Last Updated on November 24, 2025 by
Multiple Congenital Anomalies (MCAs) are when a baby is born with two or more major birth defects. These defects affect different parts of the body. They can’t be explained by just one syndrome or genetic disorder.
It’s estimated that 20-30% of kids with birth defects have MCAs. This makes their diagnosis and treatment very hard for healthcare teams.

We understand how complex MCAs are. They deeply affect the lives of those who have them and their families. Knowing about MCAs helps us give better care and support.Learn about multiple congenital anomalies, where a child is born with more than one birth defect. Understand diagnosis and care.
Multiple congenital anomalies (MCAs) are a complex condition that affects many infants worldwide. Studies show that about 2-3.7% of babies with birth defects have MCAs. This highlights the need to understand this condition well.
To diagnose MCAs, we look for two or more major congenital anomalies. The National Birth Defects Prevention Study (NBDPS) says MCAs are when a baby has two or more NBDPS-eligible birth defects. This rule helps us identify babies with MCAs clearly.
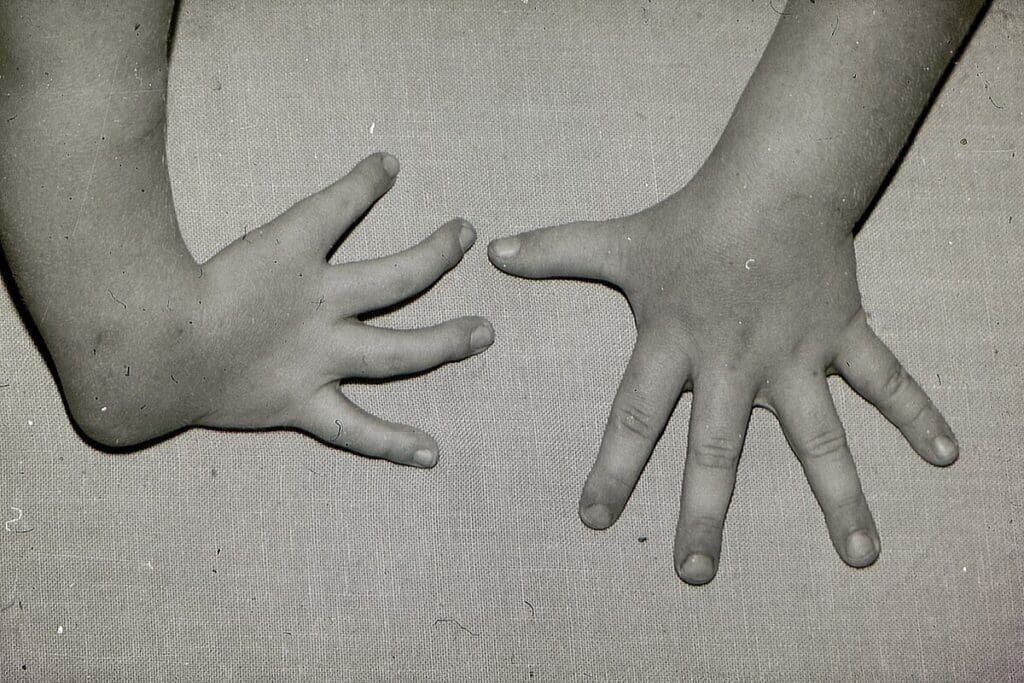
The NBDPS also says the anomalies must be different and not part of a single syndrome. For example, a child with both a heart defect and a limb anomaly has MCAs if these are not linked to a single condition.
It’s key to tell MCAs apart from single defects and syndromes. A single defect is an isolated anomaly, like a ventricular septal defect. On the other hand, a syndrome is a pattern of related anomalies with a common cause.
Experts say it can be hard to tell MCAs from syndromes because they sometimes overlap.
“Accurate diagnosis requires a thorough evaluation, including genetic testing and imaging studies, to find the underlying causes and related anomalies.”

Knowing the differences between MCAs, single defects, and syndromes is vital for proper care and support. We understand the challenges in diagnosing and managing MCAs. We’re dedicated to providing full care to those affected.
Congenital anomalies are common in births worldwide, with different rates in each area. It’s key to understand these issues to improve healthcare and support families.
Research shows congenital anomalies occur in 15.1 to 26.3 per 10,000 births globally. This range comes from different ways of collecting data and regional differences.
These anomalies are a big health issue worldwide. The data on congenital anomalies show we need more research and better ways to report these issues.
The EUROCAT study found that about 16 per 10,000 births have multiple congenital anomalies (MCAs). This highlights the role of registries in tracking congenital anomalies.
EUROCAT’s work has greatly helped us understand birth defect statistics in Europe. Their findings help plan better healthcare and use resources wisely.
There are big differences in congenital anomaly rates around the world. These differences come from genetics, environment, and socio-economic factors. Some areas have higher rates of certain anomalies due to these factors.
It’s important to understand these regional differences. By looking at congenital malformation data from different places, we can find areas with higher rates. Then, we can create specific strategies to help these areas.
It’s important to understand the different types of multiple congenital anomalies. These anomalies can appear in many ways. Some types are more common than others.
Cardiovascular defects are very common in cases of multiple congenital anomalies. The National Birth Defects Prevention Study (NBDPS) found that 63.1% of cases with MCAs had congenital heart defects. This shows how critical it is to check the heart thoroughly in patients with multiple anomalies.
Oral-facial anomalies, like oral clefts, are also common in MCAs. We see that 23% of cases involve oral clefts. This means it’s very important to check the mouth and face carefully.
