At Liv Hospital, we know how serious a blood clot in artery, also called arterial thrombosis, is. It’s when a clot blocks blood flow in an artery. This can cause heart attacks or strokes, which are very dangerous.
Arterial thrombosis happens when a clot forms in an artery. It can stop blood from reaching important organs like the heart or brain. Knowing the causes, symptoms, and risks is key to getting the right treatment fast.
Key Takeaways
- Arterial thrombosis is a serious condition that restricts blood flow to vital organs.
- It can lead to cardiovascular emergencies, including heart attacks and strokes.
- Prompt diagnosis and treatment are critical for managing arterial thrombosis.
- Understanding the causes and symptoms is essential for effective management.
- Liv Hospital is dedicated to providing top-notch care for patients with arterial thrombosis.
Understanding Arterial Thrombosis: What Is a Blood Clot in an Artery?
Arterial thrombosis happens when a blood clot forms in an artery. This can lead to heart attacks and strokes. We will look into what it is, how it happens, and its effects.
Definition and Basic Mechanism
Arterial thrombosis is mainly caused by atherosclerosis. This is when fatty deposits build up in arteries, making them hard and narrow. This buildup can lead to a blood clot forming.
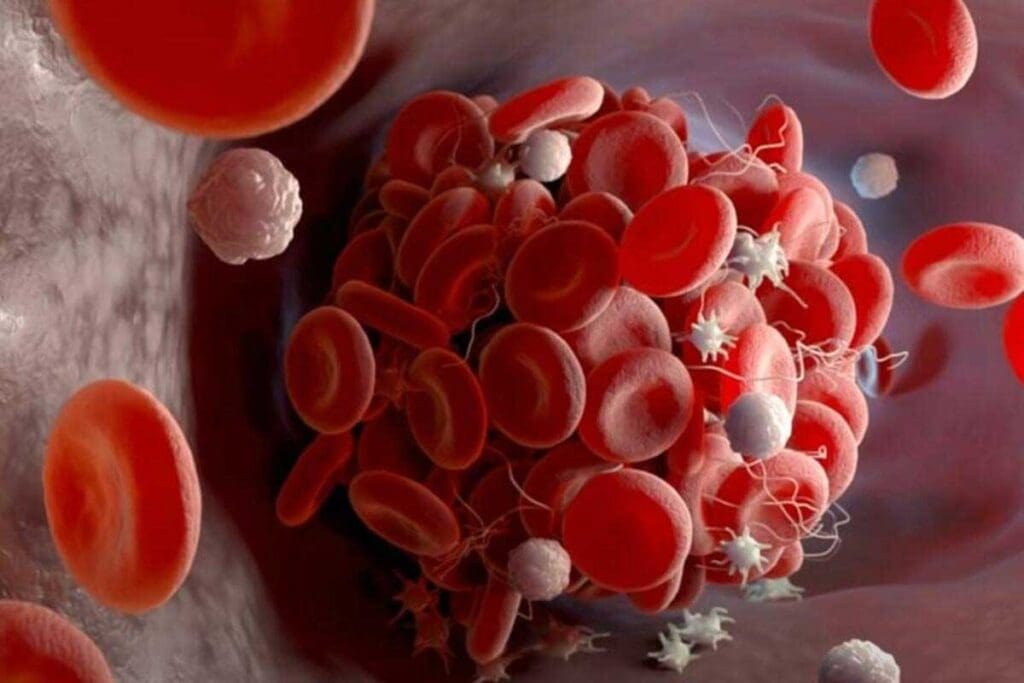
When atherosclerotic plaque ruptures, it exposes blood to highly thrombogenic material. This triggers platelet activation and aggregation. The clotting cascade starts, forming a thrombus.
Arterial thrombosis involves many factors, like plaque rupture and platelet activation. Atherosclerosis is the main condition that leads to arterial clots. Knowing this helps us understand the risks and effects of arterial thrombosis.
