Partial stomach removal is a key part of many bariatric surgeries done for weight loss. Did you know over 250,000 bariatric surgeries happen every year in the U.S.? Bariatric surgery is a big deal for those struggling with obesity.
Many think bariatric surgery changes the stomach — but what does that really mean? In most weight loss procedures, part of the stomach is either taken out or rearranged to help reduce food intake and promote weight loss.
In this section, we’ll dive into which part of the stomach is changed during obesity surgery and what these changes mean for patients.
Key Takeaways
- Bariatric surgery is a big step for weight loss.
- The stomach is the main organ changed in bariatric procedures.
- A part of the stomach is either removed or rearranged.
- Knowing the details helps in making smart choices.
- Bariatric surgery is often for those with obesity.
The Purpose and Evolution of Bariatric Surgery

Bariatric surgery has seen a lot of progress. This is thanks to new medical technology and a better understanding of obesity. Now, it’s a key treatment for those with severe obesity, helping when other methods don’t work.
Medical Indications for Weight Loss Surgery
Doctors suggest bariatric surgery for people with a high Body Mass Index (BMI). This includes a BMI of 40 or more, or 35 with serious health issues. These issues might be type 2 diabetes, high blood pressure, or sleep apnea.
Choosing surgery is a team decision. It’s based on the patient’s health, past weight loss efforts, and surgery’s benefits. Significant weight loss can improve health and lower death risks.
Development of Modern Bariatric Techniques
Modern bariatric surgery has changed a lot. Early surgeries were riskier and more invasive. But, new techniques and technology have made procedures safer and more effective.
Now, we have sleeve gastrectomy and gastric bypass surgery among the top choices. These advancements aim to reduce risks and boost weight loss and health benefits. There’s a focus on less invasive methods and better care after surgery.
Anatomy of the Digestive System in Bariatric Context
Bariatric surgery works by changing the digestive system’s anatomy. This system involves many organs, with the stomach and small intestine being key.
Structure and Function of the Stomach
The stomach is vital for digestion. It stores food and starts breaking it down. It has several important parts:
- The cardiac region where food comes from the esophagus.
- The fundus, a dome-shaped area for food storage.
- The body or corpus, where digestion starts.
- The pyloric region, which leads to the small intestine.
The stomach makes digestive enzymes and acids to break down food. Knowing the stomach’s anatomy is key for surgeries like sleeve gastrectomy.
Role of the Small Intestine in Digestion
The small intestine is also vital, mainly for nutrient absorption. It has a long, thin shape and:
- Has villi and microvilli to increase absorption area.
In gastric bypass surgery, the small intestine’s role is changed. This helps in weight loss.
It’s important to understand how the stomach and small intestine work together. Bariatric surgery changes these organs to help with weight loss.
Partial Stomach Removal: The Core of Most Bariatric Procedures
Partial stomach removal is key in many weight loss surgeries. The amount of stomach removed varies with each surgery. We’ll look at how much is taken out and how the remaining stomach works.
How Much Stomach Is Typically Removed
The amount of stomach removed can change based on the surgery. In a sleeve gastrectomy, a big part of the stomach is cut out, leaving a narrow tube. About 75-80% of the stomach is removed here. This reduces the stomach’s size, helping to control food intake and aid in weight loss.
In gastric bypass surgery, a smaller pouch is made from the stomach. The amount removed can vary, but the goal is the same: to reduce stomach size and help with weight loss.
Remaining Stomach Functionality
After removing part of the stomach, the remaining part works differently. It’s smaller, leading to earlier fullness and less hunger. This helps with managing weight. The stomach also keeps making digestive enzymes, but it can’t hold as much food.
It’s important to know that the stomach’s role in digestion doesn’t change much. Patients need to eat differently, focusing on nutrient-rich foods and smaller, more frequent meals.
The success of bariatric surgery also depends on how well patients adjust to these changes. Understanding what happens with partial stomach removal helps prepare for the lifestyle changes after surgery.
Sleeve Gastrectomy Explained
The gastric sleeve procedure removes a big part of the stomach. It leaves a narrow, sleeve-like stomach. This surgery is popular for its good results in weight loss and is simpler than other surgeries.
