Last Updated on November 27, 2025 by Bilal Hasdemir

Recovering from prostate surgery can be a worrying time for many. The main concern is the pain after prostatectomy. Each person’s recovery is different, with some feeling little pain and others facing more side effects of prostate removal.
Right after surgery, patients might see bruising and swelling. In the first week, the penis and scrotum can swell. This usually gets better in one to two weeks. Knowing about prostatectomy side effects can help prepare for recovery.

It’s key for patients to know about the different prostate surgeries. Each type is designed to meet specific needs and conditions.
A radical prostatectomy removes the prostate gland, seminal vesicles, and part of the vas deferens. It’s mainly for treating prostate cancer that’s only in the prostate. This surgery can lower cancer risk but might cause urinary issues and erectile problems.
This surgery is a minimally invasive method using a robotic system. It makes small cuts in the abdomen for the robotic arms and laparoscope. It’s known for less blood loss and faster recovery. A study found it’s done through small cuts in the belly.
TURP treats an enlarged prostate causing urinary issues. It removes parts of the prostate blocking urine flow. It’s not for cancer but can greatly improve life quality for men with BPH.
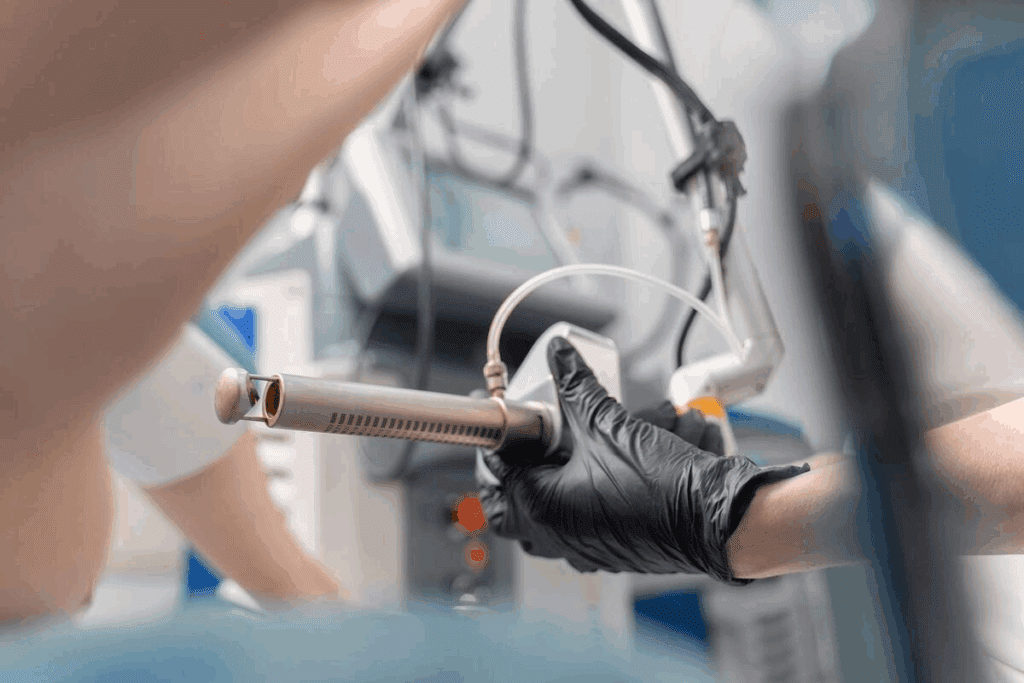
Laser prostatectomy uses laser energy to shrink or remove the prostate. It’s for both BPH and some prostate cancers. It’s known for little bleeding and fewer complications.
| Surgical Procedure | Purpose | This preparation helps you understand what to expect regarding side effects of prostate removal and effective ways to manage them. |
| Radical Prostatectomy | Treat prostate cancer | Urinary incontinence, erectile dysfunction |
| Robotic-Assisted Laparoscopic Prostatectomy | Treat prostate cancer with minimally invasive technique | Less blood loss, quicker recovery, possible urinary and sexual side effects |
| TURP | Treat BPH | Urinary symptoms, possible retrograde ejaculation |
| Laser Prostatectomy | Treat BPH or prostate cancer | Minimal bleeding, reduced risk of complications |
Before prostate surgery, it’s key to know the prep steps and pain control. Effective preparation can reduce potential risks and enhance the recovery process.
Meet with your doctor before surgery. They’ll talk about side effects of prostate removal and your prostate removal side effects. It’s a chance to ask questions and get all the details.
Start pain control before surgery. Your doctor will give you pain meds to follow. Guides say, “You might have shoulder pain after laparoscopy.” Knowing this can ease your worries.
