Last Updated on December 3, 2025 by Bilal Hasdemir

Robotic heart surgery has changed cardiac surgery a lot. It makes procedures less invasive, which means less recovery time and less scarring. But, like any new tech, it has its own set of problems. Studies show that about 10% of these surgeries lead to big complications, making us question the safety of this tech.
Looking into robotic heart surgery shows both its good sides and its downsides. It has helped many patients, but it’s not without risks. We’ll dive into the possible downsides, like risks associated with robotic heart surgery, to give you a full picture of this complex area.
Key Takeaways
- Robotic heart surgery offers minimally invasive procedures.
- Significant complications occur in nearly 10% of cases.
- Understanding the risks is key for patient safety.
- Robotic heart surgery isn’t right for everyone.
- The tech keeps getting better, leading to better results.
The Evolution of Robotic Systems in Cardiac Surgery
Cardiac surgery has changed a lot with robotic systems. These systems help surgeons do complex surgeries with more precision and less invasion. This has greatly improved patient results.
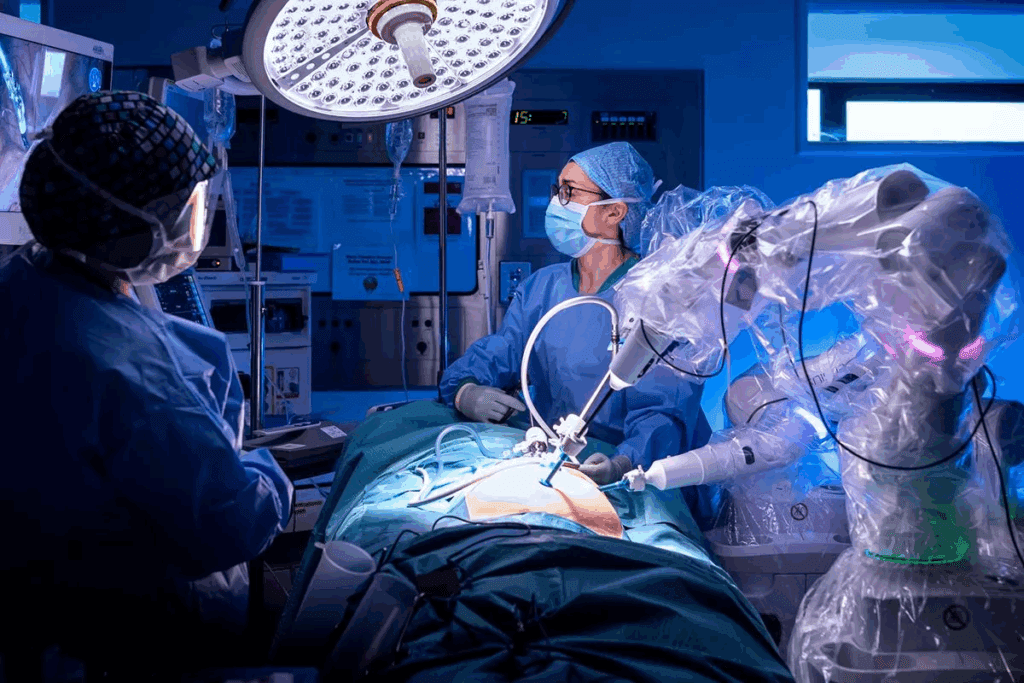
Current Technology and Applications
Robotic systems in cardiac surgery have grown a lot. Today’s tech gives surgeons advanced tools. These tools offer clear 3D views, precise instruments, and better control.
These systems are used for many surgeries, like fixing heart valves and closing holes in the heart. They make surgeries less invasive, leading to smaller cuts, less pain, and quicker healing.
Comparing Robotic Systems with Traditional Approaches
Robotic systems and traditional surgery differ in many ways. Robotic systems are great for minimally invasive surgery. They often mean less pain and faster healing.
But, traditional surgery is sometimes better for very complex cases. The choice between robotic and traditional surgery depends on the patient’s health, the surgery needed, and the surgeon’s skills.
As we keep improving in cardiac surgery, robotic systems will likely play an even bigger role. Understanding both robotic and traditional surgery helps us choose the best treatment for each patient.
Technical Limitations of Robotic Heart Surgery
Robotic heart surgery faces big challenges like mechanical issues and system failures. Even with the latest tech, these problems can affect how well and safely the surgery is done.
Mechanical Constraints and System Failures
Robotic systems in heart surgery are complex and can fail. Mechanical constraints mean the design of the robotic tools limits their movement. This can make it hard to work in tight spaces during surgery.
