Last Updated on November 27, 2025 by Bilal Hasdemir
The field of hernia surgery has seen significant advancements in recent years, with a growing focus on advanced hernia repair techniques that reduce recovery time and minimize pain.
One of the most popular methods is robotic-assisted surgery, which provides precision, smaller incisions, and faster recovery. Robotic surgery is becoming a preferred choice for hernia repair thanks to its many benefits.
The evolution of these advanced hernia repair techniques is transforming hernia surgery, offering patients more effective, efficient, and less invasive treatment options.
Hernias, though often perceived as a single condition, encompass a range of disorders that require distinct approaches to treatment. A comprehensive understanding of hernias is essential for determining the most appropriate course of action.
There are several common types of hernias, each with distinct characteristics. Inguinal hernias occur when tissue, such as part of the intestine, protrudes through a weak spot in the abdominal muscles in the groin area. Ventral hernias involve a bulge through the abdominal wall, often at the site of a previous surgical incision. Hiatal hernias occur when the stomach bulges up into the chest through an opening in the diaphragm.
Other less common types include umbilical hernias, which occur near the belly button, and incisional hernias, which develop at the site of a previous surgical scar. Each type of hernia has its specific causes and risk factors.
The causes of hernias are multifactorial, involving a combination of genetic predisposition, lifestyle factors, and certain medical conditions. Age is a significant risk factor, as hernias are more common in older adults due to the natural weakening of muscles over time. Obesity and chronic coughing can also increase the risk by putting additional strain on the abdominal muscles.
A family history of hernias can also play a role, suggesting a genetic component to the condition. Additionally, certain activities that involve heavy lifting or straining can increase the risk of developing a hernia.
“The risk factors for hernias are diverse, and understanding these can help in preventing the condition or identifying it early.”A General Surgeon
Not all hernias require surgical intervention, but surgery becomes necessary when the hernia is large, symptomatic, or at risk of complications such as incarceration or strangulation. Incarceration occurs when the hernia becomes trapped and cannot be pushed back into the abdomen, while strangulation is a more severe condition where the blood supply to the herniated tissue is cut off.
The decision to undergo surgery is typically made on a case-by-case basis, taking into account the type of hernia, the patient’s overall health, and the severity of symptoms. Minimally invasive surgical techniques have become increasingly popular for hernia repair due to their benefits, including shorter recovery times and less postoperative pain.
The treatment of hernias has undergone significant transformations over the years, driven by advances in medical technology and surgical techniques. This evolution has been crucial in improving patient outcomes, reducing recovery times, and minimizing complications.
Hernia repair has a long history that dates back to ancient civilizations, with evidence of hernia treatment found in the works of Greek and Roman physicians. Initially, treatments were largely palliative, focusing on managing symptoms rather than addressing the underlying condition. The development of surgical techniques marked a significant turning point, with early attempts at hernia repair being fraught with complications due to limited understanding of anatomy and the absence of antiseptic practices.
The modern era of hernia surgery began to take shape in the late 19th and early 20th centuries with the introduction of aseptic techniques and the development of more sophisticated surgical methods. The mid-20th century saw the establishment of tension-free repair techniques, which significantly improved outcomes.
Traditional open repair, once the standard for hernia surgery, involves making a significant incision to access the hernia directly. While effective, this method has several drawbacks, including longer recovery times, more postoperative pain, and a higher risk of wound complications. The large incision required for open repair can also lead to a more noticeable scar and potentially longer hospital stays.
A comparison of traditional open repair with modern techniques highlights the limitations of older methods. The table below summarizes key differences:
| Aspect | Traditional Open Repair | Modern Minimally Invasive Techniques |
| Recovery Time | Longer, often several weeks | Shorter, typically a few days to a week |
| Postoperative Pain | More significant | Less significant |
| Scarring | More noticeable scarring | Less noticeable, smaller incisions |
| Complications | Higher risk of wound complications | Lower risk of complications |
The advent of laparoscopic surgery marked a significant shift in hernia repair, offering a less invasive alternative to traditional open repair. Minimally invasive techniques, including laparoscopic and robotic-assisted surgery, have become increasingly popular due to their benefits, such as reduced postoperative pain, less scarring, and quicker recovery times.
The shift towards minimally invasive techniques represents a critical evolution in hernia surgery, driven by the desire to improve patient outcomes and enhance the overall quality of care. As technology continues to advance, it is likely that hernia repair techniques will continue to evolve, offering even better results for patients.