Difference Between Arterial and Venous Clots
Arterial clots are different from venous clots in many ways. Arterial clots are rich in platelets and can cause sudden ischemic events. They are in the arteries, which supply oxygen to vital organs. Venous clots, on the other hand, are more fibrin-rich and usually happen in the deep veins of the legs.
| Characteristics | Arterial Clots | Venous Clots |
| Composition | Rich in platelets | More fibrin-rich |
| Location | Arteries | Deep veins (often in legs) |
| Clinical Implications | Acute ischemic events (heart attack, stroke) | Deep Vein Thrombosis (DVT), potentially leading to Pulmonary Embolism (PE) |
Prevalence and Global Impact
Arterial thrombosis is a major cause of illness and death worldwide. Heart attacks and strokes, often caused by arterial thrombosis, are among the top killers globally. Risk factors like hypertension, diabetes, and high cholesterol increase the chance of these events.
The impact of arterial thrombosis is huge, with big costs to healthcare and the economy. Knowing how common it is and its risk factors is key to preventing and treating it. We need to understand these to manage risk and plan care.
The Formation Process: How Arterial Blood Clots Develop
It’s important to know how arterial blood clots form. This knowledge helps us find better ways to prevent and treat them. The process involves many factors and cell actions.
The Role of Plaque Rupture
An arterial blood clot often starts with a plaque rupture. This rupture exposes the lipid core to the blood. This triggers the clotting process.
Plaque rupture can happen for many reasons. These include inflammation, mechanical stress, or erosion. The body’s natural response to injury starts, leading to platelet buildup and clot formation.
Platelet Activation and Aggregation
After plaque rupture, platelet activation is key in forming an arterial thrombus. Platelets stick to the injury site, get activated, and send out signals for more platelets.
Platelet aggregation is helped by von Willebrand factor and fibrinogen. As more platelets gather, a platelet plug forms. This plug can quickly block the artery.
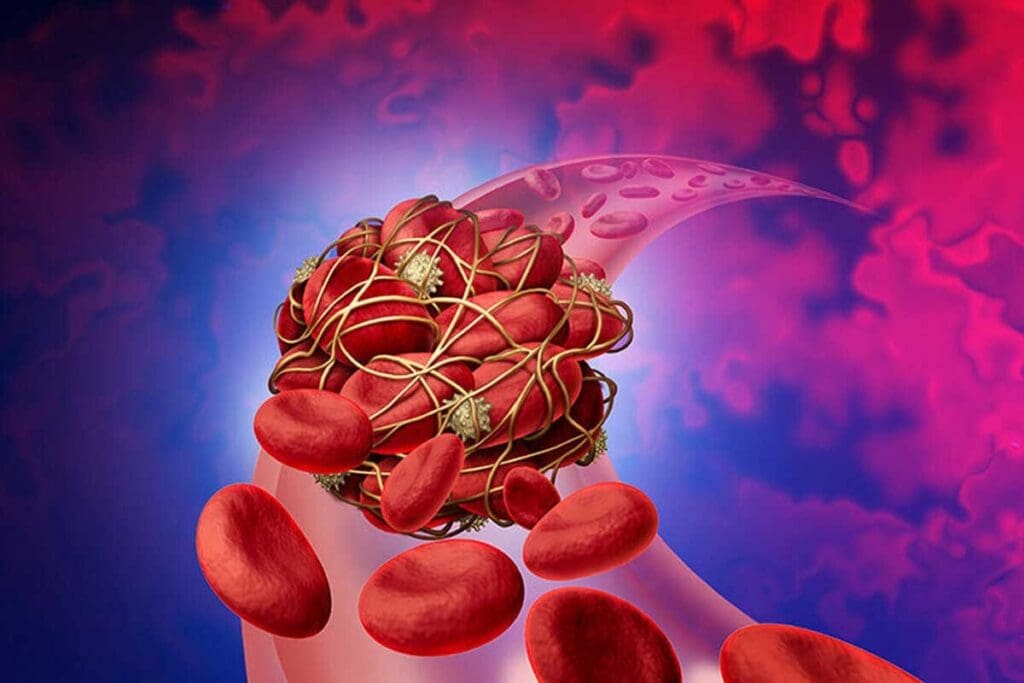
Clotting Cascade and Thrombus Formation
The clotting cascade is a series of reactions that lead to a fibrin clot. It starts when tissue factor, exposed by rupture, meets blood.
The coagulation cascade uses both the intrinsic and extrinsic pathways. These paths merge to activate thrombin and change fibrinogen into fibrin. The fibrin meshwork makes the platelet plug stable, forming a permanent thrombus that blocks the artery.