System failures are serious issues that can happen due to tech problems. These failures can be small or big, and some need to switch to open surgery. The risk of system failure shows why keeping the systems in top shape is key.
Lack of Tactile Feedback and Spatial Awareness
Robotic heart surgery also lacks tactile feedback. Unlike open surgery, where surgeons feel tissues, robotic surgery relies on what they see. This makes it hard to feel the heart’s delicate parts.
Also, spatial awareness is key in robotic heart surgery. It’s about knowing where the robotic arms and tools are in the chest. Without feeling, it’s harder to know where everything is, which can lead to injuries.
To deal with these issues, surgeons get a lot of training. They learn to use their eyes and hands better. They also use advanced tech to see and control the instruments more precisely.
Extended Operative Times and Anesthesia Exposure
Robotic heart surgery can take longer, which might pose risks. It’s key to look into how longer surgeries affect patient care.
Duration Analysis: Robotic vs. Conventional Approaches
Robotic heart surgery often takes more time than traditional surgery. For example, robotic coronary artery bypass grafting (CABG) takes longer than the traditional method.
| Surgical Approach | Average Operative Time (minutes) | Standard Deviation |
| Robotic CABG | 240 | ± 30 |
| Conventional CABG | 180 | ± 20 |
The table shows robotic CABG takes longer than traditional CABG. This is because setting up the robotic system and the need for precision add to the time.
Health Implications of Prolonged Anesthesia
Longer anesthesia times in robotic heart surgery can be risky. They may lead to postoperative cognitive dysfunction and respiratory complications.
It’s important to think about how long anesthesia affects patients. Risks include:
- Respiratory depression
- Cardiac complications
- Prolonged recovery times
Knowing these risks helps us improve patient care. By refining surgical and anesthesia methods, we can reduce risks from longer surgeries in robotic heart surgery.
The Steep Learning Curve for Cardiac Surgeons
Cardiac surgeons have a big challenge when they start using robotic heart surgery. They need to go through detailed training programs. The robotic systems are complex, so surgeons must be very skilled. This skill comes from dedicated training and lots of practice.
Training Requirements and Proficiency Milestones
To get better, cardiac surgeons must go through tough training. Training programs should be made for each surgeon’s level. There should be clear goals to check how well they’re doing.
The training includes:
- Learning about robotic systems
- Watching experienced surgeons work
- Practicing in a safe place
- Doing harder procedures with help
Surgeons need to get good at using the robotic system. They must also know how to handle problems and work well with the team. Good training is key to avoiding mistakes and better patient care.
Team Coordination and Communication Challenges
Robotic heart surgery needs a team that works together well. This includes the surgeon, anesthesiologist, nurses, and technical staff. Good communication is important. It makes sure everyone knows their job and can solve problems fast.
Hospitals can help with team work and talking by:
- Having team training to build trust and teamwork
- Using clear communication rules to avoid mistakes
- Talking about what went right or wrong after surgery
By focusing on training and teamwork, we can make robotic heart surgery better. This will lead to better care for patients.
Financial Burden: Cost Analysis of Robotic Heart Surgery
Robotic heart surgery is growing, and knowing its cost is key for everyone. It affects both healthcare systems and patients. We need to look at several important factors.
Initial Investment and Maintenance Expenses
The cost to start robotic heart surgery is high. It includes buying the equipment and training the team. Maintenance expenses are also big, as these systems need updates and support. These costs are part of the total financial burden.
Patient Financial Impact and Insurance Coverage Issues
Patients face big costs with robotic heart surgery. This includes the surgery, hospital stay, and care after. Insurance coverage helps, but it’s not the same for everyone. This can lead to financial problems for many.
Looking closely at the costs of robotic heart surgery shows several areas of expense. These are:
- The cost of the robotic system and its maintenance
- Training and education for surgical staff
- Procedure-related costs, including hospital stay and supplies
- Follow-up care and possible complications
It’s vital to understand the financial side of robotic heart surgery. By looking at the initial costs, maintenance, and how it affects patients, we can make better choices. This helps us deal with the economic challenges of this surgery.