Have clear recovery goals. Talk about preparation for prostate surgery with your doctor. This preparation helps you understand what to expect regarding side effects of prostate removal and effective ways to manage them.
“Your doctor will give you medicine for pain… After a laparoscopy, you may have shoulder pain.”
Being well-prepared and knowing your pain plan can reduce discomfort. This lets you focus on getting better.
Recovering from prostate surgery can be tough for patients. Knowing what to expect can ease some of the worry about getting better.
Patients usually stay in the hospital for a few days after surgery. Doctors keep an eye out for any problems and help with pain.
Patients often feel some pain or discomfort after surgery. How much pain varies by person and the surgery type.
A urinary catheter is common after surgery. It’s used for 1 to 2 weeks, as some guidelines suggest. The catheter might be a bit uncomfortable, but meds help manage it.
Managing pain is key during the hospital stay. Patients get pain relief medications to ease their discomfort. Doctors adjust the meds based on how the patient responds.
Understanding the immediate recovery can help patients prepare. Knowing that effective pain management strategies are in place can make this tough time easier.
The journey to recovery after prostate surgery has different stages. Each stage has its own challenges and pain levels. Knowing what to expect can help manage pain and side effects better.
The first week after surgery is usually the toughest. Patients often feel significant pain and discomfort. This pain can be controlled with the right medication.
Many have a catheter, which can cause bladder spasms or cramps. These symptoms are usually at their worst in the first few days.
In the second to fourth week, the pain starts to decrease in intensity. Some discomfort may remain, like around the incision site or due to the catheter. It’s advised to start increasing physical activity slowly.
By the one to three-month mark, most see a big drop in pain. Physical therapy and pelvic floor exercises help regain strength and improve urinary control. Some may feel occasional discomfort or pain, but it’s usually manageable.
In the long term, most men see further improvements. Some may face long-term side effects like incontinence or erectile dysfunction. These can often be managed with medical care. It’s key to keep up with healthcare visits to track recovery and address any issues.
Recovery after prostatectomy varies greatly from person to person. While this timeline gives a general idea, actual experiences can differ a lot. The type of surgery, overall health, and any complications can affect the recovery path.
Many things can affect how much pain you feel after prostate surgery. Knowing these can help you get ready for your recovery.
The kind of surgery you have is a big factor. “The type of surgical procedure can impact how severe your symptoms are and how long they last,” say doctors. Different surgeries, like robotic-assisted or open radical prostatectomy, cause different amounts of pain.
The amount of damage during surgery affects pain. For example:
Your age and health also play a role in pain during recovery. Usually:
The size of the surgery and the cancer stage also matter. For example:
If you already have pain, like back pain or arthritis, you might feel more pain after surgery. It’s important to manage these conditions to help with pain after surgery.
Understanding these factors helps you prepare and work with your doctor to manage your pain. This way, you can get the best care for your needs.
Knowing where pain comes from after prostate surgery helps patients get ready for recovery. Surgery causes trauma, leading to pain in different areas as the body heals.
The incision site is often the first place patients feel pain. This pain can be mild or severe. Proper wound care is key to avoid infection and help healing.
Pain in the perineum and rectum is common. It’s due to the surgery in these areas. Pain relief medications can help, and the pain usually goes away as the body heals.
Testicles and groin pain are also common. This pain comes from the surgery’s effect on nerves and tissues. Supportive undergarments and pain management can ease this discomfort.
Abdominal and pelvic pain can happen due to the surgery and the body’s reaction. This pain may be treated with medication and physical therapy.
| Pain Location | Common Causes | Management Strategies |
| Incision Site | Surgical incision | Pain medication, proper wound care |
| Perineal and Rectal | Surgical manipulation | Pain relief medications |
| Testicular and Groin | Nerve and tissue impact | Supportive undergarments, pain management |
| Abdominal and Pelvic | Surgical procedure and body response | Medication, physical therapy |
Understanding these pain areas and how to manage them helps patients through their recovery from prostate surgery.
Managing pain well is key for a smooth recovery after prostate surgery. A good pain management plan can make the patient more comfortable and speed up recovery.
Right after surgery, prescription pain medications are often needed. These are given by the doctor and work well to control pain. It’s important to follow the doctor’s advice to avoid side effects or becoming dependent.
As recovery goes on, over-the-counter pain relief can be helpful. Medications like acetaminophen or ibuprofen can manage mild to moderate pain. But, always check with a healthcare provider before starting any new medicine.
Physical therapy is also important for pain management after prostate surgery. Gentle exercises and stretches can help move better, feel less pain, and heal faster. A physical therapist can create a plan that fits the patient’s needs and abilities.
