Last Updated on November 14, 2025 by Ugurkan Demir
At Liv Hospital, we know how complex Anemia of Chronic Disease Treatment (ACD) is. It’s linked to many chronic illnesses like infections, autoimmune diseases, cancers, and kidney problems. Many patients also wonder how long are cat scans, especially when imaging is needed to diagnose the underlying conditions that contribute to anemia.
ACD is the second most common anemia globally. It’s key to understand how to diagnose and treat it. Advanced lab tests and a patient-centered approach are needed for accurate diagnosis and effective treatment.
Our care plans are designed to give top-notch management for this complex condition. We tailor our care to meet the unique needs of each patient.
Anemia of Chronic Disease (ACD) is a condition where chronic inflammation and disease reduce healthy red blood cells. This often leads to mild to moderate anemia. Understanding ACD involves knowing its definition, how common it is, and the chronic conditions that cause it.
ACD happens when patients with chronic diseases, like infections or cancer, have fewer red blood cells. The number of people with ACD depends on the disease and the group being studied. It’s a common problem in chronic disease patients, affecting their quality of life and health outcomes.
| Chronic Condition | Prevalence of ACD |
| Chronic Kidney Disease | 30-50% |
| Rheumatoid Arthritis | 20-40% |
| Cancer | 30-90% |
ACD is linked to many chronic conditions, including infections, autoimmune diseases, and cancers. These conditions cause chronic inflammation. This inflammation messes with iron and red blood cell production, causing anemia.
Common chronic conditions associated with ACD include:
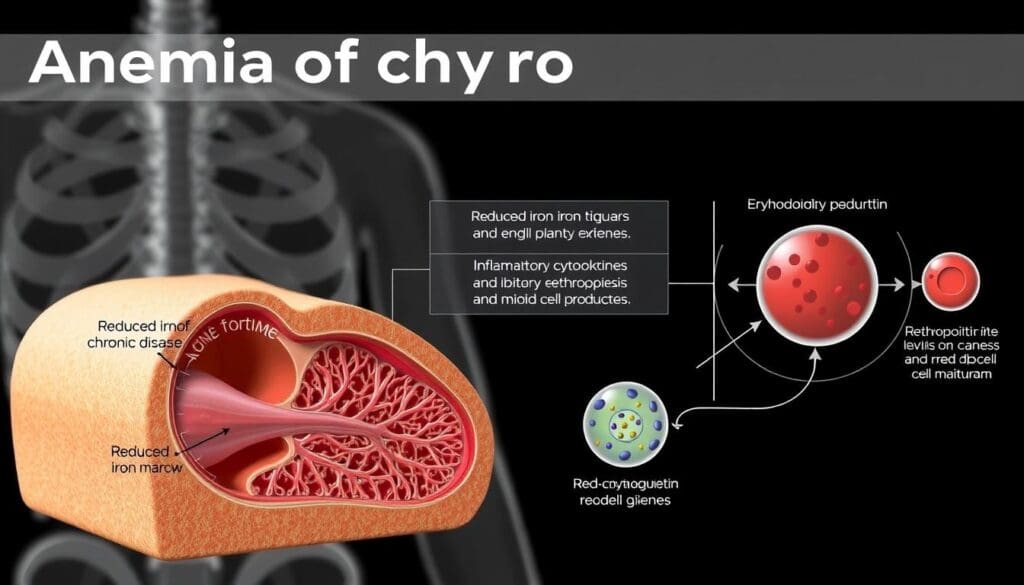
The cause of ACD involves complex interactions between cytokines, hepcidin, and iron. Chronic inflammation boosts cytokine production, which increases hepcidin. Hepcidin stops iron from being released from macrophages, making less iron available for red blood cell production and causing anemia.
The key mechanisms involved in the pathophysiology of ACD include:
The diagnosis of Anemia of Chronic Disease depends on lab tests. These tests show how hemoglobin and red blood cells are affected. They help doctors understand the severity of the anemia.
People with Anemia of Chronic Disease often have mild to moderate hemoglobin reduction. The National Institute of Diabetes and Digestive and Kidney Diseases says this is a key sign. It shows how the body reacts to long-term inflammation.
The level of hemoglobin is very important. In ACD, it’s not as low as in other anemias, like iron deficiency anemia.
A decreased reticulocyte count is also seen in ACD. Reticulocytes are young red blood cells. Their count shows how well the bone marrow is making red blood cells. A low count means the bone marrow isn’t making enough.
This happens because inflammation affects how red blood cells are made.
In ACD, red cell morphology changes are common. These changes can be seen in a blood smear test. They show how different red blood cells are in size and shape.
While these changes aren’t unique to ACD, they’re important. They help doctors understand the cause of anemia and make a diagnosis.
Anemia of Chronic Disease (ACD) is diagnosed by looking at iron panel results. This includes serum iron, transferrin, and ferritin levels. These changes help us understand ACD and how to treat it.
In ACD, the body has low serum iron. This happens because of inflammation, which messes with iron use. Low serum iron makes it hard for the body to make red blood cells.
