Last Updated on November 17, 2025 by Ugurkan Demir

When the bone marrow fails, life-giving blood cells vanish. This leads to serious health problems. At LivHospital, we focus on understanding bone marrow failure. This happens when the marrow can’t make enough blood cells, causing health issues.
Knowing about bone marrow failure is key to managing it well. We aim to give a detailed look at its causes, symptoms, and treatments. We do this in a professional yet caring way.
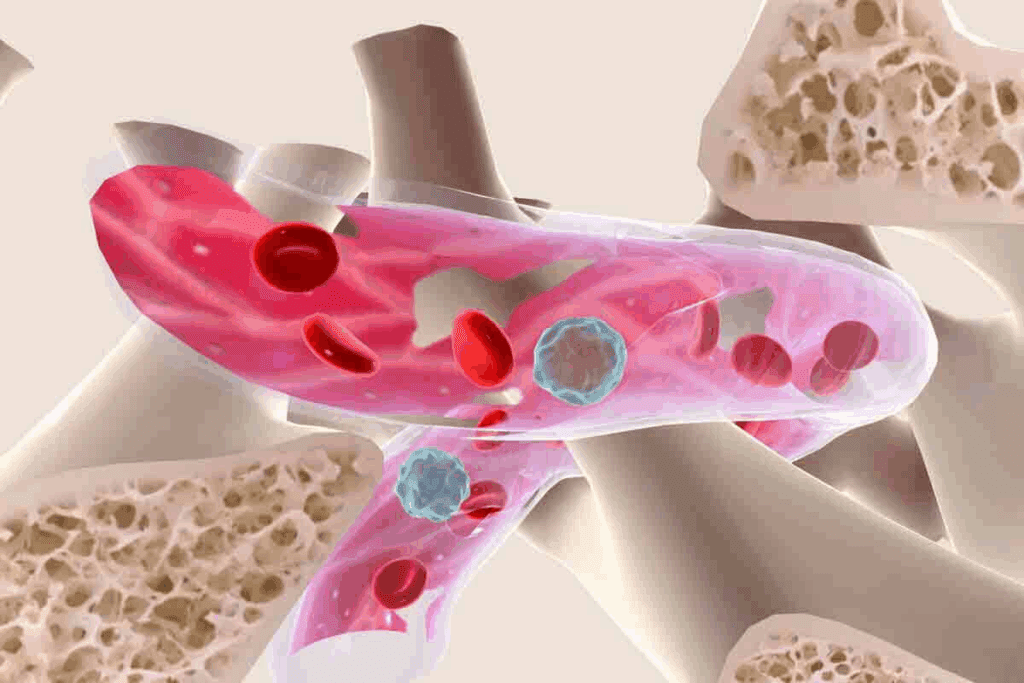
Bone marrow is key in making blood cells. Its failure can harm our health a lot. It makes red, white blood cells, and platelets. These are vital for oxygen transport, fighting infections, and blood clotting.
Bone marrow is the soft tissue in bones like hips and thighbones. It makes blood cells through hematopoiesis. This process turns stem cells into different blood cells. Healthy bone marrow is key for the right blood cell balance in our bodies.
Bone marrow works all the time, making millions of cells every day. Red cells carry oxygen, white cells fight infections, and platelets help blood clot. Each cell type has a special job, and their making is controlled by hormones and growth factors.
Bone marrow failure means it can’t make enough blood cells. This leads to bone marrow failure or insufficiency. It can cause a lack of red, white blood cells, or platelets, or any mix of these.
The effects of bone marrow failure are serious. Not enough red cells can make us tired, weak, and short of breath. Too few white cells raise infection risks. And not enough platelets can cause bleeding and bruising.
Knowing about bone marrow failure helps us spot its signs and get medical help. Understanding its role in health and disease shows why diagnosing and treating it is so important.

It’s key to know the different types of bone marrow failure disorders for the right diagnosis and treatment. These disorders happen when the bone marrow can’t make enough blood cells. They vary a lot in how they affect people.