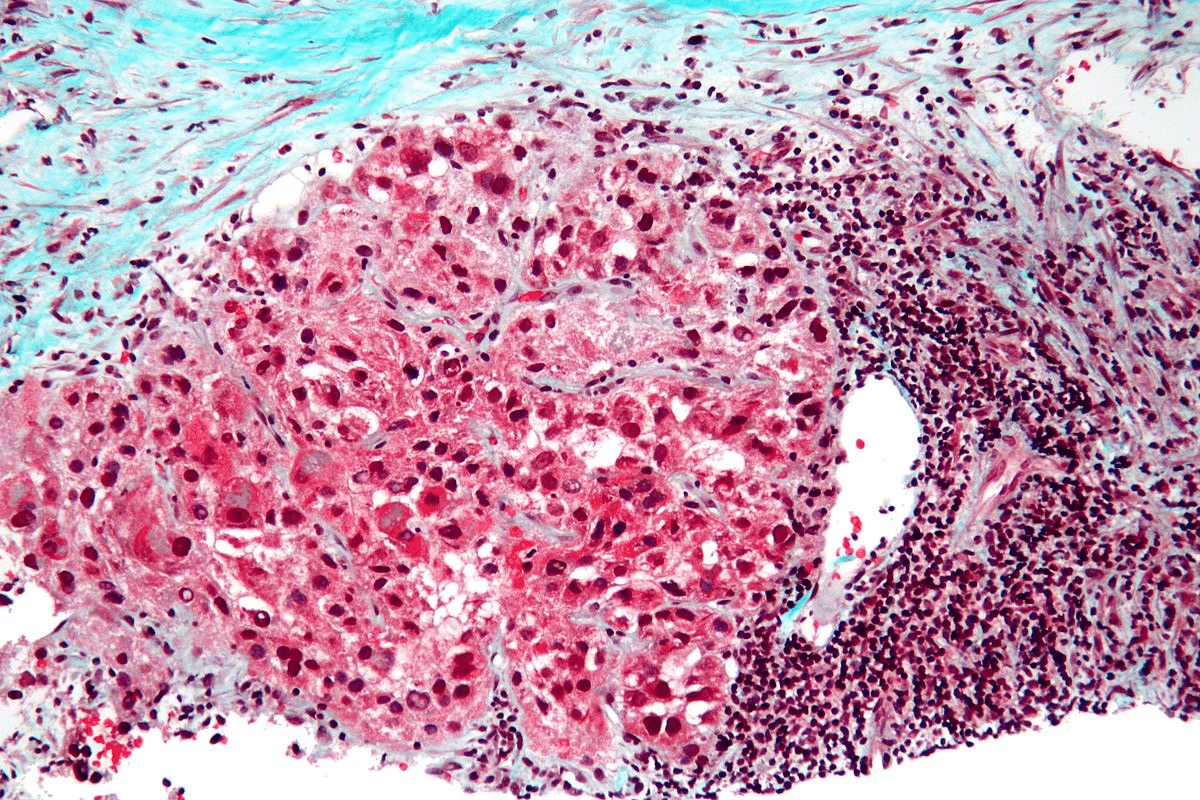
Complication of Cardiac Surgery: Specific Risks in Robotic Procedures
Robotic cardiac surgery has made big strides, but it’s not without risks. These include intraoperative complications and technical failures. It’s key to know about these risks and how to lessen them.
Intraoperative Complications Unique to Robotic Approaches
Robotic heart surgery comes with unique risks. These include vascular injuries from robotic port insertion, bleeding at the surgical site, and conversion to open surgery in emergencies.
- Vascular injuries: The risk of damaging major blood vessels during the insertion of robotic ports or during the surgery itself.
- Bleeding: Managing bleeding can be challenging due to the limited dexterity of robotic instruments.
- Conversion to open surgery: The need to immediately convert to an open surgical procedure in case of severe complications.
Technical Failures and Their Consequences
Technical failures in robotic heart surgery can have big consequences. These can include instrument malfunction and systemic software or hardware failures. It’s vital to understand these risks to develop effective backup plans and emergency protocols.
| Type of Technical Failure | Consequence | Mitigation Strategy |
| Instrument Malfunction | Interruption of surgery, possible injury | Regular maintenance, having backup instruments |
| Systemic Software Failure | Loss of control over robotic system | Robust software testing, having a manual override |
| Hardware Failure | System shutdown, possible injury | Regular hardware checks, redundancy in critical systems |
By grasping the risks of robotic cardiac surgery, we can better prepare and manage them. This helps improve patient outcomes.
Patient Selection Limitations for Robotic Heart Surgery
Choosing the right patients for robotic heart surgery is key. We look at their body shape and health before surgery. This helps us get the best results for them.
Anatomical Considerations and Contraindications
Some body shapes make robotic heart surgery harder or not possible. For example, severe aorta calcification or many past surgeries can make it tough. These cases are more complex.