The landscape of hernia repair has undergone significant transformation with the advent of advanced techniques. Modern hernia surgery now encompasses a range of innovative approaches designed to improve patient outcomes and reduce recovery times.
Modern hernia surgery is guided by several key principles, including minimal invasiveness, the use of advanced materials such as mesh, and a focus on reducing recurrence rates. Surgeons now prioritize techniques that minimize tissue trauma and promote faster healing.
Minimally invasive techniques have become the cornerstone of modern hernia repair. These approaches reduce the size of incisions, leading to less tissue damage and quicker recovery times for patients.
Contemporary hernia repair techniques can be broadly classified into several categories, including laparoscopic, robotic-assisted, and open repair with advanced mesh technologies.
| Technique | Description | Benefits |
| Laparoscopic Repair | Minimally invasive surgery using a laparoscope | Smaller incisions, less pain, quicker recovery |
| Robotic-Assisted Repair | Use of robotic systems for enhanced precision | Improved visualization, enhanced dexterity |
| Open Repair with Mesh | Traditional open surgery with mesh reinforcement | Strong reinforcement, reduced recurrence rates |
The selection of hernia repair technique is increasingly guided by evidence-based practices. Surgeons consider factors such as the type and size of the hernia, patient health, and previous surgical history.
“The choice of technique should be tailored to the individual patient, taking into account the specific characteristics of the hernia and the patient’s overall health status.”
— Expert Opinion on Hernia Repair
Studies have shown that laparoscopic techniques result in less postoperative pain and quicker return to normal activities compared to open repair. However, the choice between laparoscopic and open repair should be based on individual patient factors and surgeon expertise.
As hernia repair continues to evolve, the integration of new technologies and techniques is expected to further improve outcomes. The use of advanced mesh materials and robotic-assisted surgery represents a significant step forward in the field.
With its reduced recovery time and less postoperative pain, laparoscopic hernia repair is gaining popularity among patients and surgeons alike. This technique has revolutionized the field of hernia surgery, offering a less invasive alternative to traditional open repair.
Laparoscopic hernia repair is primarily performed using two techniques: Transabdominal Preperitoneal (TAPP) and Totally Extraperitoneal (TEP). TAPP involves entering the abdominal cavity to access the hernia, whereas TEP is performed without entering the abdominal cavity, instead working around it to repair the hernia.
The choice between TAPP and TEP depends on various factors, including the surgeon’s expertise and the patient’s specific condition. Both techniques have their advantages and are selected based on the individual case.
Laparoscopic hernia repair offers several benefits, including:
These advantages make laparoscopic hernia repair an attractive option for many patients. The minimally invasive nature of the procedure contributes to a quicker return to normal activities.
Not all patients are suitable candidates for laparoscopic hernia repair. The selection criteria include:
| Criteria | Description |
| Hernia Type | The type and size of the hernia are critical in determining the suitability of laparoscopic repair. |
| Patient Health | Overall health and presence of any comorbidities are considered. |
| Surgeon Expertise | The experience and skill of the surgeon in performing laparoscopic hernia repair. |
By carefully evaluating these factors, surgeons can determine the most appropriate approach for each patient, ensuring the best possible outcomes.
