Last Updated on November 17, 2025 by Ugurkan Demir

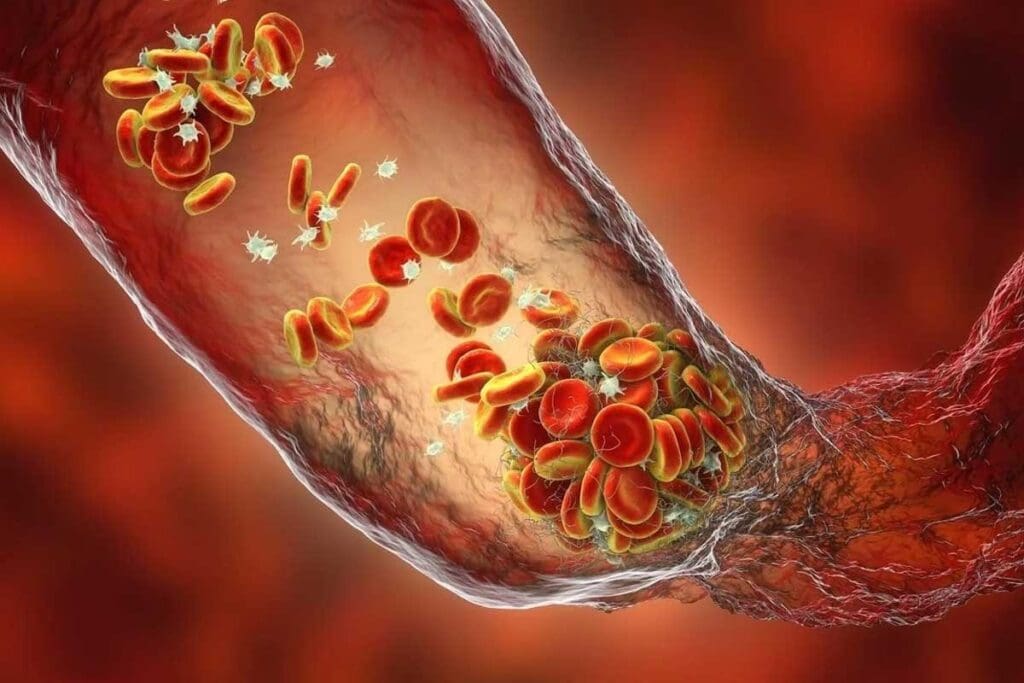
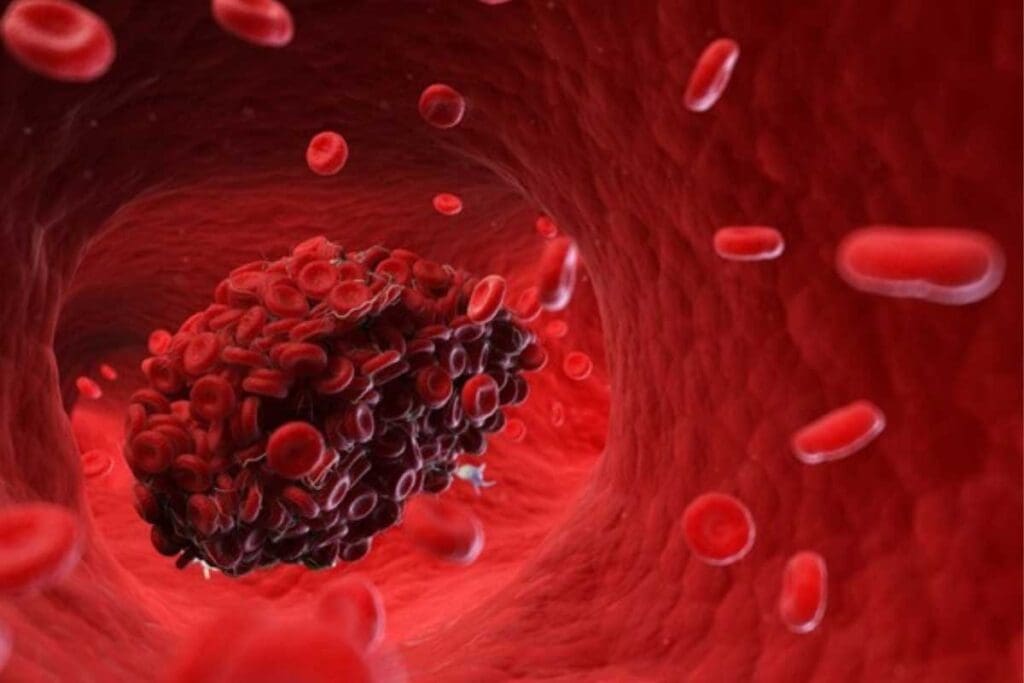
Thrombosis is a serious medical condition where a blood clot forms inside a blood vessel. This blocks the normal flow of blood. When a blood vessel gets injured, the body forms a clot to stop bleeding. But, if a clot forms inside a vessel without injury, it can cause severe problems like stroke and heart attack. Understand what is thrombosis and how a blood clot can obstruct a blood vessel and cause serious risks.
