Last Updated on November 27, 2025 by Bilal Hasdemir
Nearly 1 in 8 men will be diagnosed with prostate cancer during their lifetime. Surgery is a common treatment option.
After surgery, patients often need a urinary catheter to help with urination. The surgery can affect the urinary system, leading to issues with urination.
A catheter helps manage this by allowing urine to drain from the bladder. It’s important for patients to understand the role of a catheter after surgery.
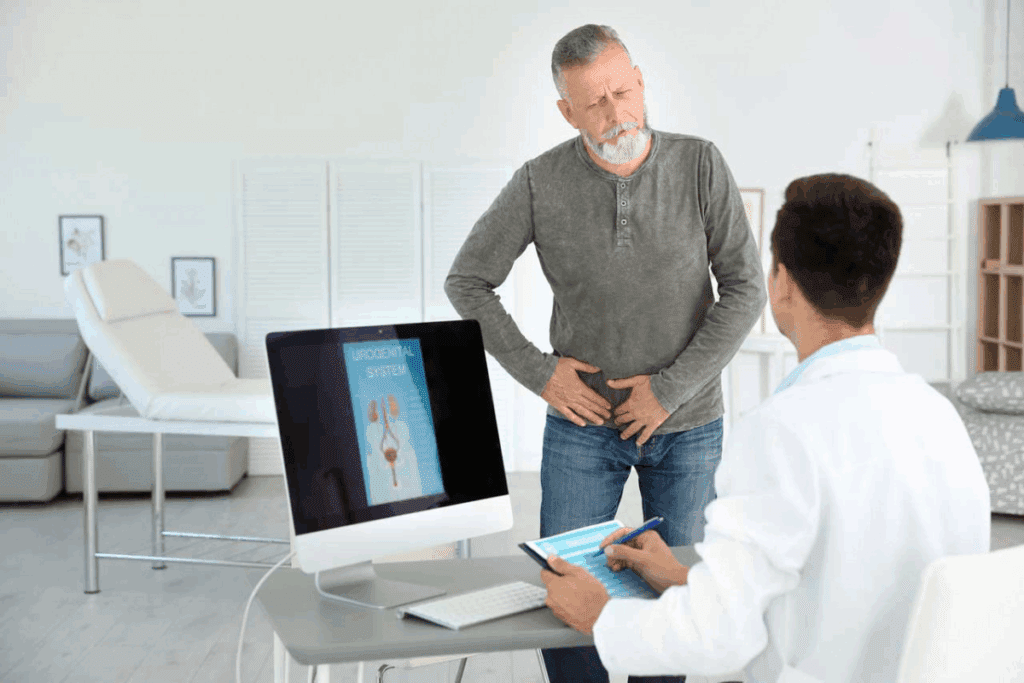
Prostate surgery, like robotic and open prostatectomy, affects how we pee. It’s a common fix for prostate problems. Knowing about it helps patients prepare.
There are many prostate surgeries, each with its own way of affecting our pee. The main ones are:
Each surgery has its good points and possible downsides, like pee problems.
Prostate surgery can mess with our pee in different ways. This might cause:
How much this happens depends on the surgery, your health, and the surgeon. Knowing this helps manage what to expect and how to care for yourself after surgery.
Understanding the differences in prostate surgeries and their pee effects helps patients get ready for their surgery and recovery.
Prostate surgery requires a catheter for healing and to avoid complications. The catheter is key in the early recovery stages. It allows urine to drain from the bladder, giving the body time to heal.
Prostate surgery can damage the area around the prostate gland. The catheter helps keep urine flowing, preventing retention or leakage. This is vital as the urethra and bladder need time to heal.
The catheter helps the bladder and urethra connection heal without long-term urinary problems. It lets doctors check urine flow and see how the body is healing.
Using a catheter after prostate surgery prevents many complications. Issues like urinary tract infections or bladder problems can be avoided with good catheter care.
Keeping the catheter area clean and following doctor’s advice can lower complication risks. The catheter also helps avoid urinary retention, which is painful and can lead to more problems if not treated quickly.
After prostate surgery, the type of catheter used can vary. Different catheters meet different needs. It’s important to know the options available.
