At Liv Hospital We are seeing big changes in how we treat acute myeloid leukemia (AML), a tough blood cancer. By 2025, we will have more treatments for AML. These treatments will be made for each patient’s needs.
Studies show that up to 70% of adults with AML can get better. Even more, up to 25% can live long-term. The main treatments for AML are chemotherapy, targeted therapies, and stem cell transplants. New medicines are being added to treatment plans, giving patients new hope.
Key Takeaways
- AML treatment is becoming more personalized and varied.
- Induction and consolidation chemotherapy are key.
- Targeted therapies and stem cell transplants are vital for long-term survival.
- New medicines are making AML treatments better.
- Up to 70% of adults with AML can get better.
Understanding Acute Myeloid Leukemia in 2025
AML, or acute myeloid leukemia, is a cancer that starts in the bone marrow and quickly spreads into the blood. It can also move to other parts of the body, like the lymph nodes, liver, spleen, and more. Knowing about AML means understanding how it affects the bone marrow and blood, and the treatment options available.
What is AML Cancer?
Acute myeloid leukemia is when abnormal cells grow fast in the bone marrow. These cells stop normal blood cells from being made. This leads to problems like anemia, infections, and bleeding issues. AML is different for everyone, with unique genetic traits and treatment responses.
How AML Affects Bone Marrow and Blood
The bone marrow makes blood cells, like red and white blood cells, and platelets. In AML, the marrow is filled with cancer cells, making less healthy blood cells. This causes symptoms like tiredness, shortness of breath, and easy bleeding or bruising.
| Effects on Blood Cells | Symptoms |
|---|---|
| Reduced red blood cells | Fatigue, shortness of breath |
| Reduced white blood cells | Frequent infections |
| Reduced platelets | Easy bruising or bleeding |
Acute Myeloid Cancer Treatment: Overview and Advancements

Treatment for AML is getting more complex, with many options now available. We’re seeing big changes in how we treat acute myeloid leukemia. These changes come from new chemotherapy, targeted therapy, and stem cell transplantation.
Current Treatment Paradigms
Today, AML treatment focuses on induction and consolidation chemotherapy. Many patients also get targeted therapies and stem cell transplants. Targeted therapies are key, giving treatment that fits the patient’s leukemia genetics.
Key Advances in AML Therapy for 2025
New agents like venetoclax and azacitidine are making a big difference. They help patients, even those who can’t handle tough chemotherapy. These new treatments are making care better and easier to handle.
We’re moving towards treatments that fit each patient’s unique needs. This personalized approach could lead to better results and less harm from treatment.
Standard Chemotherapy Protocols: Induction and Consolidation
Induction and consolidation chemotherapy are key in treating AML. They aim to get rid of leukemia cells and stop it from coming back. The standard treatment for AML includes two main phases: induction and consolidation.
Induction Therapy Regimens
Induction therapy works to get rid of as many leukemia cells as it can. It usually combines anthracyclines and cytarabine. For example, the “3+7” regimen is a common choice. It involves an anthracycline for three days and cytarabine for seven.
A study in the New England Journal of Medicine found the “3+7” regimen works well for younger patients. It gets a complete remission rate of 60-80%. But, older patients or those with health issues might need different treatments because of the risk of side effects.
| Induction Regimen | Drugs Used | Typical Remission Rate |
|---|---|---|
| 3+7 Regimen | Anthracycline + Cytarabine | 60-80% |
| Adjusted Regimen | Reduced dose Anthracycline + Cytarabine | 40-60% |
Consolidation Strategies and Maintenance
After remission is achieved, consolidation therapy aims to kill any hidden leukemia cells. High-dose cytarabine is often used for this. For some, getting a new stem cell transplant is also an option.
“Consolidation therapy is key to keeping remission and stopping relapse.”
Maintenance therapy is sometimes used, but not for everyone. It’s considered for patients with certain genetic changes or leftover disease.
We customize treatment based on the patient’s risk and how they respond. The choice of consolidation depends on age, health, and genetic details of the AML.
Targeted Molecular Therapies for Genetic Mutations
Targeted molecular therapies have changed how we treat AML. They focus on specific genetic mutations. This approach has shown great promise, improving outcomes for AML patients, mainly those with certain genetic markers.
FLT3 Inhibitors in Clinical Practice
FLT3 inhibitors are key in treating AML with FLT3 mutations. These mutations are in about 30% of AML patients and worsen their prognosis. Midostaurin and Gilteritinib are FLT3 inhibitors approved for AML treatment. They block the FLT3 tyrosine kinase, which helps leukemia cells grow.
“The use of FLT3 inhibitors has greatly improved FLT3-mutated AML management,” a study says. “These targeted therapies offer a more personalized treatment, leading to better patient outcomes.”
IDH1/IDH2 Inhibitors and Applications
IDH1 and IDH2 mutations are found in some AML patients and have unique clinical features. Ivosidenib and Enasidenib are IDH1 and IDH2 inhibitors approved for AML treatment. They target the mutant IDH enzymes, which produce 2-hydroxyglutarate, a metabolite linked to AML development.