Here’s a table showing important body shapes and their impact on surgery:
| Anatomical Consideration | Implication for Robotic Heart Surgery |
| Severe aortic calcification | Increased risk of stroke or aortic dissection |
| Previous multiple cardiac surgeries | Adhesions may complicate robotic access |
| Small or fragile vascular structures | Higher risk of vascular injury |
Pre-existing Conditions That Increase Risk
Health problems before surgery also matter. Issues like severe COPD, kidney problems, or uncontrolled diabetes raise surgery risks. These can lead to complications during and after the operation.
We check each patient’s health to see if they’re right for robotic surgery. This careful look helps us spot risks and plan how to avoid them.
Below is a table showing common health issues and their effects on surgery:
| Pre-existing Condition | Potential Impact on Robotic Heart Surgery |
| Severe COPD | Increased risk of respiratory complications |
| Significant renal impairment | Potential for acute kidney injury post-surgery |
| Uncontrolled diabetes | Higher risk of wound infection and delayed healing |
By thinking about body shape and health, we pick patients who will likely do well with robotic surgery. This way, we reduce risks for them.
Conversion Rates to Open Procedures: Causes and Consequences
It’s important to know why some robotic heart surgeries turn into open procedures. This change can affect patient care. Several factors can lead to this switch.
Common Reasons for Emergency Conversion
Emergency conversion in robotic heart surgery can happen for a few reasons. These include uncontrolled bleeding, equipment failure, and anatomical complexities that are hard to manage with robots.
Uncontrolled bleeding is a big reason for emergency conversion. It needs quick action to avoid serious problems. Equipment failure, though rare, is also a major cause. It shows the importance of good maintenance and backup systems.
Impact on Patient Outcomes and Recovery
Switching to open procedures can affect patient outcomes and recovery. Patients who need emergency conversion might stay in the hospital longer. They also face a higher risk of complications and a tougher recovery.
Research shows robotic heart surgery is less invasive and leads to quicker recovery. But, if it turns into open surgery, these benefits can be lost. So, understanding why this happens is key to better patient care and outcomes.
By looking into why some surgeries switch to open procedures, we can get ready for problems. This helps improve the quality of care for patients having robotic heart surgery.
Cardiac Surgery Mortality Rates: Robotic vs. Traditional Approaches
Looking at the death rates of robotic versus traditional heart surgery helps us see how well they work. We need to look at both short-term and long-term results to really understand.
Short-term Mortality Comparisons
Short-term death rates show how risky a surgery is right after it’s done. Research shows that both types of surgery have similar death rates within 30 days. But, robotic surgery might have a slight edge because it’s less invasive. This could mean fewer complications.
Key findings include:
- Robotic heart surgery often has fewer complications right after surgery.
- The robotic system’s precision can make recovery more stable.
- Some studies show robotic surgery might lower short-term death rates, but not for everyone.
Long-term Survival Analysis
Long-term survival studies tell us how well the surgery lasts over time. Research shows both types of surgery can lead to great long-term survival rates. Some studies say the long-term results are about the same for both.
Important things for long-term survival include:
- Robotic surgery might lower the risk of long-term problems like infections and hernias.
- Less trauma and stress from robotic surgery could help with long-term recovery and survival.
- Keeping an eye on heart health after surgery is key, no matter the surgery type.
In summary, both robotic and traditional heart surgery have their good points. Knowing the details of their death rates is key for making smart choices. As technology gets better, we can expect even better results for patients.
Postoperative Complications After Robotic Heart Surgery
It’s important to know about the complications after robotic heart surgery. This surgery has many benefits but also some challenges. Healthcare providers must address these to help patients recover well.
Wound Healing and Infection Rates
Robotic heart surgery uses smaller incisions, which can lead to less tissue damage and lower infection rates. But, the situation is more complex. Wound healing complications can happen, and things like diabetes, smoking, and the surgeon’s skill matter a lot.
Even though infections are less common than in open-heart surgery, they can occur. meticulous wound care and watching patients closely after surgery are key to avoiding these problems.
Cardiac-Specific Complications
Complications specific to the heart after robotic surgery are a big worry. These include arrhythmias, cardiac tamponade, and problems with the repair, like shunts or valve issues. The surgery’s complexity and the patient’s heart health before surgery affect these risks.
To lower these risks, thorough preoperative evaluation and intraoperative monitoring are essential. A skilled team experienced in robotic heart surgery is also important for handling any issues that come up.