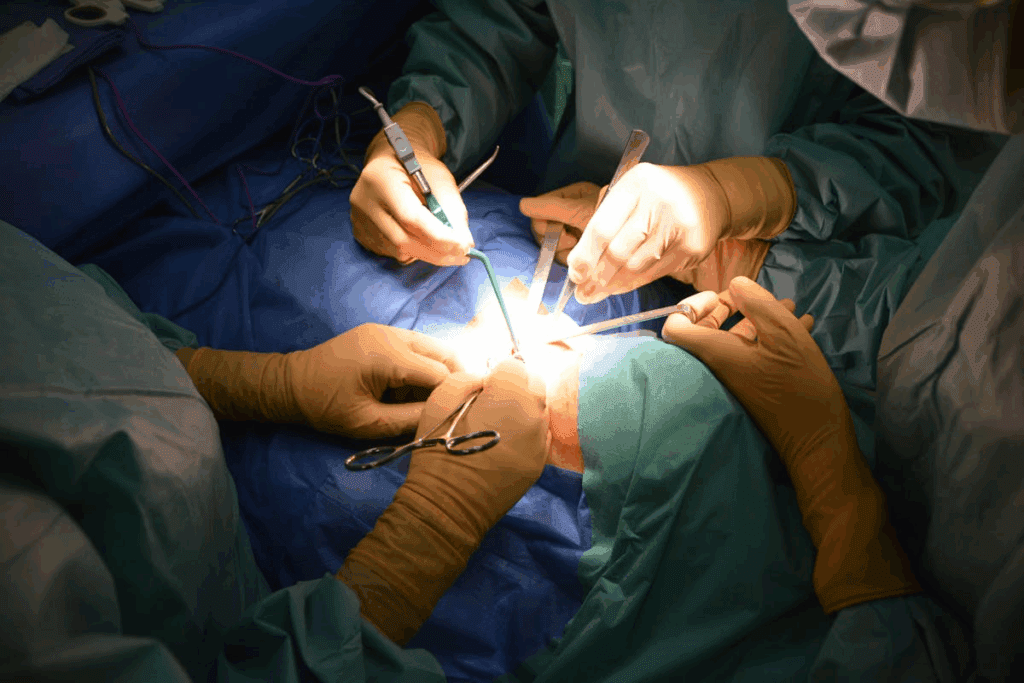
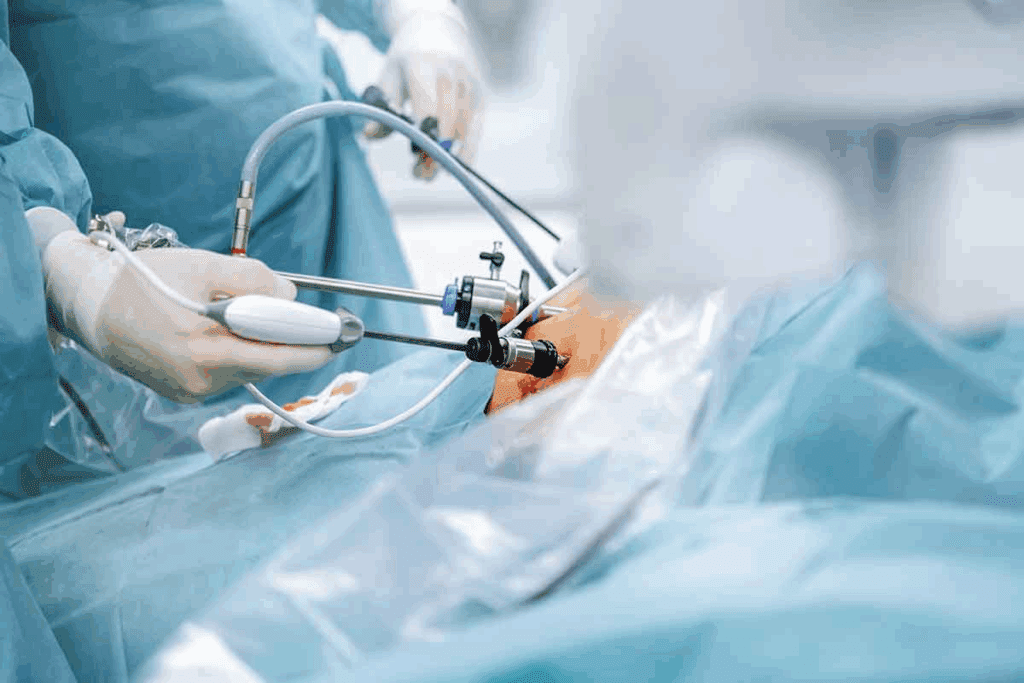
The Vertical Sleeve Procedure Step-by-Step
The surgery is done through small cuts in the belly. Here’s how it’s done:
- The surgeon makes small cuts in the belly to put in tools.
