Did you know that nearly 20% of spine surgeries may not work as well as hoped? This fact shows how vital it is to know the failure rate of spine surgery and the risks of spinal surgical procedures. We will look at what makes these outcomes vary, giving you a full picture of spine surgery outcomes and the numbers behind them.
Exploring spinal surgery reveals that success depends on many things. This includes the surgery type and the patient’s health. Our aim is to share the spine surgery statistics that help patients choose the best treatment for them.
Key Takeaways
- Spine surgery failure rates vary significantly based on the procedure type.
- Patient factors play a critical role in determining surgical outcomes.
- Understanding spine surgery statistics is key for making informed choices.
- Different types of spine surgeries have unique success rates.
- A thorough pre-surgical check can lead to better results.
Understanding Spine Surgery: Types and Common Procedures

Spine surgery includes many procedures to treat different spinal issues. These surgeries help reduce pain, improve function, and enhance life quality for those with spinal problems.
We’ll look at spinal fusion, discectomy, laminectomy, and artificial disc replacement.
Spinal Fusion Procedures
Spinal fusion is a common surgery that joins two or more vertebrae. It treats issues like degenerative disc disease, spondylolisthesis, and spinal fractures. The surgeon uses bone grafts, rods, and screws to stabilize the spine and help new bone grow, joining the vertebrae.
Discectomy and Microdiscectomy
Discectomy and microdiscectomy relieve pressure on spinal nerves from herniated discs. A discectomy removes the herniated disc part. Microdiscectomy is a less invasive version, using a microscope or special tools to reduce tissue damage.
Laminectomy and Decompression
Laminectomy and decompression surgeries relieve pressure on the spinal cord or nerves. A laminectomy removes part or all of the lamina, a bony structure covering the spinal canal. Decompression surgery may also remove other tissues like bone spurs or ligaments that compress nerves.
Artificial Disc Replacement
Artificial disc replacement is a surgery that replaces a damaged or degenerative disc with an artificial one. It aims to keep spinal mobility and reduce pain, giving an alternative to spinal fusion for some patients.
Defining Success and Failure in Spine Surgery
To measure success, we look at many things.
Clinical Outcome Measures
Clinical measures are key to judging spine surgery success. These include:
- Neurological function improvement
- Pain reduction
- Restoration of spinal stability
A study in the Journal of Neurosurgery: Spine showed a strong link between these measures and patient happiness after surgery (1).
| Clinical Outcome Measure | Description | Importance |
| Neurological Function | Assessment of nerve root or spinal cord function | High |
| Pain Reduction | Measurement of pain levels pre- and post-surgery | High |
| Spinal Stability | Evaluation of spinal fusion or stabilization success | High |
Patient-Reported Outcome Measures
PROMs give us a glimpse into what patients feel and think after surgery. They include:
- Oswestry Disability Index (ODI)
- Visual Analog Scale (VAS) for pain
- Short Form-36 (SF-36) health survey
These measures help us see how surgery affects a patient’s life and well-being.
