Last Updated on November 17, 2025 by Ugurkan Demir
Bone marrow is key to our health, making blood cells that move through our body. But, many disorders can harm its work, causing health problems.
At Liv Hospital, we know how complex bone marrow health is. We see how both cancer and non-cancer issues affect patients. Bone marrow cancers, like leukemia, lymphoma, and myeloma, cause hundreds of thousands of new cases each year in the U.S.
It’s important to know the differences between these conditions for the right treatment. We’ll explore 15 common bone marrow diseases. We’ll cover their symptoms, how to diagnose them, and treatment choices.
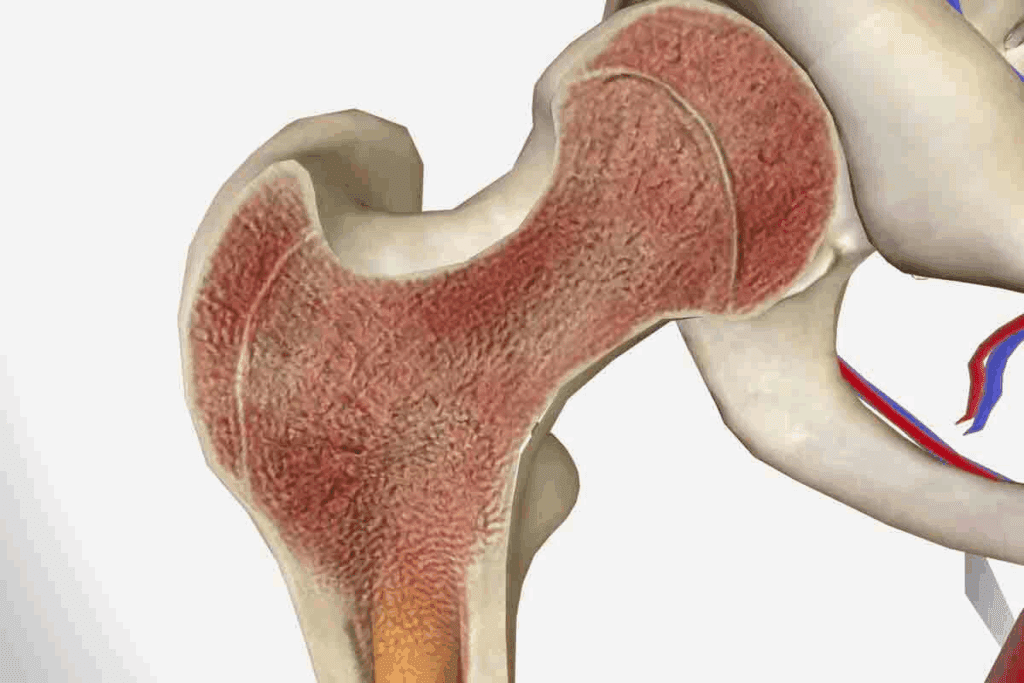
Bone marrow is more than just a part of our bones. It’s a dynamic organ that makes the blood cells we need. These cells help carry oxygen, fight off infections, and stop bleeding. Red blood cells, white blood cells, and platelets are all made in bone marrow, keeping us healthy.