- A laparoscope helps see the stomach and around it.
- The stomach is separated from other tissues and organs.
- A big part of the stomach is taken out, leaving a narrow stomach.
- The remaining stomach is stapled to close it.
Permanent Nature of Stomach Tissue Removal
Removing stomach tissue is permanent in sleeve gastrectomy. This is different from some other surgeries, like adjustable gastric banding. Sleeve gastrectomy removes a big part of the stomach forever.
This means a few things:
- Patients must stick to diet changes and follow-up care for life.
- The risk of surgery problems is lower in the long run because there are no implants.
- Weight loss can be big and last a long time if the patient follows the recommended lifestyle changes.
| Aspect | Description | Implication |
| Permanence of Stomach Removal | Significant portion of the stomach is removed | Lifelong dietary adjustments necessary |
| Surgical Method | Laparoscopic procedure | Less invasive, quicker recovery |
| Weight Loss Outcome | Significant and sustained weight loss | Improved overall health and well-being |
Gastric Bypass: Rerouting Without Complete Removal
Gastric bypass surgery is a key bariatric procedure. It creates a small stomach pouch and reroutes the intestine. This helps people with obesity lose a lot of weight.
Creating the Small Stomach Pouch
The first step is making a small stomach pouch. The stomach is split into a small upper pouch and a larger lower pouch. The small pouch is then connected to the small intestine.
This reduction in stomach size helps limit food intake, leading to weight loss. The surgery is usually done laparoscopically, which means less recovery time.
Bypassing Portions of the Intestine
The next step is bypassing a part of the small intestine. The small stomach pouch is connected to a lower part of the small intestine. This skips the duodenum and a big part of the jejunum.
This rerouting reduces the absorption of calories and nutrients, helping with weight loss. It also changes how the body feels full or hungry.
Gastric bypass surgery has many benefits, including:
- Significant weight loss
- Improvement in obesity-related conditions
- Potential reduction in hunger due to hormonal changes
Understanding these points helps people decide if gastric bypass surgery is right for them. It’s important to weigh the benefits and risks. Also, long-term nutritional management is key.
Adjustable Gastric Banding: No Organ Removal Required
For those thinking about bariatric surgery, adjustable gastric banding is a good choice. It’s a reversible option that doesn’t remove the stomach. This method uses a band to make a small pouch in the stomach, limiting how much food you can eat.
Placement and Adjustment of the Band
The first step in adjustable gastric banding is to put a silicone band around the top of the stomach. This makes a small pouch above the band, which limits how much food you can eat. The band is connected to a port under the skin. This port lets us adjust the band after surgery.
We can add or remove saline solution through the port to change the band’s tightness. This lets us adjust the band to fit the patient’s needs and comfort level.
Adjustments are made during follow-up visits. We check the patient’s weight loss and adjust the band as needed. This flexibility helps us tailor the band’s tightness for better weight loss and fewer side effects.
Reversibility Advantages
One big plus of adjustable gastric banding is that it can be reversed. If needed, the band can be removed, returning the stomach to its original shape. This is great for patients who are unsure about more permanent surgery.
“The reversibility of adjustable gastric banding provides patients with a sense of security, knowing that they can revert to their original stomach anatomy if circumstances change or if the band is not tolerated.”
Being able to remove the band without lasting harm makes it a good choice for those looking for a less invasive surgery. We look at each patient’s health, weight loss goals, and past surgeries to see if they’re a good fit for this procedure.
Biliopancreatic Diversion with Duodenal Switch
The biliopancreatic diversion with duodenal switch is a complex surgery. It reduces stomach size and reroutes the intestines. This surgery is for those who want to lose a lot of weight and improve health.
Extensive Stomach Reduction Component
A big part of this surgery is the extensive stomach reduction. A large part of the stomach is removed, leaving a narrow stomach or “sleeve.” This limits how much food you can eat, helping with weight loss.
The stomach is made smaller by removing most of it, like in a sleeve gastrectomy. This makes you feel full faster and eat fewer calories.
Major Intestinal Rerouting
The duodenal switch also involves changing the intestines. The small intestine is split and reattached to bypass a big part of it. This reduces how much nutrients your body absorbs.
| Procedure Component | Description | Effect on Weight Loss |
| Stomach Reduction | Removal of a large portion of the stomach, leaving a narrow sleeve | Reduces food intake, leading to weight loss |
| Intestinal Rerouting | Rerouting of the small intestine to bypass a portion of the intestine | Reduces nutrient absorption, contributing to weight loss |
The extensive stomach reduction and major intestinal rerouting make this surgery very effective for weight loss. But, it’s a complex surgery that needs careful thought and monitoring because of its nutritional effects.