At LivHospital, we know how critical it is to quickly spot and treat thrombosis. Our team works together to give patients the best care. Studies show thrombosis is a major cause of death in developed countries, with big risks from venous thromboembolism.
It’s key to know the risks and causes of thrombosis to prevent it and get medical help fast. We stress the need for top-notch medical care to handle thrombosis and its issues.
Thrombosis is when a blood clot forms inside a blood vessel. This can block blood flow. It’s a big worry in medicine because it can lead to serious health problems.
We’ll explore what thrombosis is, why it matters, and the terms used worldwide. Knowing these terms helps doctors and patients talk clearly.
Thrombosis means a blood clot forms in a blood vessel. This clot can be in an artery or vein and block blood flow. The thrombotic process includes platelets sticking together, the coagulation cascade starting, and a fibrin clot forming.
There’s a lot of jargon around thrombosis. For example, “thrombus” is the clot itself, while “thrombosis” is the clotting process. Knowing these terms is key to diagnosing and treating blood clots.
Thrombosis has different names in many languages. It’s called “trombosis” in Spanish, “thrombose” in French, and “tromboza” in some Eastern European languages. This shows how important it is for doctors to communicate clearly, no matter where they are.
Here’s a table showing how thrombosis is called in different languages:
| Language | Term Used for Thrombosis |
| English | Thrombosis |
| Spanish | Trombosis |
| French | Thrombose |
| Some Eastern European languages | Tromboza |
The table shows how “thrombosis” is spelled differently in various languages. But its importance is the same everywhere.
Understanding thrombosis and its global terms helps us see how complex it is. It also shows why medical practices need to be the same everywhere.
It’s important to know how blood clotting works to understand thrombosis. Blood clotting, or hemostasis, stops bleeding when a blood vessel is hurt. Normal hemostasis is a delicate balance between procoagulant and anticoagulant factors, making sure clots form only when needed.
The normal hemostasis process has several steps. First, vascular spasm reduces blood flow to the injured area. Then, platelet plug formation temporarily seals the injury. The coagulation cascade makes this plug stronger with a fibrin clot.
“The coagulation cascade is a series of chemical reactions that lead to the formation of a blood clot,” as noted by medical professionals. This process involves various clotting factors, each playing a specific role in the cascade.
When the normal clotting process goes wrong, it can cause thrombosis. This happens when the balance between procoagulant and anticoagulant factors is off, leading to too much clotting. Pathological clotting can be triggered by various factors, including genetic predispositions, environmental factors, and underlying medical conditions.
Understanding these factors is key to diagnosing and treating thrombotic conditions. By spotting the signs and symptoms of pathological clotting, healthcare providers can act early to prevent serious problems.
Blood clots, or thrombosis, can form in arteries and veins. Each type affects health differently. Knowing the differences is key for correct diagnosis and treatment.
Arterial thrombosis happens when a clot forms in an artery. Arteries carry oxygen-rich blood from the heart to the body. This can lead to heart attacks or strokes, depending on where the clot is.
Characteristics of Arterial Thrombosis:
Venous thrombosis occurs in veins, which carry deoxygenated blood back to the heart. The most common type is deep vein thrombosis (DVT), found in the legs.
Characteristics of Venous Thrombosis:
| Characteristics | Arterial Thrombosis | Venous Thrombosis |
| Vessel Involved | Arteries | Veins |
| Common Locations | Heart, Brain | Legs |
| Associated Conditions | Atherosclerosis | Immobility, Surgery |
| Symptoms Onset | Acute | Variable |
| Potential Complications | Heart Attack, Stroke | Pulmonary Embolism |
It’s vital for doctors to understand the differences between arterial and venous thrombosis. Each needs a specific treatment plan to avoid serious issues.