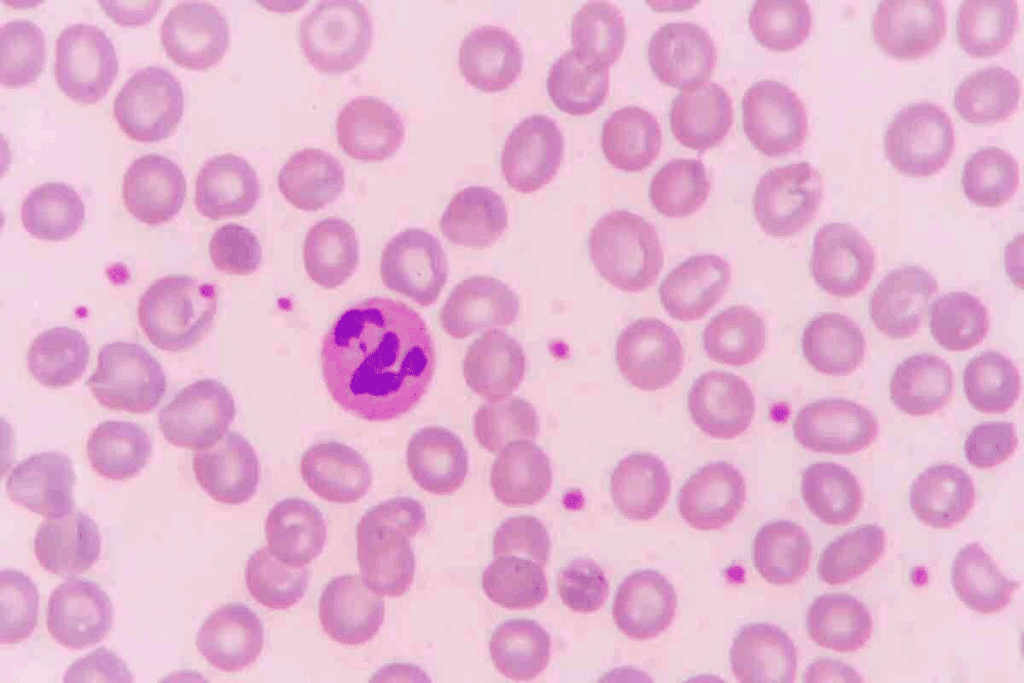
Bone marrow makes all blood cells through a process called hematopoiesis. It turns hematopoietic stem cells into different types of blood cells. These stem cells can grow and change into any blood cell type, which is key for our health.
Many factors control how blood cells are made. For example, erythropoietin helps make red blood cells. Granulocyte-colony stimulating factor (G-CSF) helps make certain white blood cells. Knowing how these work helps doctors treat bone marrow problems.
Healthy bone marrow has many cell types, like stem cells and mature blood cells. It also has blood vessels and stromal cells that help blood cells grow. The right mix of cells and a good environment are important for our health.
In short, bone marrow is key to our health by making blood cells. Knowing how it works helps us understand and treat bone marrow issues.

Blood marrow disorders come from a mix of genetic and acquired factors. These issues affect the bone marrow’s ability to make healthy blood cells. Knowing the causes and risk factors is key for diagnosis and treatment.
Genetics play a big role in bone marrow disorders. Some genetic mutations are passed down, making people more likely to get conditions like aplastic anemia or myelodysplastic syndromes. For example, DNA repair gene mutations can cause bone marrow failure.
Conditions like Fanconi anemia and Diamond-Blackfan anemia affect bone marrow. They come from mutations in genes important for making blood cells. Knowing this helps in finding better treatments.
Acquired causes of bone marrow problems include toxins, infections, and treatments. Chemicals like benzene and heavy metals can harm bone marrow. Radiation and some cancer treatments also affect it.
Infections, like hepatitis and HIV, can harm bone marrow. Autoimmune diseases, where the body attacks itself, can also cause problems.
Environmental factors and lifestyle choices matter too. For example, long-term exposure to toxins increases the risk of myelodysplastic syndromes.
“The interplay between genetic predisposition and environmental exposure is key to understanding the etiology of bone marrow disorders.”
Hematologist
In summary, both genetics and acquired factors lead to blood marrow disorders. Knowing these causes and risk factors is vital for early diagnosis and treatment.
Abnormal bone marrow findings can be scary, but they don’t always mean cancer. Getting such news can be unsettling. It’s normal to wonder what it means.
Bone marrow abnormalities can come from many conditions. These range from harmless disorders to serious diseases like cancer. It’s important to know if it’s cancer or not to get the right treatment.
Not every abnormal bone marrow finding is cancer. Many non-cancerous conditions can affect it, like infections or nutritional deficiencies. For example, aplastic anemia is when the bone marrow can’t make blood cells, but it’s not cancer.
But, some cancers like leukemia or lymphoma can also affect the bone marrow. To figure out if it’s cancer, we use different tests.
Figuring out what’s wrong with the bone marrow involves several tests. Some key ones are:
These tests help us find out what’s wrong and plan the right treatment. It’s key to talk to doctors to understand your diagnosis and treatment.