After surgery, it’s important to watch for signs of heart problems. Having plans in place for quick action if needed is important. By understanding and preparing for these heart-related complications, doctors can improve patient care and reduce risks.
Cardiac Surgery Risk Factors Amplified by Robotic Approaches
Robotic technology in cardiac surgery brings new risks. It’s vital to understand and manage these risks. This ensures the best results for our patients.
Patient-Specific Risk Factors
Patient-specific risks are key in robotic cardiac surgery. These include:
- Pre-existing Conditions: Patients with heart issues, like coronary artery disease, face higher risks.
- Age and Frailty: Older or frail patients may struggle more with recovery and surgery stress.
- Anatomical Considerations: Different heart shapes can make surgery harder, needing special techniques.
Procedure-Specific Risk Factors
Procedure-specific risks are also important. These include:
- Technical Failures: Risks of robotic system problems during surgery.
- Prolonged Operative Times: Longer surgeries increase risks, like anesthesia problems.
- Learning Curve: The complex nature of robotic surgery requires a lot of practice, affecting results at first.
It’s essential to understand these risks to improve outcomes. By focusing on patient and procedure risks, we can tackle the challenges of robotic cardiac surgery. This helps us achieve better results for our patients.
Institutional Challenges in Implementing Robotic Cardiac Programs
Starting a robotic cardiac surgery program faces many hurdles. We need to invest in infrastructure, training, and technology.
Infrastructure and Resource Requirements
Setting up a robotic cardiac program needs a lot of resources. This includes top-notch equipment and special facilities. Robotic systems need rooms with space for the console, patient cart, and vision system.
Training the surgical team is also key. This includes surgeons, anesthesiologists, and nurses. They must learn how to use the robotic technology safely and effectively.
| Infrastructure Component | Description | Importance Level |
| Robotic System | The robotic surgery equipment | High |
| Dedicated Operating Room | Specially designed OR for robotic surgery | High |
| Training Programs | Comprehensive training for surgical staff | High |
Volume-Outcome Relationship in Robotic Cardiac Surgery
The success of robotic cardiac surgery programs depends on the number of procedures done. Higher volume centers usually have better results because their teams have more experience.
It’s important to think about the volume-outcome relationship when starting and keeping robotic cardiac programs. Having enough cases is key to staying skilled.
Understanding the challenges and the role of volume in robotic cardiac surgery helps us support effective programs. This knowledge will help us improve patient care and move the field of cardiac surgery forward.
Managing Complications Following Robotic Heart Surgery
Managing complications after robotic heart surgery is key to good patient results. This surgery uses new technology and small incisions to change heart care. But, like any surgery, it has its own challenges and possible problems.
Early Recognition Strategies
Spotting problems early is very important in robotic heart surgery. This means using advanced monitoring and knowing the possible issues that can happen during and after surgery.
- Intraoperative monitoring: Keeping an eye on vital signs and the surgery area helps find problems early.
- Postoperative care: Watching closely after surgery for signs of issues like bleeding, infection, or heart problems.
- Team coordination: Good communication among the surgical team, anesthesiologists, and nurses is key for quick action on problems.
Intervention Approaches and Treatment Protocols
When a problem is found, acting fast and effectively is needed. This means having clear plans for different possible problems.
- Emergency preparedness: Being ready for emergencies like heart stop or big bleeding.
- Specific treatment protocols: Having special plans for issues like irregular heartbeat, stroke, or kidney failure.
- Multidisciplinary care: Working together with different specialists to handle problems well.
Rehabilitation Considerations
Rehab is very important for patients after robotic heart surgery, even more so if problems come up. A good rehab plan can really help patients get better.
- Personalized rehabilitation plans: Making rehab plans that fit each patient’s needs, considering any problems they have.
- Physical therapy: Starting to move and do physical therapy early to avoid problems like blood clots and to help the heart.
- Patient education: Teaching patients how to take care of themselves and watch for signs of problems while they recover.
By focusing on spotting problems early, acting quickly, and having a good rehab plan, healthcare teams can handle complications after robotic heart surgery. This helps patients get the best results possible.
Cardiac Surgery Complications Prevention in Robotic Procedures
Preventing complications in robotic heart surgery is key for the best results. As we move forward, it’s vital to know how to lower risks. This is important for both doctors and patients.
Preoperative Risk Assessment and Optimization
Checking patients before surgery is a big step in avoiding problems. We look at their medical history, current health, and risk factors. This helps us see who might need extra care before surgery.