Understanding these steps is key to creating targeted treatments for arterial thrombosis. By tackling the root causes of clotting, we can lower the risk of heart problems and improve patient outcomes.
Primary Causes of Arterial Thrombosis
It’s important to know what causes arterial thrombosis to prevent and treat it. Arterial thrombosis happens when a blood clot forms in an artery. This can lead to serious heart problems. We’ll look at the main reasons why arterial thrombosis occurs.
Atherosclerosis and Plaque Buildup
Atherosclerosis is a big reason for arterial thrombosis. It’s when plaque builds up in artery walls, which can cause clots. Atherosclerotic plaque is made of fat, cholesterol, and other blood substances. When it ruptures, it can start a clotting process.
Things like a high-fat diet, smoking, and obesity can lead to atherosclerosis. It’s key to manage these risk factors to stop plaque buildup and prevent thrombosis.
Trauma and Injury to Arterial Walls
Arterial walls can get injured, leading to thrombosis. When an artery is hurt, the inner layer gets damaged. This exposes the blood to substances that start clotting.
The severity of the injury affects how likely and how big the clot will be.
Hypercoagulability Conditions
Hypercoagulability makes blood clot more easily, raising the risk of thrombosis. These conditions can be inherited or caused by other factors. Inherited ones include factor V Leiden mutation and antithrombin III deficiency. Acquired ones might come from cancer or certain medications.
Inflammatory Processes
Inflammation is also a key player in arterial thrombosis. It makes the blood more likely to clot by changing the surface of cells. This can lead to more platelets sticking together, forming clots.
Conditions like rheumatoid arthritis can increase the risk of heart problems. Fighting inflammation with lifestyle changes and medicine can help lower this risk.
Major Risk Factors for Developing Arterial Thrombi
Arterial thrombi form due to many factors. Some can be changed, while others can’t. Knowing these factors helps in preventing and managing arterial thrombosis.
Modifiable Risk Factors
Several things can increase the risk of arterial thrombi. These include hypertension, hypercholesterolemia, smoking, diabetes, obesity, and a sedentary lifestyle. Changing these through lifestyle and medicine can lower the risk of arterial thrombosis.
- Hypertension: High blood pressure damages arteries, making them prone to clots.
- Hypercholesterolemia: High cholesterol leads to plaque buildup, raising thrombosis risk.
- Smoking: It harms the heart and increases clot risk.
- Diabetes: It damages blood vessels and nerves, raising thrombosis risk.
- Obesity: It leads to hypertension and diabetes, increasing cardiovascular risk.
- Sedentary Lifestyle: Lack of activity contributes to obesity, hypertension, and other risks.
Non-Modifiable Risk Factors
Some risk factors can’t be changed. These include age, family history, and genetic predisposition. Knowing these is key to assessing risk and taking preventive steps.
- Age: Risk increases with age, after 45 in men and 55 in women.
- Family History: A history of heart disease raises individual risk.
- Genetic Predisposition: Some genes affect blood clotting, increasing thrombosis risk.
Healthcare providers can tailor prevention and treatment plans by understanding both types of risk factors.
Recognizing Artery Thrombosis Symptoms
It’s key to know the signs of artery thrombosis. These signs can change based on where the clot is. We’ll look at common warning signs and symptoms that point to an arterial thrombus in specific areas.
General Warning Signs
Artery thrombosis shows itself in many ways. You might feel sudden severe pain, numbness or tingling, or your skin could feel cold. The skin might also look pale or blue because of less blood flow.
Some people notice weakened pulses or a big difference in pulse strength between limbs. These signs mean you might have an arterial thrombosis and need to see a doctor right away.
Location-Specific Symptoms
The symptoms of artery thrombosis change based on where the clot is. For example, a clot in the heart’s arteries can cause a heart attack. This is marked by chest pain, shortness of breath, and serious heart rhythm problems.
Clots in limb arteries can cause pain at rest, pain during exercise (claudication), and reduced mobility. In bad cases, this can lead to critical limb ischemia. The limb then feels cold, pale, and very painful.
| Location of Clot | Common Symptoms |
| Heart | Chest pain, shortness of breath, arrhythmias |
| Limbs | Pain at rest, claudication, reduced mobility |
| Brain | Stroke symptoms: facial drooping, speech difficulties, sudden weakness |
Knowing these symptoms is key for quick diagnosis and treatment. We stress the need to get medical help fast if you notice any of these signs.