Foley catheters are common after prostate surgery. They stay in for a while. A Foley catheter goes through the urethra into the bladder. It’s held by a balloon filled with sterile water.
Benefits of Foley Catheters:
Suprapubic catheters are for longer use. They go through the abdomen into the bladder. They’re used when the urethra can’t be used.
Advantages of Suprapubic Catheters:
Intermittent catheters are for draining the bladder at set times. They go through the urethra and are then taken out. Patients or caregivers do this.
Benefits of Intermittent Catheters:
| Catheter Type | Insertion Method | Duration of Use | Key Benefits |
| Foley Catheter | Through urethra | Short-term | Effective, easy to manage |
| Suprapubic Catheter | Through abdomen | Long-term | Bypasses urethral issues, comfortable |
| Intermittent Catheter | Through urethra, removed after use | Variable | Reduces infection risk, promotes independence |
“The choice of catheter after prostate surgery depends on several factors, including the type of surgery, patient health, and anticipated duration of catheterization.” –
Understanding the various types of catheters empowers patients and caregivers to make informed decisions. Each catheter has its own use and benefits. The right choice depends on the patient’s needs.
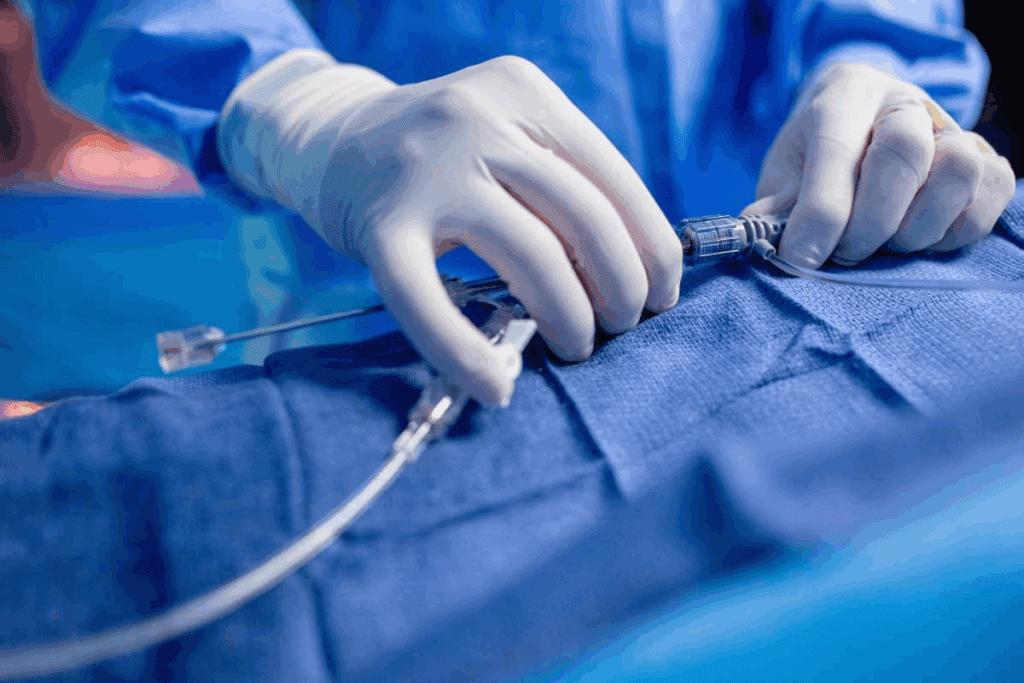
Learning about the catheter experience after prostate surgery can help reduce anxiety. A catheter is used to drain urine from the bladder. It’s a common part of care after prostate surgery.
The catheter is usually put in during surgery. The surgical team does this while the patient is asleep. This way, the patient doesn’t feel any pain during the process.
Patients might feel some discomfort or a foreign object feeling after the catheter is in. These feelings are normal and usually go away in a few hours or days. Talking to your healthcare provider about any ongoing discomfort is important.
Patients often wonder about the catheter’s purpose, how long it will stay in, and daily activities. They might worry about infection, leakage, and how it affects their life. Understanding these things can make patients feel more at ease during recovery.
