Last Updated on November 27, 2025 by Bilal Hasdemir
Many men worry about bladder control after prostate surgery. Understanding the timeline for recovery is crucial. It helps manage hopes and reduces stress.
Most men can stop leaking urine after surgery. This is true for those between 40 and 60 years old and in good health. For them, incontinence after prostate surgery usually goes away in three months.
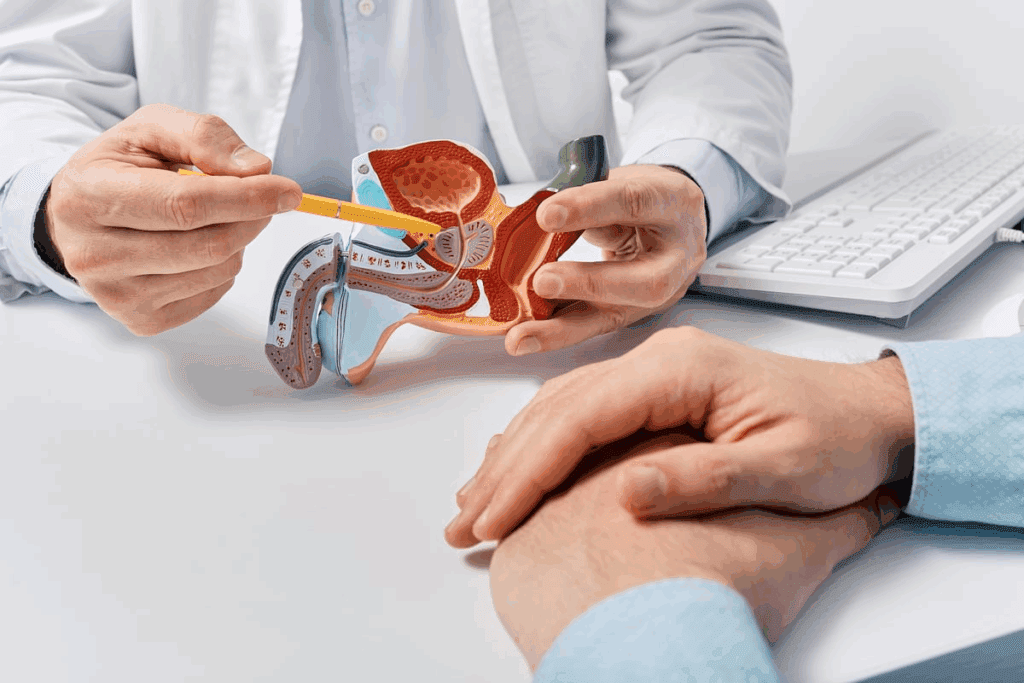
It’s important for patients and doctors to know how prostate surgery affects urine control. Radical prostatectomy, a common surgery for prostate cancer, can harm urine control.
There are many prostate surgery types, each affecting urine differently. The main ones are:
The type of surgery chosen can greatly impact urine control. Radical prostatectomy can have a big impact because it removes the prostate and can damage nerves and muscles.
Urinary incontinence after surgery happens because of damage to the urinary sphincter and nerves. The surgery can harm the muscles and nerves around the prostate. This makes it hard for the bladder to hold urine.
| Cause | Description | Impact on Urinary Continence |
| Damage to Urinary Sphincter | The surgery can weaken or damage the urinary sphincter. | Leads to stress incontinence. |
| Nerve Damage | Nerves controlling the bladder and sphincter can be injured. | Affects bladder control and sensation. |
| Removal of Prostate Gland | The prostate gland is removed, altering the urinary tract anatomy. | Can lead to issues with urine flow and continence. |
Knowing these details is key for managing what to expect and how to recover after surgery. It’s vital for patients to talk with their doctors about their specific risks and outcomes.
Recovering bladder control after prostate surgery takes time. Knowing the stages helps manage expectations and guide the recovery.
Right after surgery, many men face urinary incontinence. This is due to damage to the surrounding tissues and muscles. A catheter is used to help the healing process. After it’s removed, some incontinence is common.
In the early stages, the body starts to heal. Men may see slight improvements in bladder control. But, stress incontinence, where leakage happens during activities like coughing, is common. Pelvic floor exercises, like Kegel exercises, can help strengthen the muscles that support bladder control.
In the mid-term, many men see big improvements in bladder control. The pace of improvement varies. But, most regain a lot of continence within three to six months. It’s key to keep up with pelvic floor exercises to support this recovery.
For some, full recovery takes longer than six months. It can take up to a year or more. Age, health, and the surgery method affect the recovery time. Patience and sticking to pelvic floor exercises are vital during this time.
Knowing the typical recovery timeline helps men prepare for the journey. While results vary, being informed and proactive can greatly help.