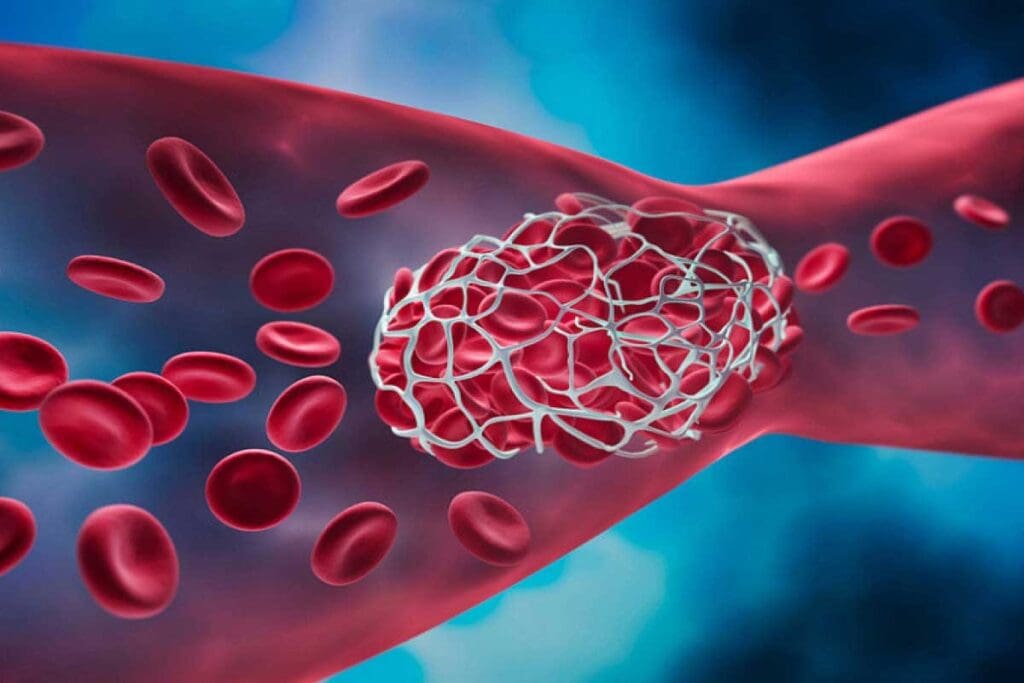
Blood Clot in Artery of Leg: A Critical Concern
Arterial thrombosis in the leg can lead to acute limb ischemia. This is a serious condition with severe outcomes. A blood clot in the leg artery is a medical emergency that needs quick diagnosis and treatment.
Unique Symptoms of Leg Arterial Clots
Symptoms of a blood clot in the leg artery include severe pain and pale skin. You might also feel numbness or tingling. These signs, known as the “six Ps,” are key indicators of acute limb ischemia.
It’s vital to recognize these symptoms early. If you or someone else has them, seek medical help right away.
Acute Limb Ischemia
Acute limb ischemia happens when blood flow to a limb suddenly stops. This is often due to an arterial clot. It can cause severe pain and permanent damage if not treated quickly.
“Time is muscle, and in the case of acute limb ischemia, timely intervention is critical to save the limb and restore function.”
Potential for Limb Loss
A blood clot in the leg artery can lead to limb loss. If acute limb ischemia is not treated quickly, it can cause gangrene. This might require amputation.
| Symptom | Description |
| Pain | Severe pain in the affected limb |
| Pallor | Pale skin due to reduced blood flow |
| Pulselessness | Absence of pulse in the affected limb |
Treatment Urgency
Treating a blood clot in the leg artery is urgent. Quick medical action is needed to restore blood flow. This prevents tissue damage and long-term problems.
Immediate action is required if symptoms don’t get better or get worse. Calling emergency services or getting to a doctor fast can save a life and prevent limb loss.
If your legs look different in color and you have severe pain or numbness, it’s a medical emergency. Call 999 right away.
Blood Clot of the Heart: Understanding Coronary Thrombosis
Coronary thrombosis, or a blood clot of the heart, is a serious condition. It happens when a clot blocks a coronary artery. These arteries are key because they carry blood to the heart muscle.
When a clot forms, it can cut off blood flow. This can lead to a heart attack.