Single Anastomosis Procedures: Simplified Approaches
Single anastomosis procedures are changing bariatric surgery for the better. They make surgery simpler without losing the weight loss benefits. We’ll look at how these procedures work and their advantages, like one-anastomosis gastric bypass and SADI-S.
One-Anastomosis Gastric Bypass
One-anastomosis gastric bypass is a simpler take on traditional gastric bypass. It makes just one connection between the stomach and small intestine. This makes the surgery less complicated.
This method leads to big weight loss and better health for people with obesity. Patients often see their BMI drop and their type 2 diabetes improve.
SADI-S Procedure Mechanics
The SADI-S (Single Anastomosis Duodeno-Ileal Switch) procedure is another single anastomosis surgery. It starts with a sleeve gastrectomy and then connects the duodenum and ileum with one anastomosis.
The SADI-S procedure keeps the pylorus intact, which might lower the risk of some problems. It also makes the surgery easier than the traditional duodenal switch.
| Procedure | Key Features | Benefits |
| One-Anastomosis Gastric Bypass | Single anastomosis between stomach and small intestine | Simplified procedure, effective weight loss |
| SADI-S Procedure | Sleeve gastrectomy and single anastomosis between duodenum and ileum | Preserves pylorus, reduces risk of certain complications |
Organs That Remain Intact During Bariatric Surgery
Bariatric surgery changes the stomach a lot. But, it keeps other important digestive organs working. This is key for good digestion after surgery.
Preservation of Essential Digestive Organs
Bariatric surgery mainly changes the stomach and sometimes the intestines. But, important organs like the liver, pancreas, and gallbladder stay the same. They keep doing their jobs in digestion and nutrient absorption.
The liver makes bile, which helps digest fats. The pancreas makes digestive enzymes and insulin, which controls sugar levels. The gallbladder holds bile from the liver and releases it to help digest fats.
| Organ | Function | Post-Surgery Status |
| Liver | Bile production, detoxification | Remains intact |
| Pancreas | Digestive enzyme and hormone production | Remains intact |
| Gallbladder | Bile storage | Remains intact |
Debunking Common Misconceptions
Many think bariatric surgery removes or changes many organs. But, most surgeries aim to keep these organs working right.
Some think surgery causes malabsorption because it changes the intestines. But, the body adjusts, and with the right diet, patients can absorb nutrients well.
Knowing how bariatric surgery affects digestion can clear up worries. By keeping key organs intact, surgery aims to boost health without messing up digestion.
Hormonal and Metabolic Changes After Stomach Alteration
Changing the stomach through bariatric surgery brings big changes in hormones and how the body uses energy. These changes are key to why bariatric surgery works for losing weight and getting healthier.
Bariatric surgery makes big changes in hormones. It affects how we feel hungry and how well our body uses insulin.
Ghrelin Reduction and Appetite Control
Ghrelin is a hormone that makes us feel hungry. Bariatric surgery, like sleeve gastrectomy, lowers ghrelin levels. This makes us feel less hungry and helps control appetite.
With less ghrelin, people find it easier to stick to a healthy diet. This helps them lose weight.
Improved Insulin Sensitivity
Bariatric surgery also makes our bodies better at using insulin. Weight loss from surgery helps our bodies use insulin better. This lowers the risk of type 2 diabetes and helps control blood sugar in people with diabetes.
Improved insulin sensitivity comes from losing weight and the hormonal changes surgery causes. This leads to better health and a lower risk of metabolic syndrome.
In summary, the hormonal and metabolic changes after bariatric surgery are key to its success. They help people lose weight and improve their metabolic health. Understanding these changes shows how bariatric surgery offers many benefits.
Potential Complications of Gastric Resection
Gastric resection is a key part of bariatric surgery. It comes with various risks. Knowing these risks is important for those thinking about bariatric surgery.
Immediate Post-Surgical Risks
Right after gastric resection, patients face several risks. Bleeding and infection are big concerns. We watch patients closely for these signs to act fast.
Another risk is leakage from the staple line or anastomosis. This can cause serious infection and needs quick surgery. We are very careful during the surgery to avoid this.
Long-term Anatomical Issues
Long-term problems after gastric resection include stricture formation and gastric pouch dilation. These can impact the surgery’s success and the patient’s life quality.