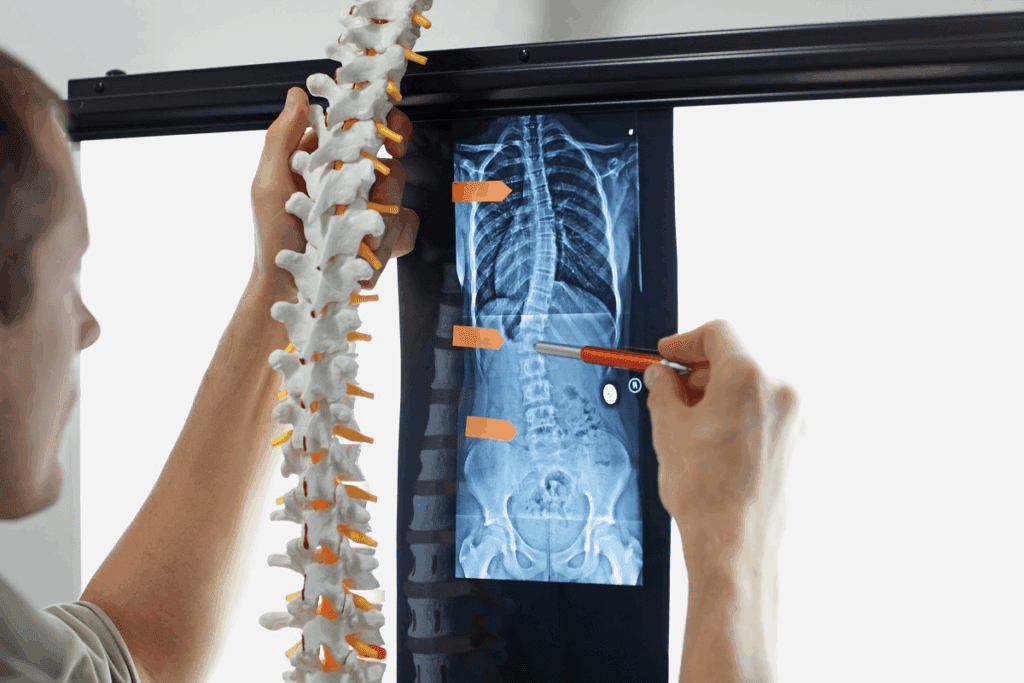
Radiographic Success vs. Symptomatic Relief
Radiographic success means the spine looks good on X-rays. But, this doesn’t always mean the patient feels better. Sometimes, patients don’t feel relief even if their spine looks fixed.
A study in the Spine Journal found that X-rays and patient feelings don’t always match (2).
The Failure Rate of Spine Surgery: Current Statistics
Recent studies have shed new light on the failure rates associated with various spine surgeries. Understanding these statistics is key for both patients and surgeons to make informed decisions.
Overall Success and Failure Percentages
The failure rate for spine surgery varies from 10% to 40%, depending on the procedure. For example, spinal fusion procedures have a higher failure rate than some other types of surgery.
The success of spine surgery depends on several factors. These include the type of procedure, the patient’s health, and the surgical technique. Studies show that while many patients see relief, a significant number may not get the results they hope for.
| Procedure Type | Average Success Rate | Average Failure Rate |
| Spinal Fusion | 70% | 30% |
| Discectomy | 85% | 15% |
| Laminectomy | 80% | 20% |
Variation by Procedure Type
Different spine surgery procedures have different success and failure rates. For example, discectomy and microdiscectomy tend to have lower failure rates than more complex procedures like spinal fusion.
The complexity and invasiveness of a procedure can greatly affect the outcome. Minimally invasive surgeries often have different success rates than traditional open surgeries.
Regional and Demographic Differences
Regional and demographic factors also play a big role in spine surgery outcomes. Studies show that outcomes can vary a lot based on age, overall health, and lifestyle.
For example, older patients or those with significant health issues may have higher failure rates. This is due to decreased bone density or other health problems.
Historical Trends in Outcomes
Historically, spine surgery outcomes have improved. This is thanks to advancements in surgical techniques, technology, and patient care. Yet, the failure rate remains a concern.
By looking at historical trends, we can better understand how outcomes have changed. This helps us identify areas for further improvement.
Failed Back Surgery Syndrome (FBSS): Definition and Prevalence
It’s important to know about Failed Back Surgery Syndrome (FBSS) for both patients and doctors. FBSS is when pain keeps coming back after spine surgery. This can really hurt a person’s quality of life.
Diagnostic Criteria for FBSS
To diagnose FBSS, doctors look at a patient’s symptoms, medical history, and past surgeries. The key signs include:
- Persistent or recurring pain after spine surgery
- Presence of radicular pain, axial pain, or a mix of both
- Failure to get better in daily activities
- Need for ongoing pain relief through medicine or other treatments
Incidence Rates Across Different Populations
FBSS happens in 10% to 40% of people who have spine surgery. The exact number can change based on many things. These include the surgery type, who gets chosen for surgery, and how doctors diagnose it.
For example, a study found more cases of FBSS in people who had surgery on their lower back before. Another study showed that those with mental health issues before surgery were more likely to get FBSS.
