Last Updated on November 27, 2025 by Bilal Hasdemir
Medical technology has advanced a lot, leading to new ways to care for the heart. This has made people wonder if it’s possible to live without a natural heart. In the United States, thousands of people get heart transplants or use ventricular assist devices (VADs) every year. The answer is amazing! Discover the medical devices and procedures that allow a person to function without a natural heart. Can you live without a heart?
The idea of living without a heart might sound like something from science fiction. But, thanks to total artificial hearts (TAHs) and other new devices, it’s now a reality. Patients can now survive and even live well without their natural heart.
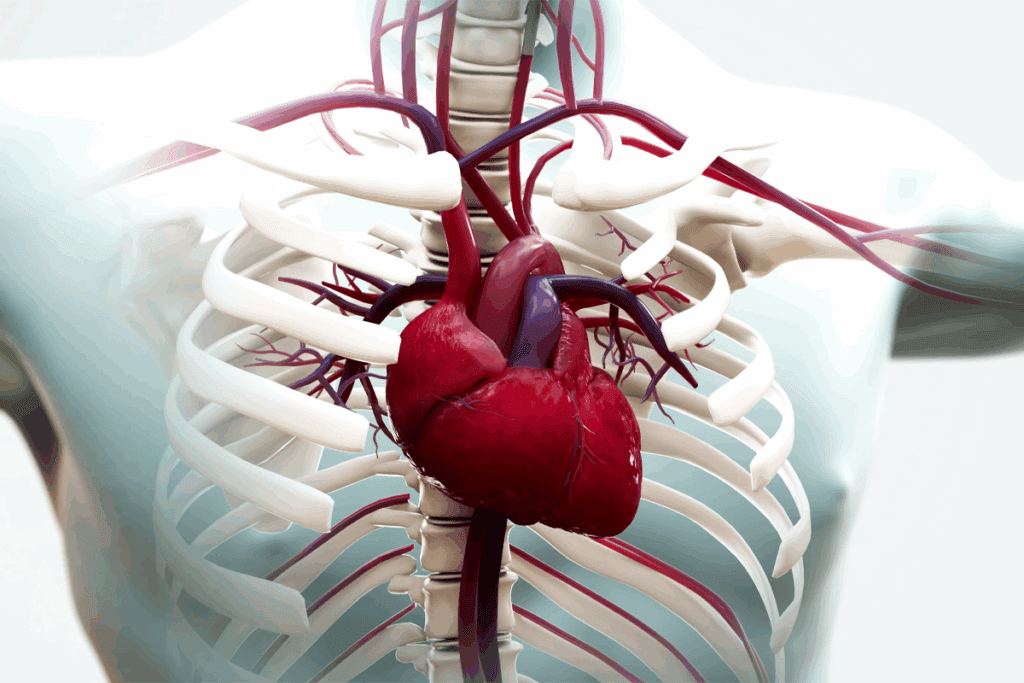
The heart is at the heart of human life. It pumps blood all over the body. This brings oxygen and nutrients to tissues and takes away waste.
The human heart is a strong muscle with four chambers. The heart’s anatomy helps blood flow well. The atria get blood coming back, and the ventricles send it out.
The heart beats thanks to electrical signals. Knowing how the heart works shows its key role in life.
The heart is vital because without it, health problems and death can happen. CA Heart and Vein Specialists say heart failure can harm other organs. The heart keeps us alive by working all our lives.
Here’s why the heart is so important:
The heart’s role in heart living and health is huge.
Living without a heart is now possible thanks to mechanical heart replacements. This medical breakthrough has changed the lives of those with severe heart issues.
“Living without a heart” means people who have had their heart replaced or removed. They survive with the help of technology. This includes artificial hearts or other devices that pump blood like a natural heart.
Artificial hearts work like the real thing, pumping blood. They’re for those waiting for a transplant or can’t get one.
It’s important to know the difference between heart replacement and removal. Heart replacement means swapping the natural heart for an artificial one or a donor heart. Heart removal is when the heart is taken out, usually for a transplant.
| Procedure | Description | Outcome |
| Heart Replacement | Surgical substitution of the natural heart with an artificial or donor heart | Patient survives with artificial or transplanted heart |
| Heart Removal | Surgical removal of the heart, often for transplant | Patient survives with transplanted heart or mechanical support |
Stan Larkin’s story, living 555 days with an artificial heart, shows what’s possible. Such tales show that living without a natural heart is within reach, thanks to medical advancements.