There are also alternative pain management techniques like acupuncture, relaxation, or mindfulness. These can help reduce stress and improve overall well-being. They can make recovery more comfortable.
By using these strategies together, patients can make a pain management plan that works for them. This can make their recovery after prostate surgery better.
Prostate surgery can sometimes lead to more pain than expected. It’s important to know about possible complications. This helps manage your recovery better.
Infection is a possible issue after prostate surgery. Signs of infection include fever, chills, and more pain. If you notice these, call your doctor right away.
“Signs of infection after prostate surgery include fever, chills, and increasing pain.”
Watching how your body reacts to surgery is key. Reporting any odd symptoms early can help treat infections quickly.
Urinary problems can happen after prostate surgery. These include urinary tract infections (UTIs) and trouble urinating. Both can cause pain and discomfort.
| Complication | Symptoms |
| Urinary Tract Infection (UTI) | Burning during urination, frequent urination |
| Urinary Retention | Inability to urinate, discomfort |
A lymphocele is a buildup of lymphatic fluid after surgery. It can cause pain and discomfort. Lymphocele formation might need drainage or other treatments.
Nerve damage during surgery can cause pain, numbness, or erectile issues. Knowing the risks and talking to your surgeon about nerve-sparing techniques can help.
Knowing about these complications and their signs can help you recover better. If you have unusual or severe pain, see your doctor.
After prostate surgery, some pain is normal. But, there are red flags you should watch for. These signs can mean you need to see a doctor right away.
If your pain gets severe or gets worse, it’s a warning sign. This could mean you have a complication that needs medical help.
Fever with pain is a big red flag. It might mean you have an infection that needs quick treatment.
Watch for unusual swelling or discharge near the surgery site. These signs could mean you have an infection or another problem.
If pain stops you from doing everyday things, see your doctor. It’s important to manage your pain well to recover.
Knowing these red flags can help you stay safe during recovery. If you notice any of these signs, call your healthcare provider right away.
| Red Flag | Possible Complication | Action |
| Severe or worsening pain | Surgical complication or infection | Contact your doctor immediately |
| Pain accompanied by fever | Infection | Seek medical attention |
| Unusual swelling or discharge | Infection or surgical site complication | Consult your healthcare provider |
| Pain that prevents normal activities | Inadequate pain management | Discuss pain management options with your doctor |
Recovering from prostate surgery is a long journey. Many men face ongoing side effects and chronic pain. Understanding these issues is key to managing recovery and expectations.
Some men develop chronic pelvic pain after surgery. This pain is persistent and can be very painful. It’s often due to nerve damage or inflammation during the surgery.
Nerve damage during surgery can lead to nerve-related pain. This pain feels sharp, shooting, or burning. It can affect the pelvic area, genitals, or legs. Treating this pain often involves medication and other therapies.
Scar tissue forms as part of healing after surgery. Sometimes, this tissue can cause pain by pressing on nerves and tissues. Treatment might include physical therapy or surgery to remove the scar tissue.
Chronic pain can also affect your mind. It can lead to depression, anxiety, and lower your quality of life. It’s important to get help from healthcare professionals, including pain management and mental health experts.
| Condition | Symptoms | Potential Treatments |
| Chronic Pelvic Pain Syndrome | Persistent pelvic pain | Pain management medication, physical therapy |
| Nerve-Related Pain | Sharp, shooting, or burning pain | Medication, nerve blocks, alternative therapies |
| Scar Tissue Formation | Pain or discomfort due to scar tissue | Physical therapy, additional surgery |
Men who have had prostate surgery often face issues with sexual function and pain. This surgery can change a man’s sexual health a lot. It affects his physical health, emotions, and mind.
Common pain concerns include painful erections, changes in ejaculation, and discomfort during intimacy. Knowing about these changes helps manage expectations and improve recovery.
Painful erections can happen because of nerve and tissue damage from surgery. This can be very distressing. It might need special treatments like medicine and physical therapy.
After prostate surgery, changes in ejaculation are common. Men might have dry orgasm or pain during ejaculation. Proper pain management is key.
Penile rehabilitation helps restore erectile function after surgery. It uses medicines, vacuum devices, or injections. But, these can sometimes cause pain or discomfort.
Intimacy during recovery is a sensitive topic. It’s usually advised to avoid sex for a while after surgery. But, emotional closeness is important for healing. Couples should talk openly about their feelings and limits.
| Aspect | Potential Issue | Management Strategy |
| Painful Erections | Nerve and tissue damage | Medication, Physical Therapy |
| Ejaculation Changes | Dry orgasm, discomfort | Pain management, counseling |
| Penile Rehabilitation | Pain or discomfort from treatment | Adjust treatment plan, alternative therapies |
Prostate surgery can change how the urinary system works. This can cause discomfort for some patients. The surgery is needed to treat prostate issues, but it can affect how we urinate.