Economic and Quality of Life Impact
FBSS costs a lot, both directly and indirectly. Direct costs include more medical care and treatments. Indirect costs are things like lost work time.
Patients with FBSS often need ongoing pain care, physical therapy, and sometimes more surgery. These things add up in cost.
FBSS also affects a person’s life a lot. It can cause ongoing pain, make it hard to move, and lead to emotional and social problems. It’s key to manage FBSS well to help patients live better.
In summary, FBSS is a serious issue that needs a detailed approach to diagnose and treat. Knowing how common it is, how to spot it, and its effects on people’s lives is vital for better care.
Common Causes of Spine Surgery Failure
Understanding why spine surgery fails is key to better results. Failures can come from technical, patient, and biological reasons.
Technical and Surgical Factors
Technical and surgical mistakes are big reasons for failure. These include not fully relieving pressure or hardware not working right.
- Inadequate decompression or stabilization
- Instrumentation failure (e.g., hardware malfunction)
- Surgical technique errors
These problems can cause ongoing pain or nerve issues after surgery.
Patient Selection Issues
Choosing the right patient is vital for success. Problems include not screening patients well or ignoring health issues.
- Poor patient screening
- Inadequate consideration of patient comorbidities
- Unrealistic patient expectations
Biological Factors Affecting Healing
Biological factors are also important. These include bone quality, infections, and how well the bone fuses.
- Poor bone quality or density
- Infection or wound complications
- Inadequate fusion techniques
These can slow down healing and lead to failure.
Psychosocial Contributors
Psychosocial factors also play a part. These include mental health, social support, and lifestyle choices.
- Psychological distress or mental health issues
- Social support issues
- Lifestyle factors such as smoking or obesity
Working on these psychosocial issues can help improve surgery results.
| Cause Category | Specific Factors | Potential Impact |
| Technical and Surgical | Inadequate decompression, instrumentation failure | Continued pain, neurological deficits |
| Patient Selection | Poor screening, comorbidities, unrealistic expectations | Increased risk of complications |
| Biological | Poor bone quality, infection, inadequate fusion | Impaired healing, failure |
| Psychosocial | Psychological distress, social support issues, lifestyle factors | Poor recovery, dissatisfaction |
Procedure-Specific Failure Rates
It’s important to know how often spine surgery procedures fail. Different surgeries and patient health can affect success or failure.
Lumbar Fusion Failure Statistics
Lumbar fusion is a common spinal surgery. But, lumbar fusion failure rates can be quite different. They depend on the surgery method, who gets the surgery, and how well they recover.
“Choosing the right patient and using careful surgical techniques can help lower failure rates,” a study found.
Cervical Spine Surgery Outcomes
Cervical spine surgery outcomes are mostly good, with many patients feeling better. But, like any surgery, there are risks of problems and failure. Success rates are high, but failure can happen due to hardware issues or not enough decompression.
Minimally Invasive vs. Traditional Approaches
The choice between minimally invasive surgery and traditional surgery is ongoing. Minimally invasive methods are popular for less damage and faster recovery. But, success depends on the surgeon’s skill and the condition being treated.
- Minimally invasive surgery often means less blood loss and shorter hospital stays.
- Traditional surgery might be better for complex cases or when more is needed.
Revision Surgery Success Rates
Revision surgery is done to fix problems or failures from first surgeries. It’s harder than the first surgery because of scar tissue and changed spinal shape.
A study showed revision surgery success rates vary. They can be between 50% and 80%, depending on why the surgery is needed and the method used.
Early Complications Leading to Surgical Failure
It’s key to know about early complications to better the results of spine surgery. These issues happen right after surgery and can threaten the success of the operation. We’ll look at the early complications that can cause surgery to fail and what they mean.
Infection and Wound Complications
Infection is a big early complication that can make surgery fail. Post-operative infections can be simple skin infections or deeper infections affecting the hardware or bone. Quick action and treatment of these infections are vital to avoid long-term problems. We use antibiotics and careful wound care to lower the chance of infection.