We also worry about malnutrition because of changed digestion. Good nutrition is key to avoid this. Patients get advice on diet and supplements to get the nutrients they need.
Knowing these risks helps us manage patient care better. This improves outcomes after gastric resection in bariatric surgery.
Nutritional Management After Stomach Surgery
After stomach surgery, a good nutrition plan is key for health. Patients need to follow a special diet to get enough vitamins, minerals, and proteins.
Essential Vitamin and Mineral Supplementation
Patients often need supplements after surgery to avoid deficiencies. Vitamin B12 is a common issue because of less stomach acid and intrinsic factor. Regular checks and supplements are advised.
Other important nutrients like iron, calcium, and vitamin D are also needed. They help keep bones strong and prevent anemia. A doctor will suggest a plan based on your needs and surgery type.
“A well-balanced diet with appropriate supplementation is key to preventing nutritional deficiencies after bariatric surgery.” –
A leading bariatric surgeon
Protein Requirements and Absorption Challenges
Protein is vital for muscle and health after surgery. But, the body might have trouble absorbing it because of changes in the digestive system.
We suggest eating high-quality proteins like lean meats, fish, eggs, and dairy. Sometimes, protein shakes are needed to meet protein needs. Eating small meals often helps with absorption.
- Prioritize protein-rich foods
- Consider protein supplements if necessary
- Eat smaller, more frequent meals
Good nutrition helps patients stay healthy and enjoy the benefits of their surgery. Regular visits to healthcare providers are important to adjust the diet as needed.
Recovery Timeline Following Bariatric Procedures
Knowing the recovery timeline after bariatric surgery is key for a healthier life. The journey includes several stages. These range from the initial hospital stay to later phases of dietary changes.
Hospital Stay and Immediate Recovery
The recovery starts right after surgery. It usually takes 1 to 3 days in the hospital. Our team watches over patients for any immediate issues and helps manage pain.
After leaving the hospital, rest and avoid hard work. Following post-op instructions is vital for a smooth recovery. These include wound care, medication, and follow-up visits.
Dietary Progression Phases
The diet after surgery changes slowly. It helps the stomach heal while providing needed nutrients. The stages are:
- Liquid Diet: Patients start with clear broths, electrolyte drinks, and protein shakes.
- Pureed Diet: Next, they move to blended foods that are smooth.
- Soft Foods: Then, they eat soft foods like scrambled eggs and cooked veggies.
- Regular Diet: Last, they can eat a balanced diet, but must watch portion sizes.
| Dietary Phase | Duration | Food Examples |
| Liquid Diet | 1-2 weeks | Clear broths, protein shakes |
| Pureed Diet | 2-4 weeks | Blended soups, yogurt |
| Soft Foods | 4-6 weeks | Scrambled eggs, cooked vegetables |
| Regular Diet | After 6 weeks | Balanced meals with lean proteins, vegetables, and fruits |
Staying hydrated and following the diet plan is important. It helps avoid complications and ensures the best results.
Long-term Lifestyle Adaptations with Modified Digestive Anatomy
It is essential for patients to adjust their eating habits to accommodate their new digestive system.
Eating Behaviors and Food Choices
It is essential for patients to adjust their eating habits to accommodate their new digestive system. They should eat smaller, more frequent meals and choose foods rich in nutrients. Nutritional balance is essential to avoid deficiencies and stay healthy.
Significant dietary changes often include the following aspects:
- Incorporating high-protein foods is vital for maintaining muscle mass and overall health.
- It’s important to consume a diverse range of fruits and vegetables to ensure adequate intake of essential vitamins and minerals.
- Steering clear of foods that are high in calories, sugar, and fat is crucial for effective weight loss.
- Staying well-hydrated by drinking sufficient water is important for health and recovery.
“The key to successful weight loss after bariatric surgery is not just the procedure itself, but the lifestyle changes that follow.”
Physical Activity Requirements
Regular physical activity is also vital for keeping weight off and improving health. Exercise helps build muscle, increases metabolism, and boosts mental health.
| Activity Type | Frequency | Benefits |
| Cardio Exercises | 3-4 times a week | Improves heart health, burns calories |
| Strength Training | 2-3 times a week | Builds muscle, boosts metabolism |
| Flexibility Exercises | Daily | Enhances flexibility, reduces injury risk |
We suggest patients talk to their healthcare provider to create a personalized exercise plan. This plan should match their needs and abilities.