Knowing the difference between cancerous and non-cancerous bone marrow conditions is key. We aim to give full care and support to those with bone marrow disorders.
We will explore aplastic anemia and related conditions that affect the bone marrow’s ability to produce blood cells. Aplastic anemia is a rare and potentially life-threatening disorder. It happens when the bone marrow fails to produce enough blood cells. This leads to fatigue, infections, and bleeding complications.
Aplastic anemia is when the bone marrow can’t make blood cells. This includes red blood cells, white blood cells, and platelets. Symptoms can vary but often include fatigue, shortness of breath, and increased infections because of the lack of healthy blood cells.
To diagnose aplastic anemia, doctors do blood tests and a bone marrow biopsy. They check the bone marrow’s function and rule out other causes of bone marrow failure.
Fanconi anemia is a rare genetic disorder. It affects the body’s ability to produce blood cells and increases the risk of cancer. It is characterized by congenital abnormalities, bone marrow failure, and a predisposition to malignancies.
Symptoms of Fanconi anemia vary but often include physical abnormalities and an increased risk of infections and bleeding. This is due to bone marrow failure.
Diamond-Blackfan anemia is another rare genetic disorder. It affects the production of red blood cells. It is characterized by anemia, congenital abnormalities, and an increased risk of cancer.
Patients with Diamond-Blackfan anemia often have anemia in infancy or early childhood. The diagnosis is confirmed through genetic testing and bone marrow examination.
| Condition | Primary Characteristics | Symptoms |
| Aplastic Anemia | Bone marrow failure to produce blood cells | Fatigue, infections, bleeding |
| Fanconi Anemia | Genetic disorder affecting blood cell production and cancer risk | Congenital abnormalities, bone marrow failure, malignancies |
| Diamond-Blackfan Anemia | Genetic disorder affecting red blood cell production | Anemia, congenital abnormalities, cancer risk |
Treatment options for these bone marrow failure syndromes vary. They depend on the specific condition and its severity. Treatments may include immunosuppressive therapy, bone marrow transplantation, and supportive care. These help manage symptoms and prevent complications.
Myelodysplastic syndromes (MDS) are a group of disorders where the bone marrow can’t make healthy blood cells. This causes problems like anemia, infections, and bleeding. We’ll look at the different types of MDS and the treatments available.
MDS is not one disease but a collection of disorders. They are classified based on the blood cells affected and the condition’s severity. The main types are:
Knowing the specific type of MDS is key to understanding the prognosis and choosing the right treatment.
Treatment for MDS varies based on the type, severity, and the patient’s health. The goals are to improve blood counts, reduce complications, and manage symptoms. Common treatments include:
Each patient’s treatment is customized to their needs and MDS characteristics. We work closely with patients to create a care plan that fits their unique situation.
Myeloproliferative neoplasms (MPNs) are blood disorders where the bone marrow makes too many blood cells. This can cause health problems like blood clots and a higher risk of leukemia. It also leads to other serious issues.
We will look at the different types of MPNs, their signs, and the challenges in diagnosing and treating them.
Essential thrombocythemia means the bone marrow makes too many platelets. This raises the risk of blood clots and bleeding. Symptoms include headaches, dizziness, and feeling tired.
Polycythemia vera makes the bone marrow produce too many red and white blood cells and platelets. This makes blood thicker, increasing the risk of clots. Symptoms include itching, feeling full in the left upper abdomen, and an enlarged spleen.
Primary myelofibrosis replaces the bone marrow with fibrotic tissue, reducing blood cell production. Symptoms include severe anemia, fatigue, and an enlarged spleen. The disease’s progression varies among patients.
Chronic myelomonocytic leukemia starts in the bone marrow and invades the blood. It’s marked by an increase in monocytes. Symptoms include weight loss, fatigue, and an enlarged spleen.