Wound issues, like opening up or fluid buildup, can also harm the success of spine surgery. These problems can cause longer hospital stays, more surgeries, and higher costs. Good wound care strategies are key to reducing these risks.
Hardware Failure and Malposition
Hardware failure or being placed wrong is another early complication that can cause surgery to fail. This includes problems like screws being in the wrong spot, rods breaking, or cages moving. Putting hardware in the right place during surgery is very important to avoid these issues. We use advanced imaging and monitoring during surgery to place hardware accurately.
Neurological Complications
Neurological problems, like nerve damage, spinal cord injury, or cauda equina syndrome, can be very serious. These issues can cause ongoing pain, nerve problems, or even paralysis. Picking the right patients and being very careful during surgery are important to lower the risk of these complications.
Vascular Complications
Vascular problems, like bleeding or injury to blood vessels, can happen during or after spine surgery. These issues can be very dangerous if not treated right away. Watching patients closely after surgery is key to spotting and handling any vascular problems quickly.
By understanding and tackling these early complications, we can make spine surgery better and lower the chance of failure. It’s important for both patients and healthcare teams to know about these possible complications and work together to lessen their effects.
Long-Term Complications and Failure Mechanisms
It’s important to know about the long-term effects of spine surgery. This knowledge helps set realistic expectations and improves results. Complications can come from the surgery, the patient’s health, and how well they recover.
Adjacent Segment Disease
Adjacent segment disease (ASD) is a common issue after spinal fusion. It happens when the segments next to the fusion site wear out, causing new pain. Research shows ASD can affect up to 30% of patients within 5 years after surgery.
ASD is becoming more common as more people get older and have spinal fusion. The reasons for ASD are complex, involving both the body’s mechanics and the patient’s health.
Pseudarthrosis (Failed Fusion)
Pseudarthrosis, or failed fusion, is a serious complication. It happens when the bone doesn’t heal or fuse right after surgery. This can cause ongoing pain and might need more surgery.
The chance of pseudarthrosis depends on the type of fusion and the patient’s health. For example, smoking and some medical conditions can raise the risk a lot.
| Risk Factor | Impact on Pseudarthrosis |
| Smoking | Significantly increases risk |
| Diabetes | Moderately increases risk |
| Osteoporosis | Moderately increases risk |
Recurrent Disc Herniation
Recurrent disc herniation can happen after certain surgeries. It means the disc bulges again, often needing more surgery.
To lower the risk of this happening, the surgery must be done right and the patient must follow up care well. Things like being overweight or lifting too much can also play a part.
Chronic Pain Syndromes
Chronic pain can develop after spine surgery, even if it seems to go well. This can be due to nerve damage, ongoing inflammation, or psychological factors.
Dealing with chronic pain needs a team effort. This includes pain doctors, physical therapists, and sometimes psychologists. We stress the need for a detailed plan to meet these patients’ complex needs.
Patient Risk Factors for Spine Surgery Failure
Patient risk factors are key in spine surgery success. Knowing these factors helps improve care and outcomes.
Medical Comorbidities
Medical conditions like diabetes and hypertension raise surgery risks. Diabetes can slow wound healing, and hypertension may cause heart problems during surgery. Managing these conditions is vital before, during, and after surgery.
Psychological and Social Factors
Psychological and social factors are also important. Mental health issues, such as depression or anxiety, can affect surgery success. A strong support network can help with recovery. We evaluate these factors before surgery to meet each patient’s needs.
Smoking and Nutritional Status
Smoking is a major risk for spine surgery failure. It hinders bone healing and increases the chance of failed fusion. Good nutrition is also key for healing. We advise patients to quit smoking and eat well before surgery.
Age-Related Considerations
Age affects spine surgery outcomes. Older patients face more risks due to comorbidities, while younger patients have different concerns. We consider age when weighing surgery risks and benefits, aiming to reduce age-related risks.
Surgeon and Hospital Factors Affecting Outcomes
When it comes to spine surgery, the surgeon’s skill and the hospital’s quality are key. These factors work together to greatly impact the success of the surgery.
Surgeon Experience and Specialization
The surgeon’s experience and focus are vital for good spine surgery results. Research shows that surgeons who do many spine surgeries get better results. This is compared to those who do fewer.