Urinary incontinence after prostate surgery is not just one issue; it’s several. These include stress, urge, and overflow incontinence. Knowing about these types is key to treating it well.
Stress urinary incontinence is the most common issue after prostate surgery. It happens when moving or pressure on the bladder makes you leak urine. This is often because the muscles that control urination get weak.
Symptoms of stress incontinence include leaking when you cough, sneeze, laugh, or lift heavy things. Pelvic floor exercises, like Kegels, can help make these muscles stronger and improve bladder control.
Urge urinary incontinence is when you suddenly feel a strong need to pee and then can’t hold it. It’s often linked to an overactive bladder. This can be very upsetting and affect your daily life.
The reasons for urge incontinence can be complex. They might include nerve problems, bladder muscle issues, or other health issues. Diagnosis usually involves urodynamic testing to check how the bladder works.
Overflow incontinence happens when the bladder doesn’t empty fully, causing constant or frequent leaking. This can be due to blockages or a weak bladder muscle. Some people might have a mix of symptoms, including stress, urge, and overflow incontinence.
Managing overflow incontinence might involve using a catheter to empty the bladder fully. Or, treatments might focus on fixing the blockage or weak muscle.
Understanding the timeline for recovery is crucial.
Age and health status are big factors in bladder control recovery time. Older people or those with health issues might need more time.
Staying healthy with a good diet and exercise can help. Healthy living might lead to better bladder control.
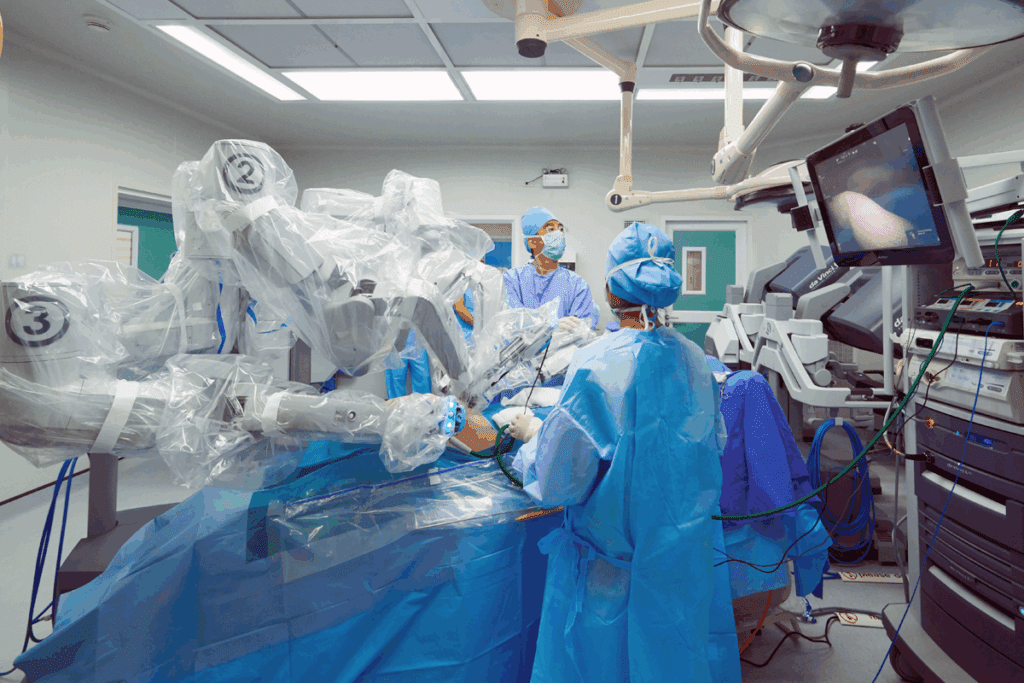
The surgery method and the surgeon’s skill are key. Experienced surgeons often do better at keeping urinary function intact.
| Surgical Technique | Description | Impact on Recovery |
| Robotic-Assisted Surgery | Minimally invasive technique using robotic instruments | Potential for less tissue damage and faster recovery |
| Open Prostatectomy | Traditional open surgery method | May result in longer recovery times due to larger incision |
Urinary function before surgery is also important. Those with better function before surgery tend to recover faster. Checking urinary function before surgery can help predict recovery challenges.
How well nerves are saved during surgery affects recovery. Nerve-sparing techniques lead to better function and quicker recovery.
Understanding these factors helps patients plan their recovery better. It lets them make informed choices about their care after surgery.
Pelvic floor exercises are key for men to regain bladder control after prostate surgery. Kegel exercises, in particular, strengthen the muscles that help control the bladder. This improves continence.
Kegel exercises involve contracting and releasing the pelvic floor muscles. To do a Kegel exercise right, find the right muscles. You can do this by stopping urine flow midstream. But, don’t make this a habit to avoid incomplete bladder emptying.