Diagnosing MPNs requires blood tests, bone marrow biopsies, and genetic tests. These help identify specific mutations linked to these disorders.
| MPN Subtype | Primary Characteristics | Common Symptoms |
| Essential Thrombocythemia | Overproduction of platelets | Headaches, dizziness, fatigue |
| Polycythemia Vera | Overproduction of red blood cells, white blood cells, and platelets | Itching, enlarged spleen |
| Primary Myelofibrosis | Replacement of bone marrow with fibrotic tissue | Severe anemia, fatigue, enlarged spleen |
| Chronic Myelomonocytic Leukemia | Increased number of monocytes in blood and bone marrow | Weight loss, fatigue, enlarged spleen |
Knowing the exact type of MPN is key to finding the right treatment. Treatments include medicines to lower blood cell counts, targeted therapies, and sometimes bone marrow transplants.
Hemoglobinopathies, like sickle cell disease and thalassemia, are genetic disorders. They affect hemoglobin structure or production, causing anemia and other issues. These conditions impact the bone marrow, where red blood cells are made.
The bone marrow is key in making red blood cells. Disorders affecting hemoglobin production can cause health problems. We’ll look at sickle cell disease and thalassemia, covering their causes, symptoms, and treatments.
Sickle cell disease is a genetic disorder. It results in abnormal hemoglobin, called hemoglobin S. This abnormal hemoglobin makes red blood cells sickle-shaped, leading to their early destruction and anemia.
Symptoms of sickle cell disease vary but often include pain episodes, infections, and anemia. Treatment options include pain and infection management drugs, blood transfusions, and sometimes bone marrow transplantation.
Thalassemia is another genetic disorder affecting hemoglobin production. It results in reduced or missing globin chains, causing anemia and other issues.
Thalassemia’s severity varies, with some forms mild and others needing regular blood transfusions. Treatment for thalassemia often involves blood transfusions to improve anemia and manage iron overload from frequent transfusions.
In conclusion, hemoglobinopathies like sickle cell disease and thalassemia significantly affect the bone marrow and overall health. Understanding these conditions is key to providing proper care and management.
Certain nutritional and metabolic conditions can deeply affect the bone marrow. They can harm the bone marrow’s ability to make blood cells. This happens due to a lack of essential nutrients and metabolic disorders.
Vitamin B12 is key for making red blood cells. A lack of vitamin B12 can cause pernicious anemia. This leads to big, abnormal red blood cells that don’t work right.
This can happen if you don’t have enough intrinsic factor in your stomach. Or if your diet doesn’t have enough vitamin B12.
Symptoms include feeling very tired, weak, and having neurological issues. Treatment usually involves vitamin B12 shots or pills. The goal is to help make normal red blood cells again.
Folate is vital for DNA and repair. A lack of folate can cause megaloblastic anemia, like vitamin B12 deficiency. This can come from not eating enough folate, needing more during pregnancy, or not absorbing it well.
To treat folate deficiency, you might need to change your diet and take supplements. It’s important to know the difference between folate and vitamin B12 deficiency. Taking folate can hide symptoms of vitamin B12 deficiency, which could harm your nerves.
Gaucher disease is a genetic disorder. It’s caused by not having enough glucocerebrosidase enzyme. This leads to too much glucocerebroside in cells, including bone marrow cells.
This buildup can cause anemia, low platelet count, and bone problems. Treatment includes enzyme replacement therapy (ERT) and substrate reduction therapy (SRT). These aim to reduce glucocerebroside buildup and manage symptoms.
Beyond cancer, bone marrow can face many non-cancerous diseases. These diseases can cause health problems like anemia and fatigue. We will look at some of these diseases, their symptoms, and how to treat them.
Sideroblastic anemia is a disorder where iron builds up in red blood cell precursors. This leads to anemia. It can be inherited or caused by other factors like toxins.
People with sideroblastic anemia feel tired, weak, and short of breath. Doctors use bone marrow tests and genetic tests to diagnose it. Treatment might include iron chelation therapy and blood transfusions.
Key aspects of sideroblastic anemia:
Pure red cell aplasia is a rare condition where the bone marrow doesn’t make red blood cells. It can be present at birth or caused by other conditions.
Those with this condition have severe anemia, fatigue, and weakness. Doctors diagnose it with a bone marrow biopsy. Treatment includes addressing the cause, immunosuppressive therapy, and blood transfusions.