Following your healthcare provider’s advice on catheter care is key. This helps avoid complications and makes recovery smoother. By doing this, patients can have a better recovery and less worry about catheter issues.
Knowing how long you’ll need a catheter after prostate surgery is key to recovery. The time needed varies by surgery type and patient factors.
The surgery type greatly affects catheter time. For example, a radical prostatectomy might need a longer catheter than a transurethral resection of the prostate (TURP). Most patients use a catheter for 1-2 weeks, but it can change.
Several things can make you need a catheter longer. These include:
Healthcare providers watch these factors to adjust your catheter time.
Each surgery has a usual time for using a catheter:
| Surgical Procedure | Typical Catheter Duration |
| Radical Prostatectomy | 1-2 weeks |
| TURP | 2-3 days |
| Simple Prostatectomy | 1-2 weeks |
Following your healthcare provider’s guidance on catheter use is crucial for a successful recovery. Everyone recovers differently.
Living with a catheter after prostate surgery means making some lifestyle changes. You need to think about your daily activities, sleep, and what you wear. These changes help you manage your condition well.
Having a catheter means you need to adjust your daily activities. You should avoid heavy lifting, bending, or hard exercises. Moderate walking is good for healing and stopping blood clots.
Sleeping with a catheter needs some adjustments for comfort and to prevent it from being dislodged. You should:
Choosing the right clothes is key to managing a catheter comfortably. Loose-fitting clothing is best. It lets the catheter and urine collection bag move without irritation or tightness.
By making these changes, patients can live more comfortably with a catheter after prostate surgery.
To keep risks low, it’s key to care for your catheter right. This means staying clean, handling the urine bag correctly, and knowing about possible problems.
Cleaning the area around the catheter is vital to avoid infections. Use mild soap and water to gently wash the area. Clean the catheter and the spot where it goes into your body every day.
Step-by-Step Cleaning Guide:
It’s important to empty the urine bag often to avoid overflow and infection. Empty it when it’s half full.
Tips for Emptying the Urine Bag:
Stopping infections is a big part of catheter care. Watch for signs like fever, cloudy or smelly urine, or redness around the catheter.
| Catheter Care Task | Frequency | Purpose |
| Cleaning the catheter site | Daily | Prevent infection |
| Emptying the urine collection bag | When half full | Prevent overflow and infection |
| Checking for signs of infection | Regularly | Early detection of complications |
By following these care tips, you can lower risks and make recovery easier after prostate surgery.
Catheter-related discomforts, such as urethral irritation and bladder spasms, are common after prostate surgery. They can be effectively managed.
Urethral irritation is a frequent complaint among patients with a catheter. To alleviate this discomfort, it’s essential to ensure the catheter is properly secured. This prevents unnecessary movement.
Using a catheter securement device can help reduce irritation by keeping the catheter in place.
Additional Tips: Applying a lubricating gel around the catheter insertion site can also help minimize irritation. It’s important to follow the healthcare provider’s instructions for catheter care to avoid complications.
Bladder spasms can be painful and are sometimes associated with catheter use. Medications such as anticholinergics may be prescribed to help manage these spasms.
It’s essential to discuss any spasm-related discomfort with your healthcare provider to determine the best course of treatment. Staying hydrated and avoiding irritants like caffeine and spicy foods can also help reduce the frequency of bladder spasms.
Pain management is a critical aspect of catheter care. Over-the-counter pain relievers may be recommended, but it’s important to consult with your healthcare provider before taking any medication.
In some cases, the catheter may need to be adjusted or repositioned to alleviate discomfort. Patients should not attempt to adjust or remove the catheter themselves but instead seek guidance from their healthcare provider.
It’s important to know about the possible problems with catheters after prostate surgery. Catheters are usually safe, but there are some issues to watch out for. This helps in managing your recovery well.
Urinary tract infections (UTIs) are a common problem with catheters. They happen when bacteria get into the urinary tract through the catheter. Symptoms include pain when you pee, needing to pee a lot, and a fever.
Prevention is key: Keeping the catheter and the area around it clean can lower the risk of UTIs. Patients are often told to follow strict hygiene practices.
Catheter blockage is another issue. It happens when urine can’t flow properly, causing discomfort. If not fixed quickly, it can lead to serious problems.