Vessel obstruction happens when a thrombus forms and sticks to the vessel wall. This can block blood flow, either partially or completely. It’s key to understanding the effects of thrombosis.
Thrombus formation is complex, involving blood coagulation, platelet activation, and endothelial dysfunction. When a blood vessel gets injured, the body tries to stop bleeding by forming a clot. But in thrombosis, this leads to a harmful clot that blocks blood flow.
Thrombi stick to the vessel wall thanks to adhesion molecules and platelet-endothelial interactions. As they grow, they can block blood flow in the vessel.
The move from partial to complete blockage depends on several things. These include the thrombus’s size and location, how fast it grows, and if there are other blood paths. Partial blockage can reduce blood flow, causing pain or dysfunction.
As the thrombus gets bigger, it can block the vessel completely. This can cause severe tissue damage or even death. The effects of complete blockage are very serious, making quick diagnosis and treatment critical.
In summary, knowing how vessel obstruction works is vital for managing blood clots. By understanding what causes thrombi, healthcare teams can find better ways to prevent and treat them.
It’s key to know the main signs of thrombosis for good diagnosis and treatment. Thrombosis shows up in different ways, affecting patients a lot. We’ll look at two big ones: Deep Vein Thrombosis (DVT) and Pulmonary Thrombosis/Embolism.
Deep Vein Thrombosis happens when a blood clot forms in deep veins, usually in the legs. Symptoms of DVT can be subtle and may include swelling, pain, or discoloration of the affected limb. If not treated, DVT can cause serious problems, like Pulmonary Embolism.
Early detection is critical, as it lets us act fast to stop serious problems. We use tools like ultrasound and D-dimer tests to find DVT.
Pulmonary Embolism (PE) happens when a clot travels to the lungs, blocking blood flow. This is a medical emergency that needs quick action. Symptoms can range from mild shortness of breath to severe respiratory distress.
“Pulmonary embolism is a life-threatening condition that necessitates prompt diagnosis and treatment to prevent fatal outcomes.”
The signs of PE can be hard to spot, making diagnosis tricky. We use imaging like CT pulmonary angiography to confirm it.
Knowing the signs of DVT and PE is vital for doctors to give the right care. By understanding these conditions, we can help patients better and lower the risk of serious problems.
It’s key for doctors to know about the dangers of thrombotic events. These events can cause serious problems that might even be life-threatening. They can really affect how well a patient does.
Stroke is a big problem caused by blood clots in the brain. There are two types: cerebral thrombosis and cerebral embolism. Thrombosis is when a clot forms in the brain. Embolism is when a clot travels there from elsewhere.
Both can lead to ischemic stroke. This is when the brain doesn’t get enough blood. It can cause permanent damage if not treated fast.
Myocardial infarction, or a heart attack, is another serious issue. It happens when a blood clot blocks a coronary artery. This stops blood from reaching the heart muscle.
This can cause heart tissue to die. It’s very serious and can be deadly.
To treat a heart attack, doctors use thrombolytic therapy or primary PCI. These methods help get blood flowing again to the heart.
There are other serious problems too. These include pulmonary embolism, deep vein thrombosis (DVT), and peripheral arterial thrombosis. Pulmonary embolism is when a clot goes to the lungs and can be deadly.
DVT is when a clot forms in the deep veins, usually in the legs. It can cause problems like post-thrombotic syndrome or even pulmonary embolism if not treated right.
Peripheral arterial thrombosis is when a clot forms in the arteries of the limbs. It can cause limb ischemia or gangrene. It’s very important to treat these quickly to avoid serious harm or death.
Knowing the risk factors for thrombosis is key for prevention and treatment. Thrombosis is when blood clots form inside a blood vessel. These factors can be inherited or acquired.
Inherited thrombophilia is a genetic condition that raises the risk of abnormal blood clots. Mutations like Factor V Leiden and prothrombin G20210A can greatly increase the risk of blood clots. If you have a family history of blood clots, talk to your doctor about genetic testing and risk assessment.
Genetic factors can make you more likely to get blood clots. For example, not having enough proteins C and S, or antithrombin, can raise your risk. Knowing your genetic predispositions helps in creating a prevention plan.
Acquired risk factors also play a big role in getting thrombosis. These include being immobile, having recent surgery, cancer, and certain medical conditions. Lifestyle choices like smoking and being overweight also increase your risk.