Aplastic anemia is when the bone marrow can’t make blood cells. This includes red blood cells, white blood cells, and platelets. It can cause tiredness, infections, and bleeding.
It can be caused by toxins, certain medicines, viruses, or autoimmune diseases.
Key characteristics of aplastic anemia include:
Myelodysplastic syndromes (MDS) are disorders where the bone marrow makes abnormal blood cells. These cells can’t work right, leading to anemia, infections, and bleeding. In some cases, MDS can turn into acute myeloid leukemia (AML).
| Subtype | Characteristics | Risk of Progression to AML |
| Refractory Anemia | Anemia with minimal blasts in the bone marrow | Low |
| Refractory Anemia with Excess Blasts | Increased blasts in the bone marrow | Moderate to High |
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare disorder. It causes the destruction of red blood cells, bone marrow failure, and blood clots. It’s caused by a gene mutation that affects blood cell proteins.
“PNH is a complex disorder that requires a complete treatment plan to manage its symptoms, like hemolysis, thrombosis, and bone marrow failure.”
The image below shows how PNH affects blood cell production and survival.
There are other bone marrow failure syndromes like Fanconi anemia, dyskeratosis congenita, and Shwachman-Diamond syndrome. These conditions are caused by genetic mutations. They can lead to developmental issues and an increased cancer risk.
Each disorder needs a specific approach to diagnosis and treatment. This highlights the need to understand their unique features.
Bone marrow failure can come from several main causes. These can be genetic or acquired. Knowing these causes helps doctors diagnose and treat the condition better.
Genetic causes include inherited conditions that harm the bone marrow’s blood cell production. Some examples are:
These genetic conditions show why genetic testing is key in diagnosing bone marrow failure.
Acquired causes are things people can be exposed to in their lifetime. These can lead to bone marrow suppression or failure. Some examples include:
| Cause | Description | Impact on Bone Marrow |
| Genetic Conditions | Inherited disorders such as Fanconi Anemia and Shwachman-Diamond Syndrome | Impaired blood cell production |
| Toxins and Chemicals | Exposure to harmful substances | Damage to bone marrow cells |
| Radiation Therapy | High doses of radiation | Suppression of bone marrow function |
| Infections | Viral infections like hepatitis and HIV | Affects bone marrow function |
Knowing the causes of bone marrow failure is key to effective treatment. Doctors can tailor treatments based on whether the cause is genetic or acquired.
The signs of bone marrow failure can be hard to spot at first. But catching them early can really help with treatment. This condition affects how blood cells are made, leading to various health problems. We’ll look at the common signs and when to get medical help.
Fatigue and weakness are key symptoms, mainly because of anemia. Anemia happens when the bone marrow can’t make enough red blood cells. These cells carry oxygen. Without enough, people feel very tired, weak, and out of breath even when doing little.
Another big symptom is more infections because of not enough white blood cells. White blood cells fight off infections. Without enough, people get sick more often. If you keep getting infections or have a lot of fevers, it might be bone marrow failure.
Bleeding and bruising easily is also a sign, because of platelet deficiency. Platelets help blood clot. Not enough can cause easy bruising, nosebleeds, and bleeding that won’t stop. These signs mean the bone marrow isn’t making enough platelets.
If you’re always tired, keep getting sick, or bleed a lot, see a doctor. Early treatment can greatly improve your chances.
It’s tough to know these symptoms, but acting fast can really help manage bone marrow failure.
Bone marrow insufficiency affects more than just blood cells. It impacts many body functions, affecting health and quality of life.
This condition can cause anemia, a lack of red blood cells or hemoglobin. This lack of oxygen can harm the heart and other organs.
Specifically, anemia can cause:
| Cardiovascular Parameter | Normal Condition | Condition with Anemia |
| Heart Rate | 60-100 bpm | Often elevated |
| Oxygen Delivery | Adequate | Reduced |
| Cardiac Output | Normal | May be increased to compensate |
Bone marrow insufficiency often results in a decrease in white blood cells. This weakens the immune system’s ability to fight infections.