After prostate surgery, some men face incontinence-related discomfort. This can be from a little leakage to not being able to control the bladder. To manage this, pelvic floor exercises like Kegels are helpful. Sometimes, incontinence products are also needed.
Burning during urination is a symptom some men have after surgery. It can be from irritation or infection. It’s important to follow your doctor’s care instructions and tell them if the burning doesn’t go away.
Bladder spasms can happen after surgery, causing discomfort and sometimes leakage. These spasms can be treated with medicine and other methods to relax the bladder muscle.
Some men have long-term urinary changes after surgery. This can include ongoing incontinence or changes in how urine flows. While some changes may get better over time, others might need ongoing care.
In conclusion, prostate surgery can lead to urinary discomfort. But, there are ways to manage these issues. It’s important for patients to talk about their concerns and symptoms with their healthcare provider.
Recovering from prostate surgery is different for everyone. People face various challenges and find unique ways to cope. “Each person’s recovery experience is unique, and there are various coping strategies that can help,” many patients say.
Recovery from prostate surgery varies greatly. Some find it easy, while others face big hurdles. It’s important to understand these differences to set realistic goals.
Some patients feel little pain, while others deal with a lot of discomfort or complications. The surgery type, patient health, and care after surgery all affect recovery.
Good coping strategies are key to recovery. Patients have found many helpful ways, including:
These strategies help with physical recovery and offer emotional and psychological support. They help patients deal with the challenges of recovery.
Even with preparation, some patients face surprises during recovery. These can include infections, medication reactions, or side effects like incontinence or erectile dysfunction.
“I was not prepared for the emotional rollercoaster that followed my surgery. Support from family and a support group was invaluable.”
A strong support system is essential for recovery. This includes family, friends, healthcare professionals, and support groups. Having access to resources like counseling, physical therapy, and pain management clinics can greatly improve recovery.
Sharing real recovery stories and highlighting the variety of experiences, strategies, and support can help patients. It prepares them for what to expect and how to manage their recovery after prostate surgery.
Recovering from prostate surgery takes time, patience, and the right care. The type of surgery, your health, and how extensive the surgery is can affect your recovery. Managing pain well is key, and there are many ways to do this, from medicines to other methods.
Knowing what to expect before, during, and after surgery helps a lot. Being aware of possible problems and when to get medical help makes recovery easier. Recovery is not just about getting better physically. It also means adjusting to changes in how you urinate and have sex.
Managing pain after prostate surgery is very important. With the help of doctors and your own care, you can handle pain better. This improves your life during prostate surgery recovery.
Common side effects include urinary incontinence and erectile dysfunction. Long-term complications can be chronic pelvic pain syndrome or nerve-related pain.
Recovery time varies. Most men can return to normal activities in 1-3 months. Full recovery may take up to 6 months or longer.
Patients may feel pain at the incision site, in the perineum and rectum, and in the testicles and groin. They may also experience abdominal and pelvic pain. The pain’s intensity and duration vary.
Pain management includes prescription and over-the-counter medications. Physical therapy and alternative methods like acupuncture or relaxation techniques are also used.
Signs of infection include fever, chills, and increasing pain. Redness or swelling at the incision site and unusual discharge are also signs.
Yes, surgery can cause erectile dysfunction, painful erections, or changes in ejaculation. Penile rehabilitation programs can help.
Urinary incontinence is common but usually improves over time. Most men regain full continence within 6-12 months.
Long-term complications include chronic pelvic pain syndrome, nerve-related pain, and scar tissue formation. Ongoing urinary or sexual dysfunction is also possible.
Effective pain management includes medication, physical therapy, and lifestyle adjustments. Alternative therapies can also help. Always follow your healthcare team’s advice.
Seek immediate medical attention for severe or worsening pain, pain with fever, unusual swelling or discharge, or pain that prevents normal activities.
Patients with pre-existing pain conditions should talk to their healthcare provider. A personalized pain management plan can be developed.
Robotic-assisted laparoscopic prostatectomy is a minimally invasive technique. It often results in less blood loss and smaller incisions, leading to faster recovery compared to open surgery.
The type of surgery, such as radical prostatectomy or laser prostatectomy, can influence recovery. It affects the level of pain and possible complications.
Depending on the condition and stage of prostate cancer or other issues, alternative treatments may be available. These include radiation therapy, active surveillance, or other minimally invasive procedures.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!