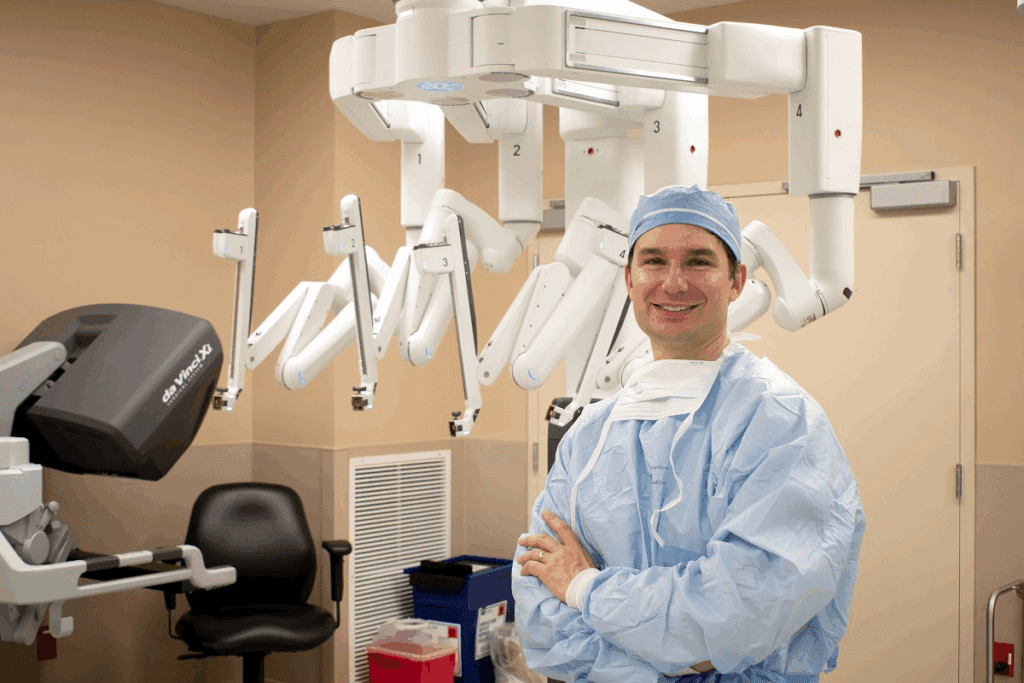
Robotic-assisted hernia surgery is revolutionizing the way hernias are treated. This advanced technique has emerged as a significant improvement over traditional methods, offering patients a more precise and minimally invasive option.
The da Vinci Surgical System is a leading robotic platform used in hernia repair. It enables surgeons to perform complex procedures with enhanced dexterity and visualization. Key features include:
Robotic-assisted hernia surgery provides surgeons with the ability to maneuver instruments with greater precision. The enhanced visualization offered by systems like the da Vinci Surgical System allows for a clearer view of the surgical site, potentially reducing complications.
Both robotic and laparoscopic hernia repair techniques are minimally invasive, but they differ in their approach. A comparison of the two is presented in the following table:
| Feature | Robotic-Assisted | Laparoscopic |
| Precision | Enhanced | Good |
| Visualization | High-definition 3D | 2D or 3D |
| Cost | Higher | Lower |
While robotic-assisted hernia surgery offers several benefits, it also comes with higher costs compared to traditional laparoscopic surgery. Additionally, surgeons must undergo specialized training to master the robotic technique, which can be a significant factor in its adoption.
The future of hernia repair is likely to be shaped by advancements in robotic technology, potentially making it more accessible and cost-effective.
Modern mesh technologies have revolutionized hernia repair, offering a range of options for surgeons. The choice of mesh material and fixation technique plays a crucial role in the success of the procedure.
The debate between synthetic and biologic mesh materials continues, with each having its advantages and disadvantages. Synthetic meshes are made from materials such as polypropylene, polyester, or polytetrafluoroethylene (PTFE), and are known for their durability and resistance to infection.
Biologic meshes, on the other hand, are derived from animal or human tissue and are designed to be absorbed by the body over time. They are often used in contaminated or infected fields where synthetic mesh may be contraindicated.
In addition to synthetic and biologic meshes, there are also absorbable and composite mesh options available. Absorbable meshes are designed to degrade over time, reducing the risk of long-term complications.
The method of mesh fixation is critical to prevent mesh migration and ensure a successful repair. Various techniques are employed, including sutures, staples, and adhesives.
Despite advancements in mesh technology, complications can still occur. These include mesh infection, adhesion formation, and chronic pain.
Management strategies involve a combination of conservative and surgical approaches, depending on the nature and severity of the complication.