Consequences include:
Platelet deficiency, another consequence, can lead to bleeding and bruising. This affects the skin and mucous membranes, causing:
Understanding these systemic effects is key to managing bone marrow insufficiency. Healthcare providers can offer better care by addressing these impacts.
Figuring out why bone marrow fails starts with a detailed check-up. Doctors use tests and procedures to find the cause and see how bad the bone marrow problem is.
The first step is initial blood tests. These tests look for problems in blood cell counts and shapes. They can show signs of anemia, low white blood cells, or low platelets, which are common in bone marrow failure.
Important blood tests include:
| Blood Test | Purpose | Typical Findings in Bone Marrow Failure |
| Complete Blood Count (CBC) | Measures levels of different blood cells | Low counts of one or more cell types |
| Peripheral Blood Smear | Examines blood cells under a microscope | Abnormal cell morphology, blasts |
| Reticulocyte Count | Assesses bone marrow’s ability to produce new red blood cells | Low reticulocyte count indicating inadequate response |
A bone marrow biopsy is a key test that shows what’s happening in the bone marrow. It takes a small sample of bone marrow tissue, usually from the hip, for study.
The biopsy is done under local anesthesia. The sample is checked for cell count, cell shape, and any odd cell types. This helps doctors diagnose bone marrow problems like aplastic anemia and myelodysplastic syndromes.
Genetic testing is important for finding inherited bone marrow failure syndromes. These tests look for specific genetic changes linked to conditions like Fanconi anemia or Dyskeratosis congenita.
Genetic counseling is often suggested when these disorders are suspected. It helps families understand the diagnosis and the risks to other family members.
It’s also important to rule out other conditions that might look like or cause bone marrow failure. More tests are done to check for infections, autoimmune diseases, or other conditions that could harm the bone marrow.
By combining the results of these tests, doctors can accurately diagnose bone marrow failure. They can then choose the best treatment plan.
Managing bone marrow failure needs a mix of supportive care and treatments that change the disease’s course. We’ll dive into these methods to see how they help patients.
Supportive care is key in handling bone marrow failure symptoms and boosting patients’ quality of life. It includes:
These steps are often paired with other treatments for a full care plan.
| Supportive Care Measure | Purpose | Benefits |
| Blood Transfusions | Fix anemia and low platelets | Boosts oxygen, cuts down on bleeding |
| Growth Factors | Boost blood cell making | Speeds up recovery, lowers infection risk |
| Antimicrobial Prophylaxis | Stop infections | Lessens sickness, death risk |
Disease-modifying treatments aim to fix the bone marrow failure’s root causes. These include:
These treatments might change the disease’s path and better long-term results.
By mixing supportive care with treatments that change the disease, doctors can create a detailed plan for each bone marrow failure patient.
Daily life with bone marrow failure can be tough. But, there are ways to make it easier. Patients need to take a full approach to manage their condition well.
Stopping infections is key for those with bone marrow failure. Frequent handwashing is a simple yet powerful way to fight off infections. It’s also important to avoid sick people and crowded places.
Getting vaccinated, like the flu shot and pneumococcal vaccine, helps prevent infections. Good hygiene when handling food is also vital. Avoiding raw or undercooked foods that may have bacteria is important.
“Prevention is key when it comes to managing bone marrow failure. By taking simple precautions, patients can significantly reduce their risk of infection.”
Eating a balanced diet is key for health. Patients with bone marrow failure should eat nutrient-rich foods. This includes fruits, vegetables, whole grains, and lean proteins.
| Food Group | Recommended Foods |
| Fruits | Apples, bananas, berries |
| Vegetables | Leafy greens, broccoli, carrots |
| Proteins | Lean meats, fish, eggs |
| Grains | Whole wheat bread, brown rice, quinoa |
Regular exercise is good for health. But, patients with bone marrow failure should talk to their doctor before starting any new exercise.