To avoid this, know the signs of blockage, like less urine coming out or leakage. Flushing the catheter regularly, as your healthcare provider suggests, can help prevent blockages.
| Signs of Catheter Blockage | Following your healthcare provider’s guidance on catheter use is crucial for a successful recovery. |
| Reduced urine output | Notify your healthcare provider immediately |
| Leakage around the catheter | Check for kinks in the catheter tubing |
| Pain or discomfort | Ensure the catheter is not twisted or obstructed |
Leakage around the catheter can be upsetting. It might happen for several reasons, like the size of the catheter, blockages, or bladder spasms.
“Managing leakage involves understanding its cause. Healthcare providers can offer guidance on adjusting the catheter or treating underlying conditions.”
If you have ongoing leakage, talk to your healthcare provider. They can help figure out why it’s happening and how to fix it.
In summary, while catheters are a common part of recovery after prostate surgery, knowing about possible problems like UTIs, blockage, and leakage is key. Working closely with your healthcare provider can help manage these risks.
After prostate surgery, seeing blood in your urine is a sign to pay attention. If you have a catheter, this might happen. It’s important to know if it’s just normal bleeding or if there’s a bigger issue.
Some bleeding is okay after prostate surgery. But, some signs need medical help. It’s key to know the difference between normal bleeding and complications.
Normal bleeding after surgery usually gets less over time. But, complications might show as more blood, pain, or trouble with the catheter.
Blood clots can block urine flow in the catheter. Watch for signs like less urine or hard resistance when trying to clean the catheter.
Steps to manage blood clots include:
Knowing when to get help is important. Call your doctor if you see:
Quick medical care can avoid bigger problems and help you heal faster.
Knowing how to keep clean with a catheter is key to getting better. Keeping the area clean stops infections and helps the catheter work right.
It’s okay to shower with a catheter, but you must be careful. Before you shower, make sure the catheter is secure. This stops it from getting pulled or caught.
When you shower, don’t let the catheter or bag get wet. Use a chair or stool if you need to sit. Also, keep the water not too hot or cold to avoid discomfort.
Keeping the area around the catheter clean is very important. Use mild soap and lukewarm water to clean. Clean from front to back to avoid bacteria.
| Cleaning Practice | Benefit |
| Gentle soap and lukewarm water | Reduces irritation and infection risk |
| Cleaning from front to back | Prevents bacterial introduction into the urinary tract |
| Drying the area thoroughly | Reduces moisture that can lead to infection |
Skin irritation around the catheter can happen. To avoid this, dry the area well after showering. Use a barrier cream or ointment to protect the skin.
Check the catheter and its securement often to avoid irritation. If irritation happens, talk to your doctor.
After prostate surgery, many wonder about sex and closeness. They might ask about what they can and can’t do. It’s all about understanding the limits and moving forward.
A catheter can really affect sex. Doctors usually say no to sex with it in to avoid pain and risks like infection. It’s key to know this to plan your recovery wisely.
Understanding these limits helps manage what to expect. It guides you in making smart choices for your healing.
Talking openly with your partner is vital. Share your feelings and the changes you’re facing. This can actually bring you closer.
Intimacy is more than just sex. It’s about feeling close and connected. You can stay close through doing things together, talking, and touching in ways that don’t involve sex.
| Ways to Maintain Intimacy | Benefits |
| Shared Activities | Enhances emotional connection |
| Conversations | Fosters understanding and closeness |
| Non-sexual Physical Touch | Maintains physical closeness without discomfort |
After the catheter comes out, you can usually start having sex again. But always check with your doctor first. They’ll tell you when it’s safe based on how you’re healing.
Prostate surgery can sometimes change how you feel about sex. You might face issues like not being able to get an erection. Talk to your doctor about these changes and what you can do about them.
Start slow when you do start having sex again. Be open with your partner about any pain or problems you face.
Catheter removal is a simple procedure that helps you get back to normal urination. It’s done by a healthcare professional in a clinical setting.
Following your healthcare provider’s guidance on catheter use is crucial for a successful recovery.
The removal is quick, taking just a few minutes. You might feel a bit of discomfort or relief as it’s taken out.