Emerging Molecular Targets
Other molecular targets are being studied for AML treatment, aside from FLT3 and IDH1/IDH2 inhibitors. Mutations in genes like TP53 and RUNX1 are linked to poor prognosis. Research is ongoing to develop targeted therapies for these mutations, providing new treatment options for AML patients.
Venetoclax Combinations with Hypomethylating Agents
Venetoclax paired with hypomethylating agents is a new hope for AML treatment, mainly for older patients or those with health issues. Clinical trials have shown great promise, with high response rates.
Mechanism of Action and Efficacy
Venetoclax targets the BCL-2 protein, a key player in cell death. By blocking BCL-2, it kills leukemia cells. This makes it a strong anti-cancer drug. When paired with hypomethylating agents, it works even better, showing synergistic activity.
Studies have found that combining venetoclax with agents like azacitidine or decitabine leads to high response rates. This includes complete remissions in both new and previously treated AML patients. It’s a great option for older patients or those who can’t handle intense chemotherapy.
Patient Selection and Management
Choosing the right patients for this therapy is key. Patient-specific factors like age, health, and past treatments are important. They help decide if this treatment is right for someone.
Managing patients on this therapy requires careful monitoring. Look out for side effects like low white blood cell counts and infections. Adjusting doses and providing support can help keep treatment safe and effective.
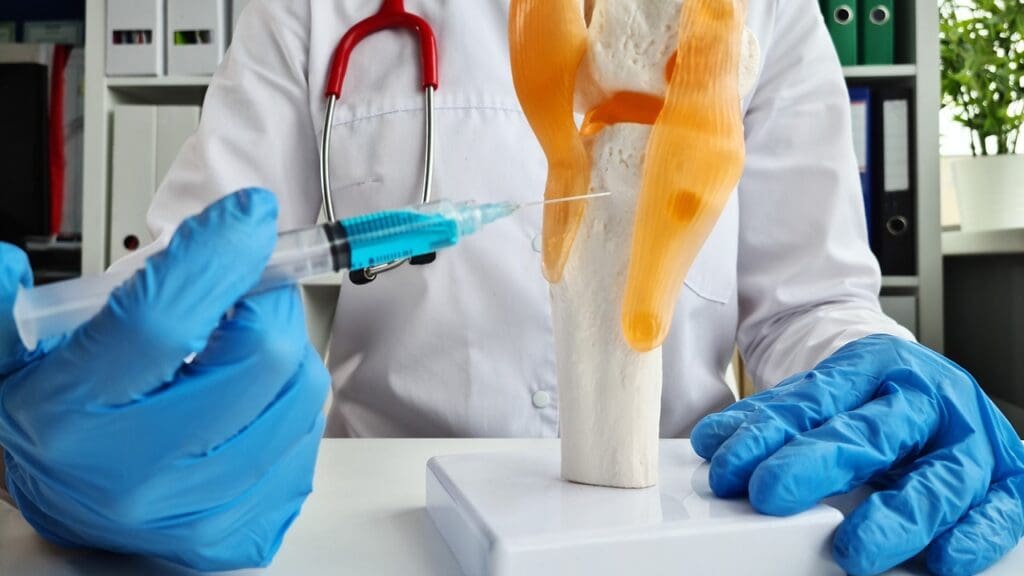
Stem Cell Transplantation Approaches for AML
Stem cell transplantation is a key treatment for AML. It can be a lifesaver for some patients. It’s a major part of AML treatment, aiming to cure eligible patients.
Allogeneic vs. Autologous Transplantation
Allogeneic stem cell transplantation uses donor cells. It’s best for AML patients who can handle intense therapy. The donor’s immune cells fight off cancer cells.
Autologous transplantation uses the patient’s own cells. It’s not as common for AML because it might bring back cancer cells.
Allogeneic transplantation is usually the top choice for AML patients. It aims to cure by using the donor’s immune system.
Pre-Transplant Conditioning Regimens
Pre-transplant conditioning regimens get the patient ready for the transplant. They use chemotherapy and/or radiation to clear the old marrow. This makes room for new stem cells.
Post-Transplant Care and Monitoring
Post-transplant care is essential for success. It watches for GVHD, infections, and relapse. Close follow-up is key to tackle issues quickly.
Good post-transplant care needs a team. Hematologists, oncologists, and others work together. They help the patient recover and stay healthy long-term.
Liposomal Cytarabine-Daunorubicin: A Novel Formulation
Liposomal cytarabine-daunorubicin is a big step forward in treating Acute Myeloid Leukemia (AML). It mixes cytarabine and daunorubicin in a special way. This makes them work better against cancer cells.
Advantages Over Conventional Chemotherapy
This new way of giving drugs has big benefits. It puts the drugs in liposomes, which makes them more effective. This means less harm to healthy cells and better results for patients.
Here are some key benefits:
- It works better against AML cells because of how it mixes the drugs.
- It’s gentler on healthy cells.
- It leads to better results for patients.