Transferrin and Total Iron Binding Capacity (TIBC) are often lower in ACD. This is different from iron deficiency anemia, where TIBC goes up. The drop in transferrin and TIBC shows how inflammation affects iron use.
Ferritin, which stores iron, is usually normal or high in ACD. This is because ferritin goes up with inflammation. High ferritin levels, along with low serum iron and transferrin, help tell ACD apart from iron deficiency anemia.
In Anemia of Chronic Disease, hepcidin is a key player. It controls iron absorption and recycling. Its imbalance is linked to anemia in chronic diseases.
In ACD, hepcidin levels are often high. This is mainly because of chronic inflammation. This inflammation is common in many diseases that cause ACD.
High hepcidin levels mean less iron for making red blood cells. This leads to anemia.
The rise in hepcidin is caused by inflammation and cytokines like IL-6. This connection is key to understanding ACD.
Hepcidin affects iron metabolism in many ways. It binds to ferroportin, causing it to be broken down. This reduces iron release from cells.
This action lowers serum iron levels, a sign of ACD. Hepcidin also impacts iron recycling from macrophages. This further limits iron for making red blood cells.
Hepcidin is being studied as a diagnostic tool for ACD. Its levels can help tell ACD apart from other anemias.
Measuring hepcidin shows promise. But more research is needed. We need to standardize tests and find clear values for use in clinics.
Managing anemia of chronic disease (ACD) needs a detailed plan. It must tackle the root cause of the condition. ACD often comes with chronic diseases like rheumatoid arthritis, chronic kidney disease, and cancer. A good treatment plan should handle both the anemia and the chronic disease causing it.
The first step is to treat the chronic disease causing ACD. This can involve different treatments based on the disease. For example, in rheumatoid arthritis, using DMARDs can help reduce inflammation and possibly improve anemia.
Iron supplements are key in treating ACD, mainly when iron deficiency is a problem. But, iron absorption can be tough due to hepcidin. We’ll look at different iron supplement methods, like oral and intravenous iron, and their role in ACD treatment.
| Iron Supplementation Method | Advantages | Disadvantages |
| Oral Iron | Easy to administer, cost-effective | Potential gastrointestinal side effects, variable absorption |
| Intravenous Iron | Bypasses hepcidin-mediated absorption block, rapid repletion of iron stores | Risk of infusion reactions, higher cost |
Other nutritional supplements are also important in managing ACD. Vitamin B12 and folate are key for making red blood cells. It’s important for patients with ACD to get enough nutrients.
Advanced treatments like ESAs and new methods are key for persistent anemia in ACD patients. When usual treatments don’t work, we use these advanced options to help patients.
ESAs are proteins that help make more red blood cells. They work like the hormone erythropoietin, which the kidneys make. They’re great for patients with anemia of chronic disease who don’t get better with iron or have too much erythropoietin.
New research is looking into new ways to treat anemia. These include agents that target hepcidin and its pathways, which could help more iron be available for making red blood cells.
By looking into these new treatments, we can offer better ways to manage anemia in ACD patients. This can greatly improve their quality of life and health outcomes.
Managing anemia of chronic disease well needs a few key steps. First, we must accurately diagnose it. Then, we treat the chronic condition that causes it. Lastly, we use supplements wisely.
Understanding the lab findings is key. This includes knowing how iron panels are affected and the role of hepcidin. This knowledge helps doctors create better treatment plans.
Treating the root cause of ACD is essential. Adding iron and other nutrients helps a lot. Sometimes, drugs that help make blood cells are needed too.
By taking a detailed approach to managing ACD, we can help patients a lot. Keeping up with the latest lab findings and treatment methods improves care. This makes life better for those with this condition.
Anemia of chronic disease, or ACD, is a condition where red blood cells decrease. It happens due to long-term inflammation or infection. This is often seen in diseases like rheumatoid arthritis, cancer, or HIV/AIDS.
In ACD, lab tests show a mild to moderate drop in hemoglobin. The count of new red blood cells is low. Also, iron levels in the blood are affected, with low serum iron and normal to high ferritin levels.
Hepcidin is a protein that controls iron in the body. In ACD, hepcidin levels go up. This makes less iron available, leading to anemia.
Iron supplements might help in some ACD cases. But it depends on the disease and how severe the anemia is. We check the patient’s iron levels before starting supplements.
Supplements like vitamin B12 and folate can help with anemia. But, a doctor should guide their use. This ensures they are safe and effective.
ESAs are drugs that help make more red blood cells. They might be used for anemia in chronic disease patients, including ACD. This is when other treatments don’t work well.
New treatments for ACD are being researched. These include ways to target hepcidin and other iron regulators. The goal is to better manage anemia and improve patient care.
Diagnosing ACD involves looking at the patient’s medical history and doing tests. These include a complete blood count and an iron panel. The doctor also checks the chronic condition.
Treating the underlying disease is key in managing ACD. It helps reduce anemia and improves patient health.
ACD can be managed and treated, but a “cure” depends on the disease. Treating the disease can solve anemia. But ongoing care might be needed in some cases.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!