Surgeon specialization is also important. It means the surgeon knows the latest methods and tools. This knowledge helps in better patient care and fewer complications.
Hospital Volume and Resources
The number of surgeries a hospital does also matters. Hospitals that do a lot of spine surgeries have better tools and staff. This leads to better care for patients.
| Hospital Volume | Complication Rate | Patient Satisfaction |
| High Volume | Lower | Higher |
| Low Volume | Higher | Lower |
Multidisciplinary Approach Benefits
Spine surgery benefits from a team effort. This means doctors from different fields work together. It ensures patients get all-around care, from before surgery to after.
This teamwork leads to happier patients, fewer problems, and faster recovery.
Technological Resources and Availability
Modern spine surgery needs the latest technology. Hospitals with the newest tools, like navigation systems and imaging, can do more precise surgeries.
By combining skilled surgeons, top-notch hospitals, teamwork, and cutting-edge tech, patients can get the best spine surgery results.
Diagnosing Failed Spine Surgery
Diagnosing failed spine surgery is complex. It involves many steps, including clinical and diagnostic methods. When spine surgery doesn’t work as hoped, finding the cause is key to fixing it.
Clinical Evaluation Approaches
First, we do a detailed clinical evaluation. This includes looking at the patient’s medical history, doing a physical exam, and checking their symptoms. We check their nerve function, pain levels, and how well they can move to see how bad the problem is.
Key components of clinical evaluation include:
- Patient history and symptom assessment
- Physical examination and neurological assessment
- Review of previous surgical records and imaging studies
Advanced Imaging Techniques
Advanced imaging is also very important. It helps us see what’s going on inside the spine. The main tools are:
- Magnetic Resonance Imaging (MRI): Shows soft tissues like nerves and discs in detail.
- Computed Tomography (CT) scans: Gives clear pictures of bones and can spot hardware problems.
- X-rays: Helps check if the spine is lined up right and if there are any hardware issues.
Diagnostic Injections and Tests
We also use injections and tests to confirm the diagnosis. These include:
- Selective nerve root blocks: Helps find out if a nerve is irritated.
- Facet joint injections: Checks for pain in the facet joints.
- Discography: Looks at pain coming from the discs.
These tests help us create a treatment plan that fits the patient’s needs.
| Diagnostic Method | Description | Clinical Utility |
| MRI | Detailed imaging of soft tissues | Assesses nerve compression, disc herniation |
| CT scans | High-resolution imaging of bony structures | Evaluates hardware failure, bony fusion |
| Diagnostic Injections | Injection of anesthetic or steroid into specific areas | Identifies pain generators, guides treatment |
Management Options for Failed Spine Surgery
Managing failed spine surgery needs a deep understanding of both surgical and non-surgical methods. When the first surgery doesn’t work, patients and doctors must explore many treatment options.
Conservative Management Strategies
First, doctors often try non-surgical treatments. These include:
- Physical therapy tailored to the patient’s specific needs
- Pain management through medication and lifestyle adjustments
- Alternative therapies such as acupuncture or chiropractic care
Experts say, “A team effort in pain management can greatly help patients.”
Pain is a complex issue that needs a detailed treatment plan by mixing different treatments, we can tackle pain’s many sides.
Interventional Pain Management
For those who don’t get better with non-surgical methods, doctors may try interventional pain management. This includes:
- Epidural steroid injections to reduce inflammation
- Facet joint injections for both diagnosis and treatment
- Radiofrequency ablation to block pain signals
A study in the Journal of Pain Research showed that “Epidural steroid injections greatly helped patients with failed back surgery syndrome.”
Revision Surgery: When and Why
Doctors consider revision surgery if the first surgery failed due to a clear reason, like faulty hardware or not enough decompression. They weigh the benefits and risks carefully before deciding.
| Indication for Revision | Description | Success Rate |
| Hardware Failure | Failure of implanted devices | 70-80% |
| Incomplete Decompression | Inadequate relief of nerve compression | 60-75% |
Emerging Therapies for Failed Spine Surgery
New treatments and technologies are always coming, giving hope to those with failed spine surgery. These include:
- Biologics and stem cell therapies to help healing
- Advanced neuromodulation techniques
- Minimally invasive surgical methods
As we look ahead, keeping up with these new options is key to giving patients the best care.