Mechanism of Heart Attacks
A heart attack happens when blood flow to the heart is blocked. This blockage damages or kills the heart muscle. It’s usually caused by a blood clot in atherosclerosis inside a coronary artery.
The blockage can be full or partial. A full blockage causes more damage.
The process starts with atherosclerotic plaque rupture. Then, platelets activate and aggregate. This leads to a thrombus that blocks the artery.
Recognizing Heart Attack Symptoms
It’s important to know the symptoms of a heart attack. Symptoms include chest pain or discomfort, feeling weak, and shortness of breath. Other symptoms are pain in the arms or shoulder, and nausea or vomiting.
Not everyone has all these symptoms. Some may have others. Acting quickly is key if these symptoms are seen.
Immediate Response Protocols
If a heart attack is suspected, act fast. Call emergency services right away. Chewing an aspirin (if not contraindicated) can help by reducing the clot’s size.
Stay calm and stay put to reduce the heart’s workload.
Long-term Cardiac Implications
Surviving a heart attack means managing cardiac health long-term. We help patients manage risk factors. This includes lifestyle changes and medication if needed.
Adopting a healthy diet, exercising more, quitting smoking, and managing blood pressure and diabetes are key. Long-term care is vital to prevent further issues and improve life quality after a heart attack.
We focus on care that covers physical and emotional recovery.
Diagnostic Approaches for Arterial Thrombotic Disease
Healthcare professionals use many tools to diagnose arterial thrombotic disease. These include physical exams, lab tests, and imaging. This detailed method helps accurately identify and treat the condition.
Initial Assessment and Physical Examination
The first step is a thorough check-up and physical exam. We look for signs of arterial thrombosis like chest pain or limb issues. A detailed medical history and physical exam help guide further tests.
Laboratory Tests
Laboratory tests are key in diagnosing arterial thrombotic disease. Blood tests check for troponin levels, which show heart damage. Other tests look at coagulation and inflammation. A study on the National Center for Biotechnology Information website highlights their importance.
Imaging Techniques
Imaging is vital for seeing where and how big arterial clots are. We use:
- Electrocardiogram (ECG): To check heart rhythm and look for signs of trouble.
- Computed Tomography (CT) scans: To see the coronary arteries and find clots or other issues.
- Magnetic Resonance Imaging (MRI): To check heart function and find ischemia or infarction.
Together, these methods help doctors accurately diagnose and treat arterial thrombotic disease. This leads to better patient outcomes.
Treatment Options for Arterial Blood Clots
Dealing with arterial blood clots requires a mix of emergency care, medicine, and surgery. The right treatment depends on where the clot is, how big it is, and the patient’s health.
Emergency Interventions
When an arterial thrombosis happens suddenly, quick medical help is key. These emergency steps aim to quickly get blood flowing again to avoid damage. Thrombolysis, which uses medicines to break down the clot, is a common first step.
A study in the Journal of the American College of Cardiology shows that fast thrombolysis can greatly help patients with acute limb ischemia.
“Prompt restoration of blood flow is critical in managing acute arterial occlusion, and thrombolytic therapy can be an effective bridge to more definitive treatments.”
— Interventional Cardiologist
Medication Approaches
Medicine is vital in treating arterial blood clots. Anticoagulants stop the clot from getting bigger and new ones from forming. Antiplatelet agents prevent platelets from sticking together. Antithrombotic therapy is key for both short-term and long-term care of arterial thrombosis.
| Medication Type | Function | Examples |
| Anticoagulants | Prevent clot growth and new clot formation | Heparin, Warfarin |
| Antiplatelet Agents | Inhibit platelet aggregation | Aspirin, Clopidogrel |
| Thrombolytics | Dissolve existing clots | Alteplase, Tenecteplase |
Surgical and Endovascular Procedures
For many, surgery or endovascular methods are needed to clear or bypass the clot. Endovascular procedures, like angioplasty and stenting, are less invasive ways to open up blood flow.
Surgical thrombectomy removes the clot directly, used when other methods don’t work. The choice between surgery and endovascular methods depends on the patient’s health and the clot’s details.
We know each patient is different, so we tailor treatments to fit their needs. By using emergency care, medicines, and surgery or endovascular methods, we can manage arterial blood clots well and improve patient results.