Yoga or short walks are good options. It’s important to balance activity with rest to avoid getting too tired.
Bone marrow failure can affect mental health. Patients should get emotional support from loved ones, friends, or support groups. Professional counseling can also help with stress and anxiety.
By using these strategies, patients with bone marrow failure can live better and manage their condition more effectively.
The prognosis for bone marrow failure depends on many factors. These include the cause and how well treatment works. It’s vital for both patients and doctors to understand these to make good care plans.
Several factors affect bone marrow failure prognosis. These are the type of disorder, the patient’s health, and treatment response. Early diagnosis and the right treatment can greatly improve chances.
Survival rates for bone marrow failure vary by disorder. For example, aplastic anemia and myelodysplastic syndromes have different survival rates.
| Disorder Type | 1-Year Survival Rate | 5-Year Survival Rate |
| Aplastic Anemia | 80% | 70% |
| Myelodysplastic Syndromes | 60% | 40% |
| Paroxysmal Nocturnal Hemoglobinuria | 90% | 80% |
While life expectancy is important, quality of life is just as important for those with bone marrow failure. It’s about managing symptoms, preventing infections, and keeping well physically and emotionally.
Healthcare providers can help patients live well despite their condition. They focus on these key areas to improve quality of life.
The field of bone marrow failure treatment is on the verge of a major breakthrough. New research is opening up several promising areas. These include novel therapies, advancements in gene editing, and improved transplantation techniques.
Several new therapies are being tested in clinical trials for bone marrow failure. These include:
These therapies show great promise and are being closely watched in ongoing clinical trials.
Gene editing technology, like CRISPR/Cas9, has changed the game in genetics. It’s now being used in bone marrow failure research. This technology allows for precise editing of genes, which could lead to new treatments for genetic forms of bone marrow failure.
Key benefits of gene editing include:
Transplantation is a key treatment for many with bone marrow failure. Recent advancements have made transplants more effective. These include:
These improvements have led to better survival rates and quality of life for transplant patients.
We’ve looked into bone marrow failure, where the bone marrow can’t make enough blood cells. It’s important to know the causes, symptoms, and treatments to manage it well.
Symptoms of bone marrow failure include feeling very tired, getting sick more often, and bleeding easily. Spotting these signs early is key for getting help quickly. Doctors use blood tests and bone marrow biopsies to diagnose it.
Treating bone marrow failure needs a full plan, including care to support the body and treatments that can change the disease. New research is bringing better treatments, giving patients hope.
Understanding bone marrow failure better means we need to work together to care for patients. We must look at the physical, emotional, and mental sides of the condition. This way, we can offer the best support.
Bone marrow failure happens when the bone marrow can’t make enough blood cells. This includes red blood cells, white blood cells, and platelets. It leads to health problems.
Symptoms include feeling very tired, weak, and getting sick more often. You might also bruise easily, bleed a lot, and have trouble breathing. These symptoms depend on which blood cells are affected.
It can be caused by genes or inherited disorders. It can also be caused by toxins, certain medicines, infections, or autoimmune diseases.
Doctors start with blood tests and a bone marrow biopsy. They also do genetic testing. This helps find out why and how bad the bone marrow failure is.
Treatments include blood transfusions and antibiotics to help. There are also medicines to fight the disease and bone marrow transplants.
To manage daily life, prevent infections, eat right, and stay active. It’s also important to get emotional and psychological support.
The outlook depends on the cause, how well you respond to treatment, and your overall health. Some people get better, while others face a tougher road.
Yes, new treatments and gene editing are being researched. These could lead to better care in the future.
It can harm the heart by reducing oxygen. It weakens the immune system by lowering white blood cells. It also affects the skin and mucous membranes due to blood cell shortages.
Some cases can be treated or even cured with the right therapy, like bone marrow transplants. Others may need ongoing care.
Life expectancy varies a lot. It depends on the disorder, treatment response, and any complications. Always talk to your doctor about your specific situation.
References
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!