Key factors assessed preoperatively include:
- Cardiac function and overall cardiovascular health
- Presence of comorbidities such as diabetes or hypertension
- Previous surgical history and possible adhesions
- Patient’s overall physical condition and frailty
By focusing on these areas, we can make patients better prepared for surgery. This might lower the chance of complications.
Intraoperative Strategies to Minimize Complications
During robotic heart surgery, we use several strategies to avoid problems. We use advanced imaging and real-time monitoring to guide the team.
| Intraoperative Strategy | Description | Benefit |
| Advanced Imaging | Utilization of high-definition 3D visualization | Enhanced precision and reduced risk of injury to surrounding structures |
| Real-time Monitoring | Continuous monitoring of vital signs and surgical site | Early detection of possible complications |
| Team Coordination | Effective communication among surgical team members | Reduced risk of human error |
These methods, along with robotic precision, help reduce surgery risks.
Postoperative Monitoring and Early Intervention
After surgery, care is just as important. We have a detailed monitoring plan to catch and fix any issues quickly.
Key aspects of postoperative care include:
- Close monitoring of vital signs and cardiac function
- Effective pain management to promote recovery
- Early mobilization to prevent complications such as deep vein thrombosis
- Continuous assessment for signs of possible complications
By staying alert after surgery, we can act fast if problems come up. This helps improve patient results.
Conclusion: Weighing the Risks and Benefits of Robotic Heart Surgery
Robotic heart surgery has changed cardiac surgery a lot. It can lead to quicker recovery times and less invasive procedures. But, it also has risks and complications like technical issues, longer surgery times, and high costs.
When looking at robotic heart surgery, we must consider both sides. It’s important to know the risks and benefits to make good choices. Doctors and patients need to think about the surgeon’s skill, the patient’s health, and what the surgery needs.
Understanding the challenges of robotic heart surgery helps us support patients and doctors better. As technology gets better, staying updated on robotic cardiac surgery is key.
FAQ
What are the main disadvantages of robotic heart surgery?
Robotic heart surgery has several downsides. It has technical limits, takes longer, and is expensive. Surgeons need a lot of training, and there are risks like system failures.
How does robotic heart surgery compare to traditional open-heart surgery in terms of risks?
Robotic heart surgery has its own risks, like system failures. But it also has benefits like smaller cuts and quicker healing. Each patient’s situation is different, so the risks and benefits must be weighed carefully.
What are the technical limitations of robotic heart surgery?
Robotic heart surgery faces technical challenges. These include system failures and a lack of touch and spatial awareness. These issues can make the surgery more complex and increase the risk of complications.
How do extended operative times affect patients undergoing robotic heart surgery?
Longer surgeries in robotic heart surgery mean more time under anesthesia. This can lead to more complications and a longer recovery.
What kind of training do cardiac surgeons need to perform robotic heart surgery?
Surgeons need special training for robotic heart surgery. They must learn to use the robotic system and handle complications. This training is essential for their skills.
How does the cost of robotic heart surgery compare to traditional heart surgery?
Robotic heart surgery is pricier than traditional surgery. The cost includes the robotic system, maintenance, and instruments. Insurance and financial impact on patients need to be considered.
What are the specific risks associated with robotic heart surgery?
Robotic heart surgery carries unique risks like system failures and the need for open surgery. Knowing these risks is important for patient care.
How are patients selected for robotic heart surgery?
Patients are chosen based on their anatomy and health. Not all patients are good candidates for robotic surgery.
What happens if a robotic heart surgery needs to be converted to an open procedure?
If a robotic surgery needs to be open, it can affect recovery. Understanding why this happens and being ready is key.
How do mortality rates compare between robotic and traditional heart surgery?
Mortality rates for robotic and traditional surgery are similar. But, they depend on patient selection and surgeon experience. Both short and long-term survival are important.
What postoperative complications can occur after robotic heart surgery?
After robotic heart surgery, patients might face wound issues, infections, and heart problems. Knowing these risks helps in providing the right care.
How can complications following robotic heart surgery be managed?
Managing complications involves early detection and treatment. A team approach is best for patient care.
What strategies can prevent complications in robotic heart surgery?
To prevent complications, assess risks before surgery and use strategies during surgery. Monitoring and early action are key to good outcomes.
References
- Chitwood, W. R., Nifong, L. W., & Chapman, W. H. (2007). Robotic mitral valve repair: experience with the da Vinci system in 300 patients. The Annals of Thoracic Surgery, 82(5), 1734-1741. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4247456/