Living without a heartbeat might sound like something from science fiction. But, it’s a temporary reality for some patients going through heart surgery. Thanks to medical tech, like cardiopulmonary bypass, people can live without a beating heart for a little while.
Cardiopulmonary bypass (CPB) is a method that takes over the heart and lungs during surgery. It lets surgeons work on a heart that’s not beating. CPB is key for keeping blood flowing and oxygen in the body when the heart stops.
With CPB, the blood goes to a heart-lung machine. This machine pumps and adds oxygen to the blood. It makes it possible for surgeons to do complex heart surgeries that were once impossible.
How long someone can survive during cardiac arrest depends on many things. Cardiac arrest survival rates change a lot based on the cause of the arrest and how fast treatment starts. CPR and defibrillation can help keep someone alive for a short time.
Survival time without a heartbeat is usually just minutes. Medical help like CPB or ECMO can extend this time. But, the longer someone goes without a heartbeat, the less likely they are to survive without brain damage or other serious problems.
Advances in artificial heart tech have given new hope to those with severe heart failure. The journey to create a reliable artificial heart has been long and complex. It has involved big steps in technology and medicine.
The idea of an artificial heart has been around for decades. The first self-contained artificial heart was put in a person in 2001. This was a big step forward in artificial heart history. Ever after, there have been many improvements to make artificial hearts better.
There have been many key moments in artificial heart tech’s growth. These include:
The progress in artificial heart tech has not just saved lives. It has also made patients’ lives better. As research keeps going, we’ll see even more advanced devices. These will bring more hope to those needing heart replacement therapy.
It’s important to know how artificial hearts work. They help patients with severe heart failure. Artificial hearts replace or support the natural heart’s function.
An artificial heart pumps blood like the natural heart does. It has pumps, valves, and sensors. These work together to keep blood flowing.
The device connects to the bloodstream. It can replace the heart or help it work better.
Artificial hearts run on batteries. These batteries are usually outside the body. They connect to the device through the skin.
The battery life depends on the device and how active the patient is. Most need to be recharged several times a day. Better batteries mean patients can move more easily and live better lives.
Even with big steps forward, artificial hearts have limits. There’s a risk of infection and device failure. Also, they need batteries, which can be big and uncomfortable.
Researchers are working hard. They want to make artificial hearts smaller, more efficient, and reliable. This will help patients even more.
Mechanical heart replacements have changed how we treat heart failure. They offer hope to those with severe heart problems. These devices help or replace the heart’s pumping action.
Total Artificial Hearts replace the whole heart. They pump blood and act as heart chambers. TAHs are for those waiting for a transplant or with badly damaged hearts.
TAHs are a big step forward in treating heart failure.
Ventricular Assist Devices are pumps that help the heart. They support one or both heart chambers. VADs help patients wait for a transplant or are a long-term solution.
There are temporary and permanent mechanical heart replacements. Temporary ones, like some VADs, help until a transplant or recovery. Permanent ones, like TAHs, are for long-term use.
The choice depends on the patient’s condition and needs.
In conclusion, today’s mechanical heart replacements offer many options. As technology improves, we’ll see more advancements in this field.
For those with severe heart disease, heart transplantation is the top choice. It involves swapping a sick heart with a healthy one from a donor. This process is detailed and requires matching the donor and recipient carefully.
The heart transplantation process starts with checking if the recipient can have the surgery. When a good donor heart is found, the transplant happens. The surgery removes the sick heart and connects the new one to the recipient’s blood vessels.
The transplantation process also includes care after the surgery. This is key for the recipient’s healing. It involves managing possible problems and keeping the immune system in check to avoid rejection.
Thanks to better surgery and treatments, more people survive heart transplants. The one-year survival rate is about 85-90%. The five-year rate is around 70-75%. The recipient’s health, other medical issues, and following care advice affect how long they live.
Despite its success, heart transplantation has big challenges. There’s a shortage of donor hearts, a risk of rejection, and a need for lifelong medication. These issues can affect how well a recipient lives and how long they live. Researchers are working hard to solve these problems and improve transplant outcomes.
