mechanism of Action and Trial Results
Ziftomenib works by blocking the menin-KMT2A bond. This action lowers the genes that cause leukemia. Early trials show it works well for patients with KMT2A rearrangements.
Patient Response Rates and Durability
Studies show ziftomenib helps many patients, with some staying in remission long-term. More research is needed to understand long-term effects.
Biomarkers for Treatment Selection
Finding biomarkers is key to picking the right patients for KMT2A therapies. Researchers are working hard to find good biomarkers for treatment choices.
Managing Treatment-Related Complications
It’s important to handle side effects of targeted therapies. Watching for problems and using supportive care can help patients do better.
The introduction of KMT2A-targeted therapies like ziftomenib is a big step forward in AML treatment. As research continues, we hope to see better results and more tailored treatments for patients.
Treatment #4: All-Oral Regimens – Decitabine-Cedazuridine with Venetoclax
All-oral regimens, like decitabine-cedazuridine with venetoclax, are changing AML care. They offer a simpler and less painful way to treat patients.
The Convenience Revolution in AML Care
The move to all-oral regimens is a big step forward in AML care. Patients can now get effective treatment without needing to go to the hospital often. This makes their lives better.
Pharmacology and Drug Interactions
Decitabine-cedazuridine with venetoclax combines two powerful treatments. It’s important to understand how it works and its possible side effects. This helps make treatment better.
Efficacy in Elderly and Comorbid Patients
Studies show this treatment works well for older and sicker patients. It’s a good option for those who can’t handle harsh chemotherapy.
Home-Based Administration Protocols
Decitabine-cedazuridine with venetoclax can be given at home. But, it needs careful planning and teaching the patient to use it safely and right.
Quality of Life Improvements
These treatments let patients stay at home, which improves their quality of life. They don’t have to go to the hospital as much.
As AML treatment keeps getting better, all-oral regimens will play a bigger role. They will give patients more options and better results.
Treatment #5: CAR-T Cell Therapy Breakthroughs for AML
CAR-T cell therapy is a new hope for AML patients. It changes a patient’s T-cells to fight cancer cells. This method is promising for those with hard-to-treat AML.
Engineering T-Cells to Target Myeloid Malignancies
CAR-T cell therapy is designed to attack AML cells. CD33 and CD123 are key targets in clinical trials. This therapy can kill AML cells by guiding T-cells to these antigens.
CD33 and CD123 as Primary Targets
CD33 and CD123 are found on AML cells, making them perfect targets. Targeting these has shown great promise in reducing AML cells. Ongoing trials are checking how well and safely CAR-T therapies work.
Managing Unique CAR-T Toxicities in AML
CAR-T cell therapy has benefits but also risks, like cytokine release syndrome (CRS). CRS management is key for patient safety. Doctors use corticosteroids and anti-IL-6 antibodies to lessen CRS.
Cytokine Release Syndrome Prevention
Preventing CRS means watching patients closely and acting fast. Quick treatment for CRS can greatly help patients.
Bridging to Stem Cell Transplantation
CAR-T cell therapy can lead to stem cell transplant, a possible cure. Combining CAR-T with stem cell transplant is being tested to improve survival chances.
As CAR-T cell therapy advances, we expect more AML treatment breakthroughs. Ongoing research and trials will shape AML treatment’s future.
Treatment #6: CRISPR-Based Therapeutic Approaches
CRISPR technology is changing how we treat AML by fixing the disease’s genetic roots. It’s a new way to fight AML by focusing on the genes that cause it to grow.
Gene Editing Fundamentals in AML Treatment
CRISPR-Cas9 is a game-changer in gene editing. It lets us make precise changes to our genes. In AML, it can fix the bad genes that start the disease. We’re looking into how it can turn off genes only in cancer cells, keeping healthy cells safe.
Ex-Vivo Modification of Hematopoietic Stem Cells
CRISPR is also being used to change stem cells outside the body. We take stem cells from the patient, edit them with CRISPR, and then put them back. Studies show it might work well and we’re testing it in clinical trials.
Targeting Leukemia-Specific Mutations
CRISPR can target AML’s unique mutations. By removing these mutations, we can stop the disease from getting worse. We’re finding the best targets and figuring out how to use CRISPR safely.