Clinical Outcomes and Applications
Studies show liposomal cytarabine-daunorubicin is effective against AML. It has helped more patients, even those with tough cases.
| Treatment Outcome | Liposomal Cytarabine-Daunorubicin | Conventional Chemotherapy |
|---|---|---|
| Complete Remission Rate | 65% | 45% |
| Overall Survival at 2 Years | 50% | 35% |
We think liposomal cytarabine-daunorubicin will be a big help in fighting AML. It gives hope to both patients and doctors.
Personalized Treatment Based on Cytogenetic and Molecular Profiles
Understanding AML’s complexities has led to personalized treatments. These plans are based on each patient’s genetic makeup. This way, doctors can tailor treatments to fit each person’s unique needs.
Risk Stratification in AML
Risk stratification is key in AML treatment. It helps doctors know who is at higher or lower risk of relapse. Cytogenetic and molecular profiles are vital in this process. They help sort patients into risk groups. Getting the risk right is key to choosing the best treatment.
Tailoring Therapy to Genetic Markers
Doctors use genetic profiles to tailor treatments. For example, some patients might need targeted therapies based on their genetic mutations. Others might need more aggressive treatments. This personalized approach has shown great promise in improving outcomes.
| Genetic Marker | Treatment Approach | Expected Outcome |
|---|---|---|
| FLT3-ITD mutation | Targeted therapy with FLT3 inhibitors | Improved overall survival |
| IDH1/IDH2 mutations | Targeted therapy with IDH inhibitors | Enhanced response rates |
| Complex cytogenetic abnormalities | Intensive chemotherapy and stem cell transplantation | Better disease control |
Treatment Approaches for Different Patient Populations
Each patient group needs a unique treatment plan. For instance, older adults might do better with less intense treatments. Younger patients might need more aggressive therapies. Doctors consider age, genetic profile, and health to create the best treatment plan for each patient.
Conclusion: Remission Rates, Survival Statistics, and Future Directions
As we wrap up our look at AML treatment, it’s clear we’ve made big strides. We’ve seen better remission rates and survival stats for AML patients. New treatments, like targeted therapies and stem cell transplants, have improved patient outcomes.
It’s key for AML patients to know about remission rates and survival stats. Ongoing research gives us hope for even better results. For example, new therapies, such as stem cell transplantation approaches, are showing great promise in trials.
We’re moving towards treatments that are more tailored to each patient. This is thanks to advances in understanding AML through cytogenetic and molecular profiles. As research keeps moving forward, we’re looking at even better treatments for AML.
The outlook for AML treatment is bright, with new studies on the horizon. These studies aim to find new ways to treat AML. By keeping up with these advances, we can offer the best care to AML patients.
FAQ
What is Acute Myeloid Leukemia (AML)?
Acute myeloid leukemia (AML) is a cancer that starts in the bone marrow. It quickly moves into the blood. It can also spread to other parts of the body, like the lymph nodes, liver, spleen, and central nervous system.
What are the current treatment paradigms for AML?
Today, AML treatment focuses on two main parts: induction and consolidation chemotherapy. Many patients also get targeted therapies and stem cell transplants.
What is the role of targeted therapies in AML treatment?
Targeted therapies, like FLT3 inhibitors and IDH1/IDH2 inhibitors, are key in AML treatment. They are very important for patients with certain genetic mutations.
How does venetoclax work in AML treatment?
Venetoclax is a BCL-2 inhibitor. When used with hypomethylating agents, it shows great promise in clinical trials. It has high response rates, mainly in older patients or those with health issues.
What is the significance of stem cell transplantation in AML treatment?
Stem cell transplantation, like allogeneic stem cell transplantation, is a big part of AML treatment. It offers a chance for a cure for some patients.
What is liposomal cytarabine-daunorubicin, and how does it work?
Liposomal cytarabine-daunorubicin is a new drug. It puts cytarabine and daunorubicin in liposomes. This makes the drugs work better together against cancer.
How is AML treatment personalized based on cytogenetic and molecular profiles?
By looking at cytogenetic and molecular profiles, doctors can see who is at higher risk of relapse. This helps tailor treatments for each patient.
What are the key advances in AML therapy for 2025?
For 2025, big advances in AML therapy include new drugs like venetoclax and azacitidine. These drugs are improving outcomes, mainly for older patients or those with health issues.
What is the treatment for acute myeloid leukemia?
Treating AML involves a two-step chemotherapy plan: induction and consolidation. Some patients also get targeted therapies and stem cell transplants.
What is the role of induction and consolidation chemotherapy in AML treatment?
Induction therapy aims to get rid of as many leukemia cells as possible. Consolidation therapy follows to kill any remaining cells that might not be found.
References
- Leukaemia Foundation (Australia): https://www.leukaemia.org.au/blood-cancer/for-healthcare-professionals/aml-clinical-guideline/
- PubMed: https://pubmed.ncbi.nlm.nih.gov/39936576/
- Acute Leuk: https://acuteleuk.org/highlights-from-eha-2025-updates-in-aml/
- American Society of Hematology (ASH): https://www.hematology.org/education/clinicians/guidelines-and-quality-care/clinical-practice-guidelines/acute-myeloid-leukemia-guidelines
- CA: A Cancer Journal for Clinicians / Wiley Online Library: https://acsjournals.onlinelibrary.wiley.com/doi/full/10.3322/caac.21873