Robotic surgery has changed the medical world. It offers a new way to do surgeries that’s less invasive than old methods. Over 1.2 million robotic surgeries were done worldwide in 2020. Many of these were robotic hysterectomies. But, what does it mean to have this surgery, and are patients awake? For a laparoscopic hysterectomy or other robotic procedures, are you awake? Get the crucial facts about anesthesia and being put to sleep.
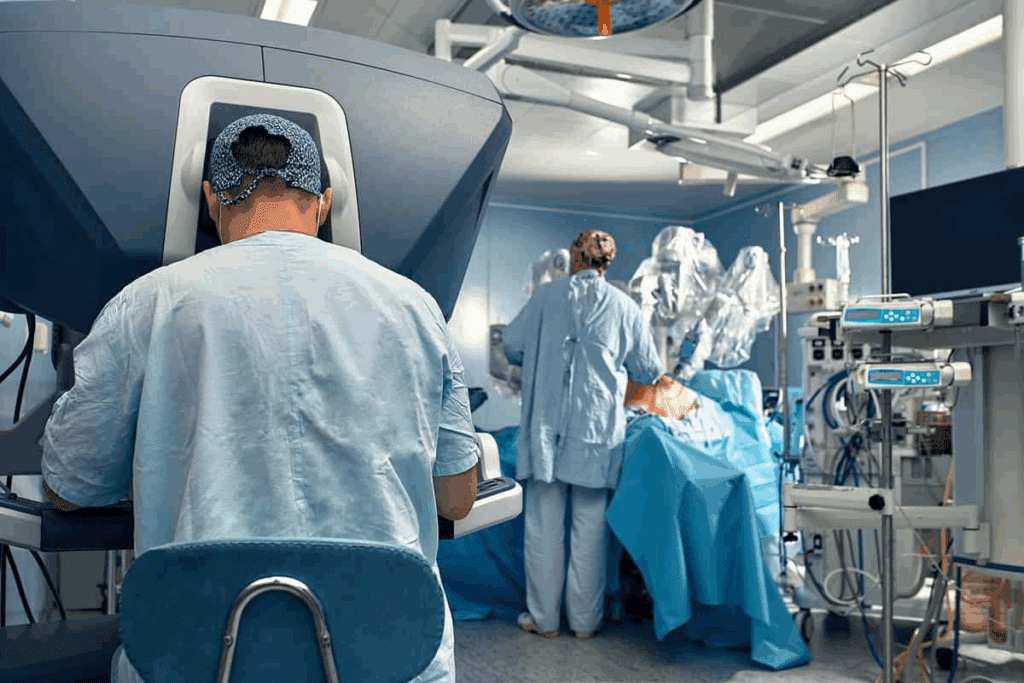
Robotic surgery, like da vinci hysterectomy, uses a robotic system. It helps surgeons do precise work through small cuts. This tech has made surgeries better, with less recovery time and less scarring.
Key Takeaways
- Robotic surgery is a minimally invasive procedure.
- Patients are typically under general anesthesia during robotic surgery.
- Robotic hysterectomy offers several benefits, including less scarring and quicker recovery.
- The da vinci system is a commonly used robotic platform.
- Robotic surgery is performed by trained surgeons with specialized expertise.
Understanding Robotic Surgery for Hysterectomy
Robotic-assisted hysterectomy is a modern surgery that brings better precision and control. It combines the good parts of small incisions with the latest in robotic tech. This makes it a top choice for many gynecological issues.
What is a Robotic-Assisted Hysterectomy?
A robotic-assisted hysterectomy uses a robotic system to help the surgeon. It lets them work with more precision, flexibility, and control than old methods.
The Evolution of Minimally Invasive Gynecological Surgery
Minimally invasive gynecological surgery has grown a lot, with robotic-assisted surgery being a big step forward. Robotic systems have made it easier and more accurate for surgeons to do complex surgeries.
| Feature | Traditional Laparoscopic Surgery | Robotic-Assisted Surgery |
| Visualization | 2D visualization | High-definition 3D visualization |
| Instrumentation | Straight instruments with limited range | Wristed instruments with enhanced dexterity |
| Surgeon Control | Direct manual control | Enhanced control through robotic interface |
Da Vinci Surgical System and Current Technologies
The Da Vinci Surgical System is a top choice for many surgeries. It offers clear 3D views and precise tools. This makes it easier for surgeons to do complex surgeries.
Robotic systems like the Da Vinci have changed gynecological surgery a lot. They offer many benefits to both patients and surgeons.
Anesthesia During Robotic Hysterectomy: Are You Awake?
Many patients wonder if they are awake during a robotic hysterectomy. The answer depends on the type of anesthesia used and why it’s chosen.