Living without a natural heart is now possible, thanks to advancements in technology. Stan Larkin lived for 555 days with an artificial heart. His story, along with others, shows how far cardiac tech has come. It also shows how patients can live full lives with mechanical hearts.
Stan Larkin’s case is truly remarkable. He used a SynCardia total artificial heart (TAH) for 555 days, a record. The SynCardia TAH is a temporary fix for those waiting for a heart transplant. Larkin’s story proves it can keep someone alive for a long time.
Larkin’s life with the artificial heart was more than just survival. He did daily activities and even traveled. He said, “I was able to live a relatively normal life, and that’s something that I never thought I’d be able to do.”
“The advancements in artificial heart technology have been nothing short of revolutionary. Patients like Stan Larkin are testaments to the power of these devices to save and improve lives.”
Stan Larkin’s story is inspiring, but he’s not alone. Many patients have benefited from artificial hearts and ventricular assist devices (VADs). Each has their own story and outcome.
| Patient | Device | Duration |
| Stan Larkin | SynCardia TAH | 555 days |
| Patient X | HeartMate III | 300 days |
| Patient Y | CardiacAssist TandemHeart | 120 days |
These stories highlight the progress in cardiac care. They show the hope artificial heart technology brings to patients and their families. As tech keeps improving, we’ll see even more amazing stories of life without a natural heart.
Artificial heart technology is changing society and raising ethical questions. It has made a big difference in medicine, giving hope to those with heart failure.
Artificial hearts have changed how we treat heart failure. They offer a new option for patients, improving survival and quality of life.
Advancements in Medical Practice
But, there are big worries about who can get artificial hearts and how much they cost. The high price and complex surgery make it hard for many to get them.
| Factor | Impact on Accessibility |
| Cost of Device | High cost limits accessibility |
| Insurance Coverage | Variability in coverage affects access |
| Medical Infrastructure | Adequacy of facilities and expertise influences accessibility |
Living with an artificial heart can greatly improve life, but it comes with challenges. Patients must get used to a mechanical device, manage battery life, and face possible complications.
As artificial heart tech gets better, we can expect even more benefits for patients. It’s key to tackle the ethical and societal issues to ensure everyone has access and gets the most out of this technology.
The idea of living without a natural heart is getting closer thanks to new artificial heart tech. Total artificial hearts and ventricular assist devices have changed how we treat heart failure. They give hope to those waiting for transplants or who can’t have traditional heart surgery.
The future of artificial hearts looks bright. Researchers are working hard to make devices last longer, lower the risk of problems, and improve life quality. But, we’re not there yet. Today, these devices are meant for short-term use until a donor heart is found.
These advancements in artificial hearts are changing cardiac care. They also bring up big questions about access, cost, and ethics. As we get closer to better artificial hearts, we must tackle these issues. This ensures everyone who needs them can get them.
Thanks to ongoing innovation and investment, living without a natural heart is becoming a real option. It’s no longer just a dream. It’s a chance for a new life for many patients around the world.
Heart transplant patients usually live 10-15 years on average. But, thanks to new tech, some live up to 20 years or more.
Living without a heart for long is not possible. Yet, artificial hearts or ventricular assist devices help some survive for a while.
An artificial heart is a machine that pumps blood like a real heart. It runs on a battery and can be put inside the body.
A total artificial heart replaces the real heart. A ventricular assist device helps the real heart pump blood.
Living with an artificial heart’s time varies. It depends on the device type and the person’s health. Some live several years.
Today’s artificial hearts have limits. They need power from outside, can get infected, and might fail.
Artificial hearts have changed society. They help people with heart failure live longer. But, they also raise questions about access and cost.
No, surviving long without a heartbeat is not possible. But, medical tech like cardiopulmonary bypass can help temporarily.
Artificial heart development started in the 1950s. Over time, we’ve seen big advances, leading to today’s devices.
Heart transplants are complex. They face challenges like finding donor hearts, risk of rejection, and needing lifelong meds.
Survival during cardiac arrest varies. It depends on quick and effective medical help.
Ventricular assist devices are key in heart failure treatment. They support the heart, helping patients until a transplant or recovery.
Artificial hearts can be permanent for some. But, they’re often used as a bridge to transplant or until the heart heals.
We’ve made big strides in artificial heart tech. But, more research is needed for a permanent artificial heart.
Patients with artificial hearts face many challenges. They need ongoing care, risk complications, and face daily activity impacts.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!