Removing a catheter isn’t usually painful, but some might feel a bit of discomfort or stinging. This feeling is usually short-lived and goes away soon after.
Right after, you might leak a bit or feel a burning sensation while peeing. Drinking water and following your doctor’s advice can help. These feelings are normal and should pass quickly.
Knowing what to expect during catheter removal can ease your worries. It’s important to follow your doctor’s advice and let them know if you have any issues after the removal.
After the catheter is taken out, patients start to feel better in controlling their urine. This is a big part of getting better after prostate surgery.
How fast patients get better varies. Most start to feel better a few weeks after the catheter is removed. “The time it takes to get better depends on the surgery type, health, and doing pelvic floor exercises.”
It’s important to remember that getting better takes time. Some people might get better faster, while others might take longer.
Pelvic floor exercises, or Kegel exercises, are very important. They help the muscles that help you control your bladder. “Doing Kegel exercises regularly can really help with staying dry.”
Many people have trouble controlling their urine after the catheter is removed. It’s important to manage this well to recover smoothly. Using absorbent products and keeping clean can help a lot. One patient said, “
Using adult diapers helped me feel more secure during the initial recovery phase.
“
Drinking plenty of water and avoiding things like caffeine and spicy foods can also help. These can make bladder problems worse.
By knowing how long it takes to get better, doing pelvic floor exercises, and managing incontinence, patients can greatly improve their urine control after the catheter is removed.
Knowing when to seek medical help is key to a smooth recovery after prostate surgery. It’s important to watch for signs of catheter problems and know when to act.
There are several signs that might mean you have a catheter issue. These include:
Some catheter problems are emergencies. You need to get help fast if you have:
In emergencies, call your healthcare provider or go to the emergency room without delay.
At follow-up visits, ask important questions. This ensures you’re using your catheter correctly and addresses any worries. Consider asking:
Being proactive and asking questions can help ease your mind and make recovery smoother.
Getting ready for prostate surgery is essential for a smooth recovery. It’s important to prepare both mentally and physically. Knowing what to expect, like using a catheter and managing care, helps a lot.
Being well-informed helps face the challenges of recovery. This includes understanding catheters, managing complications, and getting back to normal with urination. Mental preparation is also key to handle the emotional side of healing.
Recovering well from prostate surgery means being ready mentally and physically. By focusing on these, people can recover faster and get back to their lives sooner. This ensures a successful recovery after surgery.
A catheter helps manage urination issues after prostate surgery. It allows urine to drain from the bladder. This helps the healing process.
Foley catheters, suprapubic catheters, and intermittent catheters are common. Each type meets different patient needs and is used for different lengths of time.
The time needed with a catheter varies by surgery type. It usually lasts 1-2 weeks. But, recovery times can differ.
Yes, you can shower with a catheter. But, it’s important to follow cleaning guidelines. This prevents skin irritation.
You might feel some discomfort, like urethral irritation or bladder spasms. But, there are ways to manage these issues.
Following your healthcare provider’s guidance on catheter use is crucial for a successful recovery.
Removing a catheter is usually not painful. But, you might feel some discomfort. Knowing the process can help ease worries.
After removal, you’ll start to regain control over urination. You might need to do pelvic floor exercises. Managing temporary incontinence is also part of the process.
Contact your doctor if you notice warning signs of complications. This includes urinary tract infections or catheter blockage. Also, reach out if you have concerns about managing your catheter.
Blood in urine can be normal after surgery with a catheter. But, it’s important to tell the difference between normal bleeding and signs of complications that need medical help.
Watch the catheter and urine output for blood clots. If clots cause blockages or other problems, seek medical help.
Look out for decreased or stopped urine output, pain, or discomfort. If you notice these signs, get medical help right away.
Prevent infections by following proper catheter care. This includes cleaning, emptying the urine bag regularly, and watching for infection signs.
The length of time you can wear a catheter varies. It depends on your needs and the type of catheter. For example, suprapubic catheters are used for longer periods.
Choose loose, comfortable clothes that don’t put pressure on the catheter site. This makes managing the catheter and urine bag easier.
You might need to limit your activities to avoid discomfort or complications. Your healthcare provider can give specific guidance.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!