“Pure red cell aplasia is a condition that highlights the complexity of bone marrow disorders and the need for precise diagnosis and treatment,” said a leading hematologist.
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare disease that destroys red blood cells and affects bone marrow. It’s caused by a gene mutation.
Symptoms include dark urine, fatigue, and abdominal pain. Doctors use flow cytometry to diagnose it. New treatments have greatly improved outcomes for patients.
Treatment advancements for PNH:
Mastocytosis is a disorder where mast cells build up in organs. It can be skin-related or affect the whole body, including the bone marrow.
Symptoms vary and can include skin lesions, stomach issues, and bone pain. Diagnosis involves biopsy and mast cell marker tests. Treatment depends on the disease’s severity and symptoms.
In conclusion, diseases like sideroblastic anemia, pure red cell aplasia, paroxysmal nocturnal hemoglobinuria, and mastocytosis pose challenges. Understanding these conditions is key to better care and outcomes for patients.
Effective treatment for blood marrow disorders needs a detailed plan. Each patient’s case is different. So, treatment must fit the disorder, its severity, and the patient’s health.
Bone marrow transplantation is a key treatment for many blood marrow disorders. It replaces the patient’s bad marrow with good marrow. There are two main types:
The choice depends on the condition, donor availability, and the patient’s health.
Medications are key in treating blood marrow disorders. They help manage symptoms, improve life quality, and sometimes cure the condition. Common treatments include:
The field of hematology is growing fast. New treatments and therapies are being developed. These include gene therapy, targeted therapies, and new medicines. Clinical trials test these new treatments for safety and effectiveness.
We aim to keep up with these new developments. This way, our patients get the latest and best treatments.
Understanding bone marrow disorders is key to managing and treating them. We’ve looked at different conditions, their causes, symptoms, and how to treat them.
Living with these diseases needs a lot of care and support. With the right diagnosis and treatment, many people can live full and active lives. Support for patients is very important. It helps them deal with their condition and make smart health choices.
Healthcare providers are essential in helping patients with bone marrow disorders. They give accurate diagnoses, create effective treatment plans, and offer ongoing support. This support greatly improves patient outcomes.
As we learn more about bone marrow diseases, we can find better treatments. This will improve the lives of those affected. By working together, we can positively change the lives of patients with bone marrow diseases.
Bone marrow is a spongy tissue inside some bones, like the hips and thighbones. It makes blood cells, including red blood cells, white blood cells, and platelets.
Bone marrow disorders are conditions that affect the bone marrow’s ability to make healthy blood cells. They can be cancerous or non-cancerous.
No, not always. Some bone marrow disorders are cancerous, but others are not. Examples include aplastic anemia and myelodysplastic syndromes.
Causes and risk factors include genetic predispositions, toxins, infections, and acquired conditions. These can lead to bone marrow dysfunction.
Aplastic anemia is a rare blood disorder. The bone marrow fails to make blood cells. This leads to fatigue, infections, and bleeding.
Myelodysplastic syndromes (MDS) are disorders with poorly formed or dysfunctional blood cells. They often progress to acute myeloid leukemia.
Myeloproliferative neoplasms (MPNs) are blood cancers. They cause the excessive production of blood cells. Examples include essential thrombocythemia and polycythemia vera.
Hemoglobinopathies are genetic disorders affecting hemoglobin production. Examples include sickle cell disease and thalassemia. They can impact bone marrow function and overall health.
Treatments include bone marrow transplantation, medication, and emerging treatments. The goal is to manage symptoms, improve quality of life, and achieve remission.
Bone marrow transplantation is a procedure. It infuses healthy bone marrow cells into a patient. It’s used to treat blood cancers and other disorders.
Yes, non-cancerous disorders can be treated. Therapies include medications, lifestyle changes, and supportive care. They help manage symptoms and improve quality of life.
Disorders are diagnosed through medical history, physical examination, and laboratory tests. A bone marrow biopsy is also used. It helps find the cause of symptoms.
Compassionate care is key for patients with bone marrow diseases. It helps manage symptoms, improve quality of life, and achieve the best outcomes. A team of healthcare providers is needed.
References
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!