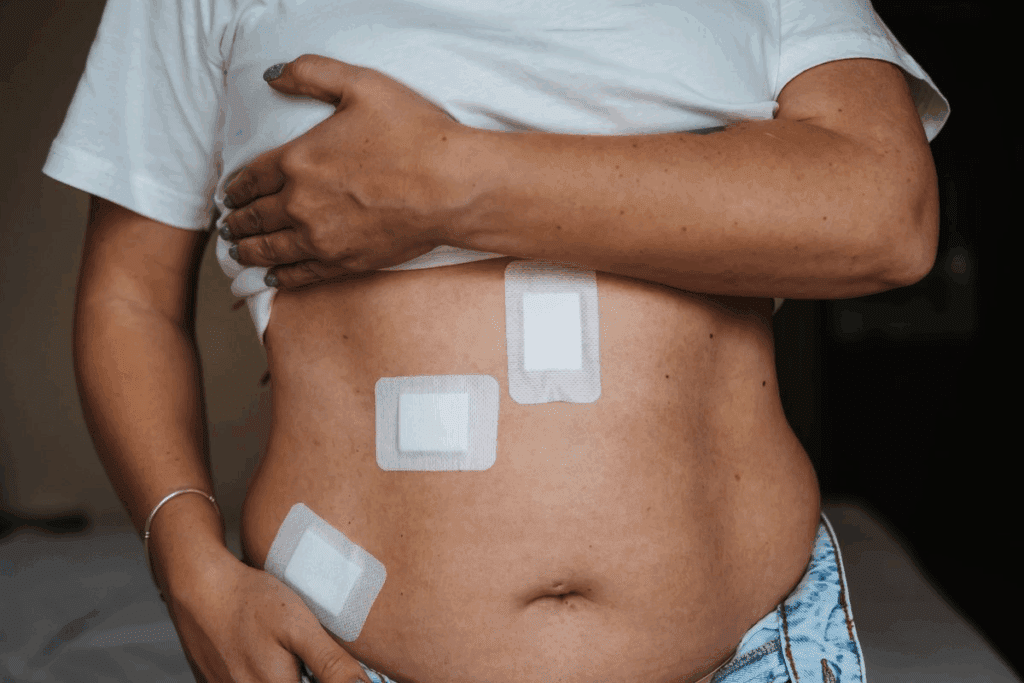
The latest innovation in minimally invasive surgery, SILS, is transforming the approach to hernia treatment. This technique involves performing hernia repair through a single incision, typically in the navel, thereby reducing visible scarring.
SILS for hernia repair involves the use of specialized laparoscopic instruments and a laparoscope with a high-definition camera. The procedure begins with a small incision, through which a port is inserted to allow the introduction of the laparoscope and surgical instruments.
Key Steps in SILS:
SILS requires specialized instruments that are curved or articulated, allowing for greater maneuverability within the limited space. Access ports designed for SILS enable the introduction of multiple instruments through a single incision.
The primary cosmetic benefit of SILS is the reduction of visible scarring to a single, small incision, often hidden within the navel. However, SILS can be technically challenging and may not be suitable for all patients or types of hernias.
Studies have shown that SILS for hernia repair is safe and effective, with outcomes comparable to traditional laparoscopic techniques. The cosmetic benefits and potentially less postoperative pain are significant advantages.
| Outcome | SILS | Traditional Laparoscopic |
| Cosmetic Satisfaction | High | Moderate |
| Postoperative Pain | Less | Moderate |
| Recovery Time | Faster | Faster |
The Enhanced-View Totally Extraperitoneal (eTEP) technique represents a significant advancement in minimally invasive hernia repair. This approach has garnered attention for its potential to improve surgical outcomes, particularly for complex hernias.
The eTEP technique involves a totally extraperitoneal approach, which means that the surgery is performed outside the peritoneal cavity. This method allows for reduced risk of intra-abdominal complications and promotes a faster recovery. The enhanced visualization provided by this technique enables surgeons to precisely identify and repair hernias, even in challenging cases.
The eTEP technique is particularly beneficial for patients with complex or recurrent hernias. Its minimally invasive nature and enhanced visualization capabilities make it an attractive option for surgeons dealing with difficult cases. By utilizing the eTEP technique, surgeons can potentially achieve better outcomes and lower recurrence rates.
While the eTEP technique offers several advantages, it also presents certain technical challenges. Surgeons must be experienced in laparoscopic surgery and familiar with the specific instrumentation required for eTEP procedures. Proper patient selection is crucial, as is meticulous technique, to minimize the risk of complications.
Emerging evidence supports the efficacy of the eTEP technique in hernia repair. Studies have shown promising results in terms of reduced postoperative pain, shorter hospital stays, and faster return to normal activities. As the technique continues to evolve, ongoing research will be essential to fully establish its benefits and potential limitations.
Component separation techniques have revolutionized the approach to repairing complex ventral hernias. These techniques involve separating the layers of the abdominal wall to facilitate closure of large defects without tension.