Types of Anesthesia Used in Robotic Surgery
There are two main types of anesthesia for robotic hysterectomy: general and regional. General anesthesia makes you completely unconscious. Regional anesthesia numbs a certain area of your body.
General anesthesia is the usual choice for robotic hysterectomy. It keeps you pain-free and perfectly steady during the surgery.
Why General Anesthesia is Standard Practice
General anesthesia is the top pick for robotic hysterectomy for good reasons. It lets doctors control your breathing, which is key during laparoscopic surgeries. It also makes sure you’re comfortable by blocking pain and anxiety.
Patient Consciousness and Awareness Considerations
One worry with general anesthesia is the chance of being aware during surgery. Thanks to advanced monitoring, this risk is now very low.
Special Cases Where Regional Anesthesia Might Be Used
Even though general anesthesia is common, there might be times when regional anesthesia is better. This choice depends on your health, any medical conditions, or the surgeon’s preference.
In summary, patients usually don’t wake up during robotic hysterectomy because of general anesthesia. Knowing why this is helps ease worries and gets you ready for your surgery.
The Laparoscopic Hysterectomy Procedure Explained
Laparoscopic hysterectomy is a surgery that removes the uterus through small cuts in the belly. It’s less painful and has quicker recovery times than traditional surgery. This makes it a popular choice for many women.
Pre-Surgical Preparation and Planning
Before the surgery, patients go through several steps. They get a medical check-up, talk about their health history, and do any needed tests. They’re also told to stop certain medicines that could affect the surgery or healing.
Patient Positioning for Robotic Hysterectomy
The patient is placed in a special position for the surgery. They lie on their back with their feet up. This helps move the intestines out of the way, giving the surgeon a clear view.
Incision Placement and Port Insertion
The surgeon makes small cuts in the belly for the instruments and a camera. The camera shows images on a screen, helping the surgeon see inside. The exact number and where the cuts are made can vary.
Step-by-Step Surgical Process
The surgery has several important steps. First, the surgeon finds and cuts the uterine arteries. Then, the uterus is freed and removed through the belly or vagina.
How the Uterus is Removed During Surgery
Removing the uterus is a key part of the surgery. Sometimes, it’s taken out whole through the vagina. Other times, it’s cut into pieces to fit through the small cuts.
Internal Stitches and Closure Methods
After removing the uterus, the surgeon closes any cuts inside and repairs the area. The belly cuts are then closed with stitches or staples. The choice of how to close depends on the size and where the cuts are.
| Procedure Step | Description | Key Considerations |
| Pre-Surgical Preparation | Medical evaluation and testing | Patient’s medical history, medications |
| Patient Positioning | Trendelenburg position | Access to pelvic area, comfort |
| Incision Placement | Small incisions for instruments | Number and placement vary |
| Uterus Removal | Through vagina or incisions | Intact or morcellated |
| Closure | Sutures, staples, or glue | Method depends on incision size |
What to Expect in the Operating Room
The operating room for a robotic hysterectomy is a place of precision and teamwork. It’s where a skilled team works together to achieve success.
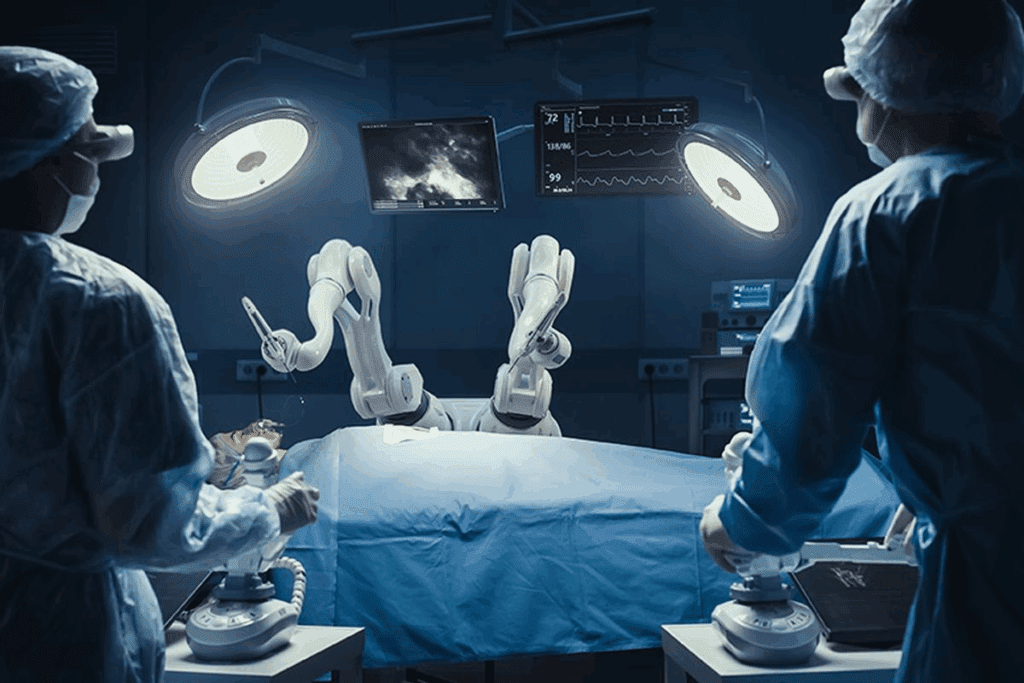
The Surgical Team and Their Roles
The surgical team is key to a successful procedure. It includes the surgeon, anesthesiologist, nurses, and surgical technologists. Each one has a specific job, from using the robotic system to watching the patient’s health.