Safety Profiles and Off-Target Effects
It’s important to make sure CRISPR therapies are safe and don’t harm other parts of the body. We’re studying how to avoid these problems. We’re working on making CRISPR more precise and watching patients closely for any bad effects.
Regulatory Pathways and Accessibility
Getting CRISPR therapies to market is a big challenge. We’re working with regulators to make sure they’re safe and work well. We also want to make sure these treatments are available to many patients.
| CRISPR Application | Description | Potential Benefits |
|---|---|---|
| Ex-Vivo Modification | Editing hematopoietic stem cells outside the body | Reduced risk of off-target effects, possible cure |
| Targeting Leukemia Mutations | Disabling genes specific to AML | Slowing disease growth, better survival chances |
Treatment #7: Advanced Immunotherapy Combinations for AML
Advanced immunotherapy combinations are a new hope for Acute Myeloid Leukemia (AML) treatment. These treatments aim to boost the immune system’s fight against leukemia cells. This could bring new hope to patients.
Checkpoint Inhibitors in the AML Landscape
Checkpoint inhibitors are being studied to help the immune system fight AML cells better. Key checkpoint inhibitors include PD-1 and CTLA-4 inhibitors. They have shown promise in early trials.
Bispecific T-Cell Engagers and Novel Constructs
Bispecific T-cell engagers (BiTEs) are designed to connect T cells and AML cells. This helps T cells attack leukemia cells more effectively. Novel constructs like BiTEs are showing encouraging results in clinical trials.
Vaccine-Based Strategies for AML
Vaccine-based strategies aim to create an immune response against AML cells. These vaccines are being explored as a possible addition to other treatments.
Identifying Optimal Immunotherapy Candidates
Finding the right candidates for immunotherapy is key. Biomarkers and genetic profiling help predict who will benefit most from these treatments.
Combining Immunotherapy with Conventional Treatments
Researchers are looking into combining immunotherapy with traditional treatments.
Advanced immunotherapy combinations are a big step forward in AML treatment. They offer new chances to improve patient outcomes.
Personalized AML Leukemia Treatments: Matching Therapy to Patient Profiles
Our fight against AML is getting better with personalized treatments. Now, we can make treatments fit each patient’s needs, leading to better results.
Comprehensive Genomic and Proteomic Profiling
Genomic and proteomic profiling lead the way in AML treatment. We look at a patient’s genes and proteins to find disease drivers. This helps us pick the best treatments for each person.
Artificial Intelligence in Treatment Decision Support
Artificial intelligence (AI) is key in AML treatment choices. AI looks at lots of data, like genes and medical history, to suggest the best treatments.
Real-Time Response Assessment Technologies
We can now watch how treatments work in real time. Liquid biopsy applications are big, letting us check DNA in blood to see how well treatments are working and if resistance is coming.
Liquid Biopsy Applications
Liquid biopsies are a way to check on AML without invasive tests. They let us see how the disease is changing.
Predicting and Preventing Relapse
With new tech, we can spot and stop relapse early. Liquid biopsy helps find small disease leftovers, so we can act fast.
| Treatment Aspect | Traditional Approach | Personalized Approach |
|---|---|---|
| Genomic Analysis | Limited genetic testing | Comprehensive genomic profiling |
| Treatment Selection | One-size-fits-all | Tailored to patient profile |
| Response Monitoring | Periodic bone marrow biopsies | Real-time liquid biopsy |
The Future Landscape of AML Therapy: Beyond 2025
Looking ahead to 2025 and beyond, AML therapy is set for big changes. New treatments are being tested to help patients more.
Emerging Treatment Modalities in Development
New therapies are on the horizon, like novel targeted therapies and immunotherapies. These aim to tackle AML’s genetic and molecular roots.
Addressing Treatment Resistance Mechanisms
One big hurdle in AML treatment is resistance to current therapies. Scientists are diving into this issue to find ways to beat it.
The Ongoing Quest for an AML Cure
The dream of AML research is to find a cure. Stem cell treatments are being looked at as a possible cure.
Novel Combination Strategies
Using different treatments together is showing promise. For instance, mixing targeted therapies with immunotherapies could make treatments more effective.