Anterior component separation is a traditional method that involves releasing the external oblique aponeurosis to allow for medial mobilization of the rectus abdominis muscle. This technique enables significant advancement of the abdominal wall, facilitating closure of large ventral hernias.
Posterior component separation, on the other hand, involves releasing the posterior rectus sheath, providing an alternative to anterior release. This method can be particularly useful in cases where anterior access is limited or when additional mesh placement is required.
Endoscopic component separation represents a minimally invasive evolution of the traditional component separation technique. By utilizing endoscopic instruments, surgeons can achieve the necessary release with smaller incisions, potentially reducing morbidity and recovery time.
For particularly large or complex defects, hybrid approaches combining different component separation techniques may be employed. These tailored strategies allow surgeons to address challenging cases more effectively, optimizing outcomes for patients with complex ventral hernias.
| Technique | Description | Advantages |
| Anterior Component Separation | Release of external oblique aponeurosis | Significant advancement of abdominal wall |
| Posterior Component Separation | Release of posterior rectus sheath | Alternative to anterior release, useful for additional mesh placement |
| Endoscopic Component Separation | Minimally invasive release using endoscopic instruments | Reduced morbidity and recovery time |
| Hybrid Approaches | Combination of different component separation techniques | Tailored strategies for complex defects, optimized outcomes |
Tailored hernia repair approaches have become the norm, offering patients more effective and personalized treatment options. Different types of hernias require distinct repair methods, and recent innovations have improved treatment outcomes.
Inguinal hernia repair has seen significant advancements, with techniques such as laparoscopic and robotic-assisted surgery improving recovery times and reducing complications. Laparoscopic inguinal hernia repair involves minimal invasion, leading to less postoperative pain and quicker return to normal activities.
Ventral and incisional hernias present unique challenges, but advanced techniques such as component separation and the use of biologic mesh have improved outcomes. Component separation techniques allow for the closure of large defects without excessive tension, reducing the risk of recurrence.
| Hernia Type | Repair Technique | Benefits |
| Inguinal Hernia | Laparoscopic Repair | Less postoperative pain, quicker recovery |
| Ventral/Incisional Hernia | Component Separation | Closure of large defects, reduced recurrence |
| Hiatal Hernia | Laparoscopic Nissen Fundoplication | Effective reflux control, minimal invasion |
Hiatal and parastomal hernias require specialized techniques. Laparoscopic Nissen fundoplication is a common approach for hiatal hernias, offering effective reflux control. Parastomal hernias can be managed with techniques such as Sugarbaker repair or stoma relocation.
Pediatric hernia repair has evolved with the adoption of laparoscopic techniques, which offer smaller incisions and less postoperative pain. Pediatric laparoscopic hernia repair is particularly beneficial for young patients, promoting faster recovery and improved cosmetic outcomes.
Comparing traditional and modern hernia repair techniques reveals substantial differences in outcomes. The latest techniques have shown significant improvements in various aspects, including recurrence rates, pain management, cost-effectiveness, and recovery times.
Studies have consistently shown that modern hernia repair techniques have lower recurrence rates compared to traditional methods. The use of advanced mesh materials and improved surgical techniques has contributed to this reduction. For instance, laparoscopic hernia repair has been associated with fewer recurrences due to its minimally invasive nature and enhanced visualization.
Pain management has also seen significant advancements with modern hernia repair techniques. Laparoscopic and robotic-assisted surgeries tend to result in less postoperative pain and quicker recovery times, improving overall quality of life for patients. Enhanced pain management strategies and protocols further contribute to better patient outcomes.
While initial costs for modern hernia repair techniques may be higher due to the use of advanced technology and materials, long-term cost-effectiveness is often improved. Reduced recovery times and lower recurrence rates translate into fewer additional surgeries and less time off work, ultimately benefiting both patients and healthcare systems.
Recovery times have decreased significantly with the advent of modern hernia repair techniques. Patients undergoing laparoscopic or robotic-assisted hernia repair typically experience shorter hospital stays and quicker returns to normal activities compared to those undergoing traditional open repair. This rapid recovery is a significant advantage for patients with demanding lifestyles or work commitments.
Patient recovery after advanced hernia procedures is a complex process that benefits from modern protocols. The journey to full recovery involves several key components, including Enhanced Recovery After Surgery (ERAS) protocols, effective pain management strategies, a gradual return to normal activities, and careful long-term follow-up.