How Long Does a Robotic Hysterectomy Take?
The time it takes for a robotic hysterectomy varies. It depends on the case’s complexity and the patient’s health. Generally, it lasts from 2 to 4 hours.
The Surgeon’s Control vs. The Robot’s Function
The surgeon uses a console to control the robotic system. This console shows a clear view of the area being operated on. The robotic tools move just like the surgeon’s hands, making precise and detailed work possible.
Monitoring During Surgery
The patient’s health is watched closely during surgery. The anesthesiologist and team keep an eye on heart rate, blood pressure, and oxygen levels. This ensures the patient’s safety during the operation.
| Team Member | Role |
| Surgeon | Operates the robotic system and performs the hysterectomy |
| Anesthesiologist | Administers anesthesia and monitors the patient’s vital signs |
| Nurses and Surgical Technologists | Assist the surgeon and ensure the operating room is prepared |
Benefits of Choosing a Robotic Laparoscopic Hysterectomy
Robotic laparoscopic hysterectomy is a modern surgery that offers many benefits. It makes recovery faster and the surgery safer. This method is a big change from older ways of doing hysterectomies.
Advantages of Minimally Invasive Techniques
These surgeries use small cuts, which means less damage to the body. This leads to less pain after surgery and fewer problems. The robotic tools help the surgeon work more accurately.
Enhanced Surgical Precision and Visualization
The robotic system gives surgeons clear 3D views of the area they’re working on. This makes it easier to do detailed work. The tools can move in ways humans can’t, making the surgery more precise.
Reduced Blood Loss and Tissue Trauma
Robotic laparoscopic hysterectomy means less blood loss than open surgery. The small cuts and precise tools reduce damage to tissues. This leads to fewer problems and a quicker recovery.
Shorter Hospital Stay and Faster Return to Activities
People who have this surgery usually stay in the hospital for less time. They can get back to their daily life sooner than those who have open surgery. This is a big plus, letting women get back to their routines faster.
- Faster recovery times
- Less post-operative pain
- Smaller incisions
- Reduced risk of complications
Choosing robotic laparoscopic hysterectomy is a smart choice for women. It offers a safer, more efficient surgery. And it means a quicker return to normal life.
Potential Risks and Side Effects of Robotic Hysterectomy
It’s important for patients to know about the risks and side effects of robotic hysterectomy. This surgery is usually safe, but it’s good to know about possible problems.
Common Post-Operative Complications
After robotic hysterectomy, patients might face infections, bleeding, or reactions to anesthesia. They could also feel pain, swelling, or bruising at the cut sites. Proper post-operative care can help avoid these issues.
Rare but Serious Risks to Consider
Even though rare, serious risks include damage to nearby organs, blood clots, and issues with the robotic tools. Surgeon experience and skill are key in lowering these risks.
Anesthesia-Related Concerns
General anesthesia carries risks like breathing and heart problems. People with health issues might be more at risk.
Risk Comparison with Traditional Hysterectomy Methods
Robotic hysterectomy is compared to open and laparoscopic hysterectomies. It often means less recovery time and less blood loss than open surgery. But, risks can vary based on the patient and the surgeon.
Recovery from Robotic Hysterectomy Week by Week
Recovering from a robotic hysterectomy takes time. It involves several stages, from right after surgery to long-term care. Knowing these stages helps patients prepare for what’s ahead and when.
Immediate Post-Operative Experience (Days 1-3)
The first few days after surgery are key. Patients might feel pain, tiredness, and some bleeding or spotting. It’s important to follow the doctor’s instructions to manage pain and avoid problems.
First Week Recovery Milestones
In the first week, rest and avoid hard work. Walking a bit is okay to keep blood flowing and prevent clots. Most patients go home a day or two after surgery.