Selecting the Appropriate Bariatric Procedure
Choosing the right bariatric procedure is based on many factors. It’s important to think about your health needs, weight loss goals, and the risks of each surgery.
Medical Considerations and BMI Factors
Medical factors are key in picking the best surgery. Body Mass Index (BMI) is very important. It shows how severe obesity is and the health risks it brings.
People with a higher BMI might need more serious surgeries, like biliopancreatic diversion with duodenal switch. Those with a lower BMI might do better with less invasive options, like adjustable gastric banding.
Other health issues, like diabetes, high blood pressure, and sleep apnea, also matter. These can affect which surgery is safest and most effective for you. We look at all these factors to find the best surgery for you.
Personal Goals and Risk Assessment
Your personal weight loss goals are also important. Some people want to lose a lot of weight, while others want to improve their health. We listen to your goals and plan a treatment that fits you.
Understanding the risks of each surgery is also key. Each procedure has its own risks and might need more surgeries later. We help you understand these risks so you can make a good choice.
In summary, picking the right bariatric procedure involves looking at many things. We consider your health, BMI, goals, and risks. This way, we can help you reach your weight loss goals and improve your health.
Conclusion: The Transformative Impact of Bariatric Surgery
Bariatric surgery can change lives for those struggling with obesity. It offers a powerful solution. By learning about the different surgeries, people can make better choices for their weight loss journey.
This surgery does more than just help with weight. It improves health and happiness. It can make metabolism better, lower disease risks, and boost life quality.
Exploring different surgeries like sleeve gastrectomy and gastric bypass shows their unique benefits. The right surgery can lead to big weight loss and a major health improvement.
In the end, bariatric surgery is a strong tool against obesity. It can spark lasting change and a healthier life ahead.
FAQ
What is bariatric surgery and how does it help with weight loss?
Bariatric surgery changes the stomach to help people lose weight. It’s considered when other weight loss methods fail.
Which part of the stomach is removed during bariatric surgery?
The stomach part removed varies by procedure. In sleeve gastrectomy, a big part is removed, leaving a narrow stomach.
What is sleeve gastrectomy and how is it performed?
Sleeve gastrectomy removes a lot of the stomach, leaving a narrow one. It’s done laparoscopically, stapling and removing stomach tissue.
Is the stomach removal in bariatric surgery permanent?
Yes, in procedures like sleeve gastrectomy, stomach tissue removal is permanent. But, some procedures like adjustable gastric banding are reversible.
What are the possible complications of gastric resection in bariatric surgery?
Risks include bleeding and infection right after surgery. Long-term, there can be stomach obstruction or vitamin deficiencies.
How does bariatric surgery affect hormonal and metabolic changes?
It can lower ghrelin levels, helping control appetite. It also improves insulin sensitivity, helping with glucose metabolism.
What nutritional management is required after bariatric surgery?
Patients need to follow a specific diet. This includes taking vitamins and being careful about protein and absorption.
What is the recovery timeline following bariatric surgery?
Recovery starts with a hospital stay. Then, there are dietary phases and a return to normal activities with lifestyle changes.
How does bariatric surgery impact long-term lifestyle adaptations?
Patients must make lasting lifestyle changes. This includes new eating habits, food choices, and exercise levels to keep weight off.
How do I select the appropriate bariatric procedure for my needs?
Choosing the right procedure involves looking at medical needs, BMI, weight loss goals, and risk. A healthcare professional should help.
Are there any organs that remain intact during bariatric surgery?
Yes, important digestive organs stay the same during surgery. Keeping them intact is key for normal digestion.
What are single anastomosis procedures in bariatric surgery?
Single anastomosis procedures, like one-anastomosis gastric bypass, are simpler. They involve fewer connections between the stomach and intestine.
How does gastric bypass surgery work?
Gastric bypass surgery makes a small pouch from the stomach. It connects this pouch to the small intestine, bypassing parts of the digestive tract.
What is adjustable gastric banding and its advantages?
Adjustable gastric banding uses a band around the stomach to make a small pouch. It’s reversible and doesn’t remove stomach tissue.
What is biliopancreatic diversion with duodenal switch?
Biliopancreatic diversion with duodenal switch is a complex surgery. It reduces stomach size and reroutes the intestine significantly.
Reference
- Batsis, J. A., & Zagaria, A. B. (2018). Addressing Obesity in Aging Patients. Journal of the American Geriatrics Society, 66(2), 218–224. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5769212/
