Gastrointestinal malformations, like anorectal atresia/stenosis, are often seen with MCAs. The data show that 21% of cases involve anorectal anomalies. This means we need to check the gut very carefully.
There are also other common combinations of anomalies. These combinations often involve different systems working together. Some common ones include:
Knowing these patterns helps us give better care to those affected. Our team is here to offer advice and support to families dealing with these complex conditions.
Multiple congenital anomalies (MCAs) come from a mix of genetic, environmental, and health factors. It’s key to understand these to better care for babies before birth. Knowing what causes MCAs helps us improve prenatal care and outcomes for these children.
Genetics is a big part of MCAs. Chromosomal abnormalities and single-gene disorders can lead to multiple birth defects. We’re working to learn more about the genetics behind MCAs. This knowledge is vital for genetic counselling and planning families.
Exposure to harmful substances in pregnancy can raise the risk of MCAs. Teratogenic substances, like some chemicals and drugs, are linked to birth defects. We urge pregnant women to avoid harmful substances to lower the risk of MCAs.
Health issues in the mother, like diabetes and obesity, can increase the risk of MCAs. We emphasize the need for managing health conditions and a healthy lifestyle during pregnancy. This can help reduce the risk of MCAs.
Understanding the complex mix of genetic, environmental, and health factors in MCAs helps us prevent and intervene early. Our healthcare team is dedicated to giving personalized care and advice to families with MCAs.
Advances in prenatal diagnosis have changed how we care for unborn babies. We can now find and fix many problems earlier. This means we give parents more detailed and accurate information about their baby’s health.
Prenatal screening has gotten much better, with detection rates going up from 26% to 57%. This is thanks to new technologies and methods. We’ve moved past old ways of screening to use more advanced tests.
Several things have led to these changes:
Ultrasound is key in prenatal care, and it’s getting even better. New ultrasound tech gives us clearer images and more info about the baby. We use:
Genetic testing is also playing a big role in prenatal care. We have many options, including:
These advances have changed how parents make decisions. With more info early on, they can make better choices. We help parents understand their options and support them in making the right decisions.
We’re committed to top-notch healthcare and support for international patients. As we keep improving prenatal diagnosis, we aim to support families with complex fetal conditions.
Identifying specific patterns in multiple congenital anomalies (MCAs) has greatly improved our understanding. These patterns are key to understanding causes and managing these complex conditions.
The VATER/VACTERL association is a well-known pattern of MCAs. It includes Vertebral defects, Anal atresia, Tracheo-Esophageal fistula, Renal anomalies, and Limb abnormalities. Recent studies have explored the genetic and environmental factors behind it.
Other patterns include CHARGE syndrome, with Coloboma, Heart defects, Atresia of the choanae, Restricted growth, Genital abnormalities, and Ear anomalies. Each pattern has its own diagnostic criteria and management implications.
Research into MCAs is ongoing. It shows that genetic, environmental, and maternal health factors are key. Genetic testing has found specific mutations linked to MCAs. Understanding these mechanisms is vital for targeted interventions.
Recognizing patterns in MCAs is vital. It helps in diagnosis, guides management, and provides prognostic information. It also aids in counselling families about future pregnancy risks. By grasping the causes, we can improve patient care and outcomes.
We keep learning about MCAs through research and practice. This helps us diagnose and manage these complex conditions better.
Managing multiple congenital anomalies requires a detailed plan. Each patient’s needs are different. So, we tailor our approach to fit their specific situation.
A team of experts is key to treating these anomalies. Our team works together to create a care plan. This plan covers all aspects of the patient’s condition.
Surgery is a big part of managing these anomalies. We use the latest techniques to fix defects and improve life quality.
Key considerations for surgical interventions include:
Long-term care is essential for patients with these anomalies. Our team offers ongoing support and monitoring. This helps manage any complications that might come up.
Long-term care involves:
Supporting families is a big part of our work. We offer resources and advice to help families deal with their child’s condition.
Our caregivers are here to support and guide families. We make sure they get the help they need during their child’s care journey.
Multiple congenital anomalies are complex conditions that need a lot of care and support. Understanding MCAs is key to effective treatment and management. This is what we’ve learned in this article.
At Liv Hospital, we aim to use the latest medical knowledge and improve care together. Thanks to new prenatal diagnosis and treatments, people with MCAs have better chances. We’re dedicated to leading in research and care, giving families top-notch healthcare and support.
Dealing with multiple birth defects requires a team effort. By knowing the patterns and links of MCAs, we can offer better treatments and support. Our promise to provide full international patient support and guidance never wavers.
Multiple congenital anomalies occur when a baby is born with two or more major birth defects. These defects affect different parts of the body and can’t be caused by just one thing.
Congenital anomalies are a big health issue worldwide. The number of cases varies a lot from place to place.
The most common types include heart defects, facial and mouth issues, and problems with the digestive system. These can happen alone or together with other defects.
The causes are complex and involve many factors. Genetics, environmental factors, and the health of the mother all play a part.
New ways to check for these issues during pregnancy have improved. Ultrasound and genetic tests help doctors diagnose earlier.
The VATER/VACTERL association is a group of birth defects. It includes problems with the spine, anus, and heart, among others.
Treating these conditions requires a team of doctors. Surgery, ongoing medical care, and support for families are key to care.
Spotting patterns helps us understand the causes. It also helps us find better ways to manage and treat these conditions.
We offer support and guidance to families. Our team of experts provides nurturing care and advice.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!