ERAS protocols are a cornerstone of modern surgical care, designed to reduce postoperative complications and accelerate recovery. For hernia patients, these protocols typically include preoperative counseling, optimization of nutrition, standardized analgesic and anesthetic regimens, and early mobilization.
The implementation of ERAS protocols has been shown to significantly reduce hospital stay and improve patient outcomes. By minimizing surgical stress and managing pain effectively, patients are able to recover more quickly and return to their normal activities.
Effective pain management is crucial for a smooth recovery. Advanced hernia repair techniques often result in less postoperative pain, but a comprehensive pain management plan is still essential. This may include a combination of pharmacological interventions, such as multimodal analgesia, and non-pharmacological approaches, like early mobilization and physical therapy.
Pain management strategies should be tailored to the individual patient’s needs and the specifics of their surgery. By controlling pain effectively, patients are more likely to participate in early mobilization and rehabilitation, further enhancing their recovery.
The timeline for returning to normal activities after hernia surgery varies depending on the surgical technique used and the individual patient’s health status. Generally, patients who undergo minimally invasive procedures can expect a faster return to normal activities compared to those who have open surgery.
A gradual return to normal activities is recommended, with patients typically advised to avoid heavy lifting and strenuous exercise for several weeks postoperatively. A well-structured rehabilitation plan can help patients safely resume their usual activities.
Long-term follow-up after hernia repair is important for monitoring recurrence and addressing any late complications. Patients are usually followed up at regular intervals postoperatively, with the frequency of follow-up visits determined by the complexity of their surgery and their individual risk factors.
| Follow-Up Aspect | Importance | Timeline |
| Monitoring for Recurrence | High | Regular intervals up to 5 years |
| Managing Late Complications | High | Ongoing |
| Assessing Quality of Life | Medium | At 1, 3, and 5 years post-op |
By understanding the recovery process and adhering to a well-structured follow-up plan, patients can achieve optimal outcomes after advanced hernia procedures.
Selecting the right technique for hernia repair involves a nuanced understanding of both patient-specific factors and hernia characteristics. This personalized approach ensures that patients receive the most appropriate treatment for their unique condition, enhancing the likelihood of a successful outcome.
When considering hernia repair, patient-specific factors play a crucial role in determining the most suitable technique. These factors include the patient’s overall health, age, lifestyle, and previous surgical history. For instance, a patient with a history of multiple abdominal surgeries may require a more complex approach, such as component separation techniques, to address the hernia effectively.
The characteristics and complexity of the hernia itself are also critical in selecting the appropriate repair technique. Factors such as the size, location, and type of hernia can significantly influence the choice of surgery.
A shared decision-making process between the patient and the surgeon is essential in personalized hernia care. This collaborative approach ensures that the chosen technique aligns with the patient’s preferences, expectations, and lifestyle, while also meeting the surgeon’s professional judgment regarding the most effective treatment.
“The key to successful hernia repair lies in tailoring the treatment to the individual patient, taking into account their unique needs and circumstances.” –
A renowned hernia specialist
Specialized hernia centers play a vital role in providing personalized hernia care. These centers are equipped with state-of-the-art technology and staffed by experienced surgeons who are experts in the latest hernia repair techniques. By concentrating care in specialized centers, patients can benefit from a multidisciplinary approach that includes comprehensive evaluation, tailored treatment plans, and follow-up care.
In conclusion, personalized hernia care is a multifaceted approach that considers patient-specific factors, hernia characteristics, and the shared decision-making process. By leveraging the expertise of specialized hernia centers, patients can receive the most appropriate and effective treatment for their condition, leading to improved outcomes and quality of life.
The landscape of hernia surgery is on the cusp of a revolution, driven by technological advancements and innovative techniques. As we look to the future, it’s clear that hernia repair will continue to evolve, offering patients more effective and less invasive treatment options.
New techniques are being developed to improve the outcomes of hernia surgery. One such innovation is the use of robotic-assisted surgery, which enhances precision and allows for more complex repairs. According to recent studies, robotic hernia repair has shown promising results in reducing recurrence rates and improving patient recovery times.
“The integration of technology in hernia surgery has opened up new avenues for treatment,” says a leading hernia surgeon. “We’re seeing a shift towards more personalized and minimally invasive procedures.”
Artificial intelligence (AI) is beginning to play a significant role in surgical planning for hernia repair. AI algorithms can analyze patient data and imaging studies to help surgeons plan the most effective approach. This technology has the potential to improve outcomes by reducing complications and recurrence rates.