Preventing Spine Surgery Failure: Best Practices
Preventing spine surgery failure needs a detailed plan that starts before surgery. We focus on strategies that improve patient results and lower complication risks.
Preoperative Optimization Strategies
Getting ready for surgery is key to avoiding failure. Smoking cessation is important because smoking hinders healing and raises complication risks. Also, making sure patients are well-fed helps their bodies heal.
We also manage health issues and mental factors to help surgery go well. We tailor our care to meet each patient’s unique needs.
Surgical Planning and Technology
Using the latest in planning and technology is vital. 3D imaging and computer-assisted navigation make surgeries more precise, cutting down on risks.
Choosing the right surgery for each patient is also critical. We look at their health, condition, and lifestyle to pick the best option.
Postoperative Rehabilitation Protocols
After surgery, care is just as important. Our rehabilitation plans help patients fully recover and regain strength. This includes physical therapy, managing pain, and watching for complications.
We also stress the need for follow-up visits. This lets us track progress and quickly address any issues.
Patient Education and Expectation Management
Teaching patients about their surgery and recovery is essential. Clear information helps reduce anxiety and boosts satisfaction.
We explain the surgery’s risks and benefits clearly. This ensures patients are well-informed and ready for their recovery journey.
Conclusion: The Future of Spine Surgery Outcomes
Spine surgery is a complex field with many procedures and outcomes. The failure rate can be high, but new technology and techniques are on the horizon. These advancements promise to make outcomes better in the future.
Success in spine surgery depends on several factors. These include the surgeon’s experience, the hospital’s resources, and who gets surgery. By focusing on these areas and using new technologies, we can improve spine surgery’s future.
The future of spine surgery looks bright. Ongoing research aims to make patient outcomes even better. As we learn more, we can expect higher success rates and better lives for those undergoing surgery. This will lead to overall better outcomes.
FAQ
What is the average failure rate of spine surgery?
The failure rate of spine surgery varies. It depends on the procedure type, patient, and other factors. Studies show it ranges from 5% to 40%.
What are the most common reasons for spine surgery failure?
Spine surgery can fail for many reasons. Technical issues, wrong patient selection, and healing problems are common. Pseudarthrosis and disc herniation also play a big role.
How is success or failure determined in spine surgery?
Success or failure is judged by several measures. These include clinical outcomes, patient reports, and X-rays. They check for pain relief, better function, and complications.
What is Failed Back Surgery Syndrome (FBSS), and how common is it?
Failed Back Surgery Syndrome (FBSS) is chronic pain after spine surgery. It affects many patients, impacting their life and finances.
Can revision surgery improve outcomes for patients with failed initial spine surgery?
Revision surgery can help some patients. It offers better pain relief and function. But, success depends on the reason for failure and patient choice.
What are the risks associated with spine surgery?
Spine surgery has risks like infection and hardware failure. Knowing these risks helps make better decisions and care for patients.
How can patients minimize the risk of spine surgery failure?
To lower failure risk, optimize before surgery and plan carefully. Post-op care and education are key. Addressing risks like smoking is also important.
What role do surgeon experience and hospital volume play in spine surgery outcomes?
Surgeon experience and hospital volume matter a lot. High-volume centers and experienced surgeons have better results. They have fewer complications and happier patients.
Are there non-surgical alternatives for patients with failed spine surgery?
Yes, non-surgical options exist for failed spine surgery. These include conservative treatments and pain management. They help patients who don’t want or can’t have surgery.
What advancements are being made to improve spine surgery outcomes?
New tech, techniques, and care are making spine surgery better. Minimally invasive methods, better imaging, and rehab are some examples.
References
- Daniell, J. R. (2018). Failed Back Surgery Syndrome: A Review Article. PMC. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5913031/


