Medical conditions and treatments can also up your risk. For instance, people having major surgery, like orthopedic surgery, are at higher risk of DVT. Cancer and its treatments can also raise your risk due to substances that promote clotting.
Healthcare providers can use this knowledge to create prevention and treatment plans. This includes using anticoagulant medications, making lifestyle changes, and other interventions based on your risk profile.
Diagnosing thrombosis requires a detailed approach. This includes clinical assessment, imaging, and lab tests. Getting the diagnosis right is key for good treatment and care.
We start with a detailed clinical assessment. This looks at the patient’s history, symptoms, and risk for thrombosis. Tools like the Wells score help figure out the chance of deep vein thrombosis (DVT) or pulmonary embolism (PE).
This step is important. It helps decide what tests to do next and who’s at the highest risk.
Imaging is a big part of diagnosing thrombosis. Ultrasound is often used for DVT. Computed tomography pulmonary angiography (CTPA) is the top choice for PE.
Labs play a big role in diagnosing thrombosis. D-dimer tests are common. They check for D-dimer, a sign of clot breakdown.
| Laboratory Test | Application |
| D-dimer | Excluding DVT and PE in low-risk patients |
| Coagulation Profile | Assessing bleeding risk and monitoring anticoagulation therapy |
| Thrombophilia Screening | Identifying genetic or acquired thrombophilic conditions |
Biomarkers like troponin and BNP can also help. They show if there’s been a thrombotic event.
Today, treating thrombosis involves a mix of medicine, intervention, and surgery. The right treatment depends on the thrombosis’s type, location, and how severe it is. It also depends on the patient’s health.
Anticoagulant medications play a key role in managing thrombosis. They stop new clots from forming and prevent existing ones from getting bigger. Heparin, warfarin, and newer drugs like rivaroxaban and apixaban are used.
Thrombolytic therapy is used for severe cases. It breaks down clots that block blood flow. This is very important for acute ischemic stroke and massive pulmonary embolism.
For more serious cases, doctors might use interventional or surgical methods. Thrombectomy, or removing the clot surgically, is sometimes needed. Techniques like catheter-directed thrombolysis are also used to treat clots without surgery.
Surgery might be needed to deal with thrombosis complications or to remove a clot. The decision to have surgery depends on the patient’s situation and the risks involved.
We make treatment plans that fit each patient’s needs. By using medicine, intervention, and surgery together, we can manage thrombosis well. This helps improve patient outcomes.
Preventing thrombosis means knowing the risks and taking steps to avoid them. We look at who’s at risk and use medicines to help. We also encourage healthy lifestyle choices.
Stopping thrombosis needs a full plan. This includes finding people with inherited conditions and handling other risks. As we learn more, we’ll find better ways to help patients.
New research will lead to better ways to stop thrombosis. We’ll get better at diagnosing and treating it. Our goal is to keep improving care and results for patients.
Thrombosis is when a blood clot forms inside a blood vessel. This blocks blood flow. It can cause health problems, depending on where and how big the clot is.
Arterial thrombosis happens when a clot forms in an artery. It can lead to heart attacks or strokes. Venous thrombosis occurs in veins, causing DVT or pulmonary embolism.
Thrombosis risk factors include genetic and acquired conditions. Genetic factors are inherited clotting tendencies. Acquired factors include age, obesity, smoking, and immobility.
Diagnosing thrombosis involves clinical assessment and imaging like ultrasound or CT scans. Laboratory tests also check for clotting disorders.
Treatments include anticoagulant medications and interventional techniques like thrombolysis. Sometimes, surgery is needed to remove or bypass the clot.
DVT is a blood clot in the deep veins, usually in the legs. Treatment includes anticoagulant medication and compression stockings to reduce swelling.
Pulmonary thrombosis/embolism is a blood clot in the lungs. Symptoms include sudden shortness of breath, chest pain, and coughing up blood. It needs immediate medical attention.
Preventing thrombosis involves managing risk factors. This includes maintaining a healthy weight, staying active, avoiding immobility, and using anticoagulant medications as prescribed.
Thrombosis complications include stroke, myocardial infarction, and pulmonary embolism. It can also cause post-thrombotic syndrome, leading to chronic pain and swelling.
LivHospital provides top-notch care for thrombosis patients. They offer advanced diagnostic and treatment options, including pharmacological and interventional therapies, to improve patient outcomes.
References
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!