Tissue engineering is another area of research that holds promise for the future of hernia surgery. By developing biomaterials that can integrate with the body’s tissues, surgeons may be able to repair hernias more effectively and reduce the risk of complications.
Augmented reality (AR) is being explored for its potential to enhance surgical visualization during hernia repair. By overlaying digital information onto the surgical site, AR can help surgeons navigate complex anatomy and improve the accuracy of their repairs.
The future of hernia surgery is bright, with technological innovations set to transform the field. As these emerging techniques continue to evolve, patients can expect better outcomes and a faster return to normal activities.
The field of hernia repair is undergoing a significant transformation, driven by advancements in surgical techniques, mesh technologies, and a growing emphasis on minimally invasive approaches. As highlighted in the preceding sections, techniques such as laparoscopic and robotic-assisted hernia repair have revolutionized the field, offering patients reduced recovery times, less postoperative pain, and improved outcomes.
The changing landscape of hernia repair is characterized by a shift towards personalized care, with surgeons now able to tailor their approach to the specific needs of each patient. This personalized approach, combined with advancements in mesh technologies and surgical techniques, is set to continue shaping the future of hernia repair.
As the field continues to evolve, it is likely that we will see further innovations in hernia surgery, including the integration of artificial intelligence, tissue engineering, and augmented reality. These advancements will not only improve patient outcomes but also enhance the overall efficiency and effectiveness of hernia repair procedures, marking a new era in the treatment of hernias.
The latest techniques in hernia surgery focus on minimally invasive approaches, including robotic-assisted surgery and advanced mesh technologies, aiming to reduce recovery time, minimize pain, and improve outcomes.
Common types of hernias include inguinal, ventral, incisional, hiatal, and parastomal hernias, often caused by a combination of factors such as muscle weakness, strain, and genetic predisposition.
Hernia repair has shifted from traditional open repair to modern minimally invasive approaches, including laparoscopic and robotic-assisted techniques, offering reduced recovery time and improved outcomes.
Modern hernia surgery emphasizes minimally invasive techniques, advanced mesh technologies, and personalized care, with a focus on reducing recurrence rates, managing pain, and improving quality of life.
Laparoscopic hernia repair involves using a laparoscope to repair the hernia through small incisions, offering advantages such as reduced pain, faster recovery, and improved cosmetic outcomes.
The da Vinci Surgical System is a robotic-assisted surgical platform that enhances precision and visualization in hernia repair, offering benefits such as improved accuracy and reduced recovery time.
Mesh materials used in hernia repair include synthetic, biologic, absorbable, and composite meshes, each with its own characteristics, advantages, and potential complications.
SILS is a minimally invasive technique that involves repairing the hernia through a single incision, offering cosmetic benefits and potentially reduced recovery time.
eTEP is a laparoscopic technique used for hernia repair, offering enhanced visualization and potentially improved outcomes, particularly for complex hernias.
Component separation techniques involve separating the abdominal wall components to allow for tension-free closure of large defects, offering a solution for complex ventral hernias.
Latest hernia repair techniques, such as laparoscopic and robotic-assisted approaches, have been shown to offer improved outcomes, including reduced recurrence rates, pain, and recovery time, compared to traditional open repair.
ERAS protocols are standardized care pathways that aim to reduce perioperative stress, optimize pain management, and improve recovery outcomes in hernia repair patients.
Personalized care in hernia repair involves tailoring the treatment approach to individual patient factors, hernia characteristics, and complexity, through a shared decision-making process.
Emerging techniques and innovations in hernia surgery include artificial intelligence, tissue engineering, and augmented reality, which are expected to further improve outcomes and revolutionize the field.
Robotic-assisted hernia surgery offers enhanced precision, visualization, and dexterity, potentially improving outcomes and reducing recovery time, compared to laparoscopic approaches.
Mesh fixation techniques, such as suturing or stapling, play a crucial role in securing the mesh in place, reducing the risk of recurrence, and improving outcomes in hernia repair.
Cambridge University Hospitals NHS Foundation Trust – comprehensive patient information and surgical techniques overview
https://www.cuh.nhs.uk/patient-information/bladder-care-and-management
Medical News Today – detailed articles on hernia treatments, including robotic surgery advances
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!