Prevention Strategies: Reducing Your Risk of Arterial Clots
Preventing arterial clots is possible with healthy habits and medical care. Knowing your risk factors and acting early can lower your chance of getting clots.
Lifestyle Modifications
Changing your lifestyle can help fight heart disease. Eat a diet full of fruits, veggies, and whole grains. Also, stay active with regular exercise.
Dietary Recommendations:
- Eat more omega-3s from fish and nuts.
- Reduce saturated fats and cholesterol.
- Choose foods rich in fiber and antioxidants.
Exercise Guidelines:
- Do at least 150 minutes of moderate exercise weekly.
- Do strength training twice a week.
Medical Management of Risk Factors
Managing risk factors like high blood pressure, diabetes, and high cholesterol is key. Work with your doctor to keep these under control.
| Risk Factor | Management Strategy |
| Hypertension | Regular blood pressure checks, follow medication, make lifestyle changes |
| Diabetes | Check blood sugar, use insulin, adjust diet |
| High Cholesterol | Monitor cholesterol, take statins, change diet |
Prophylactic Medications
Some people might need medicines to prevent clots. These include antiplatelet and anticoagulant drugs.
Regular Screening for High-Risk Individuals
Screening is vital for those with heart disease history or risk factors. Early action can lead to better health outcomes.
By following these steps, you can lower your risk of arterial clots. This helps keep your heart healthy.
Conclusion: The Importance of Awareness and Prompt Action
Knowing about arterial thrombosis can save lives. It’s important to understand its causes, symptoms, and risks. This knowledge helps people get medical help quickly, which can stop serious heart problems.
Acting fast is key when dealing with arterial thrombosis. Spotting early signs and knowing who’s at risk helps people protect their heart health. We stress the need for being aware and getting medical help right away to avoid the worst of arterial thrombosis.
By focusing on heart health, people can lower their risk of getting arterial thrombosis. This means living a healthy lifestyle, managing risk factors, and seeing doctors regularly. Being aware and acting quickly are essential to fight against arterial thrombosis and save lives.
FAQ
What is arterial thrombosis?
Arterial thrombosis is when a blood clot forms in an artery. This can block blood flow to important organs like the heart or brain.
What causes arterial thrombosis?
It’s mainly caused by atherosclerosis, where fatty deposits build up on artery walls. This makes the arteries hard and narrow. Other causes include injury, conditions that make blood clot too easily, and inflammation.
What are the symptoms of arterial thrombosis?
Symptoms depend on where the clot is. Common signs are pain, numbness, and weakness. For heart clots, you might feel chest pain. Brain clots can cause neurological problems. Leg clots lead to limb pain.
What is the difference between arterial and venous clots?
Arterial clots block blood flow to vital organs, leading to heart attacks and strokes. Venous clots cause deep vein thrombosis and pulmonary embolism by blocking veins.
How is arterial thrombosis diagnosed?
Doctors first do a physical check and lab tests like troponin levels. They also use imaging like ECG, CT scans, and MRI.
What are the treatment options for arterial thrombosis?
Treatments include emergency care, medicines, and surgery or endovascular procedures. These aim to restore blood flow and prevent more problems.
How can I reduce my risk of developing arterial clots?
To lower your risk, make lifestyle changes like eating right and exercising. Manage health issues like high blood pressure and diabetes. Take preventive medicines and get screened if you’re at high risk.
What are the risks associated with blood clots in the arteries of the leg?
Leg artery clots can lead to acute limb ischemia. This is a serious condition that can cause limb loss if not treated quickly.
What is coronary thrombosis?
Coronary thrombosis is a blood clot in the coronary arteries. It can cause a heart attack by cutting off blood to the heart muscle.
How can I recognize the symptoms of a heart attack?
Heart attack signs include chest pain or discomfort, shortness of breath, and feeling lightheaded. You might also feel pain in your arms, back, neck, jaw, or stomach.
What is the importance of an immediate response to a heart attack?
Quick action is key to protecting the heart muscle and improving survival chances. Call emergency services and start first aid right away.
References:
- Faheem, M. S. B., et al. (2025). Trends in ischemic heart disease and thromboembolism. Thrombosis Research, 248, 45–52. https://www.sciencedirect.com/science/article/abs/pii/S0049384825002324