Weeks 2-4: Healing Progress and Activity Levels
In weeks two to four, you can start doing more. But, avoid heavy lifting and hard exercise. It’s important to see your doctor during this time to check on your healing.
Months 1-3: Return to Normal Life
By the end of the first month, you’ll likely feel much better. You can start doing your usual things again. Everyone heals differently, so the time it takes can vary.
Managing Pain, Swelling, and Incision Care
Managing pain is a big part of recovery. Doctors usually give pain meds to help. Taking care of swelling and incisions is also key.
Long-term Outcomes and Follow-up Care
Long-term care is important for the best results. Regular doctor visits help track your healing and solve any issues that come up.
Understanding the recovery process week by week helps patients heal better after a robotic hysterectomy.
Comparing Different Types of Hysterectomy Procedures
There are many ways to do hysterectomy surgery. These include open abdominal, vaginal, laparoscopic, and robotic-assisted methods. It’s important for both patients and doctors to know about these options to choose the best one.
Open Abdominal Hysterectomy vs. Robotic Approach
An open abdominal hysterectomy uses a big cut in the belly to reach the uterus. On the other hand, a robotic-assisted hysterectomy makes small cuts and uses a robot. The robotic approach can lead to less blood loss and shorter hospital stays. But, it might not be right for everyone, like those with complex health issues or a history of many surgeries.
Vaginal Hysterectomy Considerations
Vaginal hysterectomy is done through the vagina, avoiding belly cuts. This can mean less pain after surgery and faster recovery. Yet, it depends on the uterus size and if there are adhesions.
Standard Laparoscopic vs. Robotic-Assisted Techniques
Both laparoscopic and robotic-assisted hysterectomies are minimally invasive. Robotic surgery gives better views and precision, which can help some patients more.
How Surgeons Determine the Best Approach for Each Patient
Doctors look at many things when choosing a surgery method. They consider the patient’s health, why the surgery is needed, and their medical history. This way, each patient gets the care that’s best for them.
Conclusion: Making an Informed Decision About Your Hysterectomy
It’s important to understand the different types of hysterectomy surgery. This includes robotic and laparoscopic hysterectomies. The Da Vinci system has made these surgeries more precise and faster to recover from.
The choice of surgery depends on several things. These include the patient’s health, the surgeon’s skills, and the technology used. For example, the da vinci system is a key factor in robotic surgeries.
Patients should talk to their doctors to find the best option for them. They need to weigh the benefits and risks of each surgery. Being well-informed helps make choices that are good for their health.
FAQ
What is a robotic hysterectomy?
A robotic hysterectomy is a surgery to remove the uterus. It uses a robotic system, like the Da Vinci Surgical System, for a minimally invasive procedure.
Are you awake during robotic hysterectomy?
No, patients are usually not awake during this surgery. General anesthesia is used to keep them comfortable.
How long does a robotic hysterectomy take?
The surgery can last from 1 to 3 hours. This depends on how complex the case is.
What are the benefits of robotic laparoscopic hysterectomy?
Benefits include less invasive techniques and better precision. There’s also less blood loss, a shorter hospital stay, and a quicker recovery.
What are the risks and side effects of robotic hysterectomy?
Risks and side effects include common complications and rare serious ones. There are also concerns about anesthesia.
How is the uterus removed in a robotic hysterectomy?
The uterus is removed through small incisions in the abdomen. The robotic system helps dissect and extract it.
What is the recovery time for robotic hysterectomy?
Recovery time varies, but most can return to normal activities in 2-4 weeks. Full recovery takes several months.
How many internal stitches are used after a hysterectomy?
The number of internal stitches varies. It depends on the case and the surgeon’s technique.
What is the difference between robotic and laparoscopic hysterectomy?
Robotic hysterectomy is a type of laparoscopic surgery. It uses a robotic system for better precision and visualization.
Can I have regional anesthesia for robotic hysterectomy?
While general anesthesia is common, regional anesthesia might be considered in some cases. But it’s not the usual choice for this surgery.
How is pain managed after robotic hysterectomy?
Pain is managed with medications and other post-operative care strategies. This helps patients feel better.
What are the long-term outcomes of robotic hysterectomy?
Long-term outcomes are positive. Most patients see a significant improvement in their quality of life.
How do surgeons determine the best approach for hysterectomy?
Surgeons look at the patient’s health, the reason for the surgery, and their anatomy. This helps decide the best surgical approach.
References
- Barud, M., Turek, B., Dąbrowski, W., & Siwicka, D. (2025). Anesthesia for robot-assisted surgery: A review. Anaesthesiology Intensive Therapy, 57(2), e100-e110. https://www.ait-journal.com/pdf-203168-125538?filename=125538.pdf
