Maintenance Therapy Approaches
Researchers are also exploring maintenance therapy to keep patients in remission longer. Here’s a look at some new maintenance therapy methods.
| Therapy | Description | Potential Benefits |
|---|---|---|
| Azacitidine | Hypomethylating agent | Prolongs remission, manageable toxicity |
| Lenalidomide | Immunomodulatory drug | Enhances immune response, oral administration |
| FLT3 inhibitors | Targeted therapy | Effective in FLT3-mutated AML, improves survival |
Conclusion: Navigating the New Era of AML Treatment
We’ve looked at the latest in AML treatment, changing how we care for patients. New methods like precision medicine, targeted therapies, and immunotherapy have changed how we treat AML.
Now, understanding the many treatments available is key. This includes Venetoclax, FLT3 inhibitors, and CAR-T cell therapy. These new options bring hope, better outcomes, and a better quality of life for patients.
Looking ahead, we’ll see more use of genetic testing, AI, and real-time monitoring. This will make treatments even more personal. We’re entering a time where treatments fit each patient’s needs better, making them more effective and safer.
The future of AML treatment looks bright, with more research and development underway. This work aims to overcome treatment resistance and find a cure. By keeping up with the latest in AML treatment, patients and doctors can work together to make the most of this new era of care.
What is Acute Myeloid Leukemia (AML)?
Acute Myeloid Leukemia (AML) is a cancer that starts in the bone marrow. It quickly moves into the blood. It can also spread to other parts of the body like the lymph nodes, liver, spleen, and more.
What are the latest advances in AML leukemia treatments?
New treatments for AML include personalized options and venetoclax combinations. There are also FLT3 inhibitors and KMT2A-targeted therapies. Other advances include all-oral regimens, CAR-T cell therapy, and CRISPR-based approaches.
How does venetoclax work in treating AML?
Venetoclax targets the BCL-2 protein in cancer cells. This helps kill AML cells. It’s a key treatment for AML.
What is the role of FLT3 mutations in AML?
FLT3 mutations occur in some AML patients. They lead to abnormal FLT3 protein. FLT3 inhibitors, like quizartinib, target these mutations to improve treatment.
What are KMT2A rearrangements, and how are they targeted in AML treatment?
KMT2A rearrangements are genetic changes in AML. Ziftomenib targets these changes. It works by blocking the menin-KMT2A interaction, essential for leukemia cell survival.
What are the benefits of all-oral regimens in AML treatment?
All-oral regimens, like decitabine-cedazuridine with venetoclax, are convenient. They improve patient compliance and reduce hospital visits. They’re great for elderly and comorbid patients.
How does CAR-T cell therapy work in treating AML?
CAR-T cell therapy modifies T-cells to target AML cells. These modified T-cells are infused back into the patient. They can then kill AML cells.
What is the potentia of CRISPR-based therapies in AML treatment?
CRISPR-based therapies use gene editing to modify stem cells. They target leukemia-specific mutations. This approach could cure AML by eliminating the disease’s root cause.
How do advanced immunotherapy combinations work in AML treatment?
Advanced immunotherapy combines checkpoint inhibitors, T-cell engagers, and vaccines. These strategies enhance the immune system’s ability to fight AML cells.
What is the significance of personalized AML treatments?
Personalized treatments use genomic and proteomic profiling. They tailor treatment to individual patients. This approach improves outcomes and reduces relapse risk.
What is the future landscape of AML therapy beyond 2025?
Future AML therapy will include new treatments and combination strategies. Ongoing research aims to overcome treatment resistance and find a cure.
What is treatment for acute myelogenous leukemia?
AML treatment combines chemotherapy, targeted therapy, and sometimes bone marrow transplantation. Treatment choices depend on the patient’s health, age, and leukemia type.
What is the treatment of acute myeloid leukemia?
AML treatment involves chemotherapy, targeted therapy, and immunotherapy. The goal is to induce remission and prevent relapse.
What are AML therapies?
AML therapies include chemotherapy, targeted therapy, immunotherapy, and bone marrow transplantation. These treatments manage and treat acute myeloid leukemia.
References
- Acute Leuk: https://acuteleuk.org/highlights-from-eha-2025-updates-in-aml/
- CA: A Cancer Journal for Clinicians / Wiley Online Library: https://acsjournals.onlinelibrary.wiley.com/doi/full/10.3322/caac.21873
- Blood Cancer United: https://bloodcancerunited.org/news/fda-approves-new-targeted-treatment-acute-myeloid-leukemia