To do Kegel exercises, contract the pelvic floor muscles for 5-10 seconds, then release for the same duration. Repeat this 10-15 times per session, aiming for three sessions a day. Kegel exercises improve bladder control, sexual function, and speed up recovery after surgery.
Consistency is vital in pelvic floor exercises. Creating a routine and sticking to it boosts their effectiveness. Start slow and increase intensity and frequency as muscles get stronger.
Adding other pelvic floor exercises like pelvic tilts and bridges to your routine is beneficial. Consulting with a healthcare provider or a physical therapist specializing in pelvic health can help tailor a routine that meets your needs.
Tracking progress is key to seeing if your exercises are working. Keeping a journal or using a mobile app to track workouts and bladder control changes is helpful.
If progress is slow or if you face challenges, adjust your exercise routine or seek professional help. Be patient, as regaining bladder control takes time, effort, and the right guidance.
Prostate surgery can cause urinary incontinence. But, there are treatments to help control the bladder again. The appropriate treatment depends on the severity of incontinence, the individual’s health, and other relevant factors.
Some medicines can help with urinary incontinence after prostate surgery. These include:
“The use of anticholinergics can significantly improve the quality of life for men experiencing urinary incontinence after prostatectomy.”
Biofeedback therapy is a non-invasive treatment. It helps patients control their pelvic floor muscles. This therapy involves:
Biofeedback therapy works well with pelvic floor exercises (Kegels).
Electrical stimulation is another option for post-prostatectomy incontinence. It involves:
It’s important for patients to talk to their healthcare provider. They can decide the best treatment plan for their condition.
When other treatments don’t work, surgery like male sling procedures and artificial urinary sphincter implantation can help. These options offer relief from persistent incontinence.
The appropriate treatment depends on the severity of incontinence, the individual’s health, and other relevant factors.
Male sling procedures help by placing a supportive sling around the urethra. This is often for men with mild to moderate stress urinary incontinence.
The appropriate treatment depends on the severity of incontinence, the individual’s health, and other relevant factors.
Artificial urinary sphincter (AUS) implantation is a top choice for severe urinary incontinence. It has a cuff around the urethra, a pump in the scrotum, and a balloon in the abdomen.
It has a high success rate, with many men becoming fully continent. But, it’s a complex surgery with possible mechanical failure or complications.
Bulking agent injections add material around the urethra to improve its function. This is less invasive than other options and works for mild incontinence.
It’s generally safe, but how well it works can vary. You might need more than one injection to keep the incontinence under control.
Think about surgery when other treatments don’t help enough. A healthcare provider will evaluate you to find the best surgery for your situation.
Talking to a healthcare provider about risks, benefits, and outcomes is key. This helps you make a well-informed decision.
Recovering from bladder control issues after prostate surgery needs a few key steps. Using incontinence products, staying hydrated, and planning physical activities are important. These steps can make the recovery period easier.
The right incontinence products can greatly improve life during recovery. Options include absorbent pads, adult diapers, and male external catheters.
Drinking enough water is key, but it’s also important to plan bathroom visits. Drinking less water at certain times and setting a regular bathroom schedule can help manage incontinence.
| Strategy | Description | Benefit |
| Timed Voiding | Voiding at regular intervals (e.g., every 2 hours) | Reduces frequency of incontinence episodes |
| Fluid Management | Limiting fluids in the evening | Minimizes nighttime incontinence |
Rest is important, but so is staying active. Yet, some activities might need to be avoided to prevent making incontinence worse.
Gentle exercises, like pelvic floor exercises (Kegels), can help. But, high-impact activities like running or heavy lifting should be avoided until a healthcare provider says it’s okay.
Incontinence can impact social life and work. Using incontinence products can boost confidence. Also, planning ahead, like knowing where restrooms are, can help in social situations.
By using these strategies, people can manage their daily lives better during bladder control recovery. This can improve their overall quality of life.
Recovering bladder control after prostate surgery involves many lifestyle changes. Understanding and making these changes can help patients recover better.
Eating well is key to recovery. Some foods and drinks can make the bladder worse. For example, caffeine and spicy foods can irritate it. It’s also important to drink the right amount of water to stay hydrated without overdoing it.
Keeping a healthy weight is important for bladder control. Extra weight can strain the pelvic floor muscles. Regular exercise helps manage weight and improves health.
Talking to a healthcare provider about exercise is a good idea. They can suggest activities that strengthen the pelvic floor, like Kegel exercises.
Alcohol and caffeine can make bladder control worse. They irritate the bladder and make you need to urinate more often. Cutting down on these can help with incontinence after prostate surgery.
Quitting smoking is also important for bladder control. Smoking can cause chronic coughing, which strains the pelvic floor muscles. Quitting smoking improves bladder control and overall health.
By making these lifestyle changes, patients can improve their bladder control and quality of life after prostate surgery.
Many myths surround post-prostatectomy incontinence, affecting recovery and well-being. Men often don’t know what to expect with their urine control after surgery. This lack of knowledge can cause stress and slow down healing.
One big myth is that incontinence after prostate surgery is permanent. But, many men regain control of their bladder over time. Research shows that with the right treatment and exercises, many men see big improvements in their continence.
“The majority of men will experience some level of incontinence after prostate surgery, but this is not always a permanent condition.”
Another myth is that nothing can help speed up bladder control recovery. But, there are many ways to help. Pelvic floor exercises, like Kegels, are very effective in improving bladder control. Changes in lifestyle and some medical treatments can also help.
Some men think incontinence after surgery means it failed. But, this isn’t true. Incontinence is a possible side effect, not a sign of failure. Surgery success is usually about treating cancer, not side effects like incontinence.
Knowing the truth about post-prostatectomy incontinence can reduce anxiety. It helps men face their surgery with better understanding and hope.
Urinary incontinence after prostate surgery deeply affects men’s lives. It’s not just about getting better physically. It’s also about dealing with the emotional and psychological sides of incontinence.
Men often feel frustrated, anxious, and depressed after surgery. It’s important to acknowledge these feelings and seek help. Recognizing the emotional impact of incontinence is the first step towards healing. Ways to cope include:
“The psychological impact of incontinence should not be underestimated. Men need to feel supported and understood during their recovery.”
Support groups and counseling are key for men dealing with incontinence’s psychological effects. These resources offer a safe place to talk and get advice and support.
“Support groups were invaluable to me. Hearing others’ stories and knowing I wasn’t alone made a huge difference.” –
Anonymous Patient
Talking openly with loved ones is vital. Sharing feelings and experiences can strengthen bonds and reduce isolation. It’s essential to educate loved ones about the challenges of incontinence and the support needed during recovery.
Incontinence shouldn’t stop men from being social. With the right support and strategies, they can stay active socially. Planning ahead, using the right products, and staying in touch with friends and family are key.
By tackling the psychological impact of incontinence and keeping a strong support network, men can improve their quality of life. It’s about healing both physically and emotionally.
If you’re dealing with ongoing incontinence after prostate surgery, knowing when to see a doctor is key. Some incontinence is normal after surgery. But, certain signs might mean you need medical help.
It’s important to watch out for signs of complications or unusual symptoms during recovery. These can include:
At follow-up appointments, ask the right questions to understand your recovery better. Consider asking:
| Question | Purpose |
| What is the expected recovery timeline for my bladder control? | Understand the typical recovery process and timeline. |
| Are there any specific exercises or therapies that can help improve my incontinence? | Learn about recommended treatments or exercises. |
| What are the signs of complications that I should watch out for? | Be aware of possible complications and their signs. |
| Are there any lifestyle changes that I can make to aid in my recovery? | Discover lifestyle changes that can help your recovery. |
Being informed and proactive helps you work with your healthcare provider. Together, you can tackle ongoing incontinence and aim for the best recovery after prostate surgery.
Getting bladder control back after prostate surgery is different for everyone. Incontinence is a common issue, but knowing how to manage it can help. Understanding the recovery time and available strategies can ease worries.
Doing pelvic floor exercises, like Kegels, and making lifestyle changes can help. For those who can’t stop leaking, there are medical and surgical options. These can offer relief from persistent incontinence.
Talking to a healthcare provider is key to finding the right treatment. They can help address any issues that come up during recovery. With the right plan, many people can regain bladder control and enjoy a better life after surgery.
Recovering bladder control is a journey that needs patience and the right support. Knowing what affects recovery and taking action can make the process easier. With confidence and the right steps, individuals can overcome this challenge.
The time to regain bladder control after prostate surgery varies. Most men see big improvements in 6-12 months.
After prostatectomy, common urinary incontinence types are stress, urge, and overflow incontinence.
Pelvic floor exercises, like Kegels, strengthen muscles that control urination. This improves bladder control and reduces incontinence.
Surgical options like male slings and artificial sphincters can manage incontinence. But, they also have risks and complications.
To manage daily life, use incontinence products and stay hydrated. Adjust physical activity and social interactions too.
Lifestyle choices like diet, weight, and smoking affect recovery. Healthy choices can improve incontinence.
Yes, treatments like medications, biofeedback, and electrical stimulation can manage incontinence after prostatectomy.
Consult your doctor for ongoing incontinence if symptoms persist or worsen. Or if you have recovery or treatment concerns.
To cope, seek support from healthcare, support groups, and loved ones. Practice stress-reducing techniques and stay active socially.
Common myths include thinking incontinence is always permanent or that nothing can speed recovery. Some believe incontinence means the surgery failed.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!