What Is Microbiology?
Microbiology is the study of microscopic organisms bacteria, viruses, fungi, and parasites that can influence your health. In a hospital or clinic, microbiology is not just a science; it is a daily medical service that helps your care team find the exact cause of infection and select the most effective treatment.
When you experience symptoms like fever, cough, painful urination, sore throat, wound redness, or gastrointestinal upset, your clinician often relies on clinical and medical microbiology tests to confirm the diagnosis and guide therapy promptly.

For patients, the benefits are immediate. Microbiology testing can shorten illness, reduce complications, and help avoid unnecessary antibiotics. Accurate results support targeted treatment, which protects your normal flora (the helpful microbes that live on and in your body) and reduces side effects.
This approach also supports antimicrobial stewardship, a hospital wide effort to use antibiotics responsibly so they remain effective when truly needed.
You might need microbiology testing if your symptoms persist or worsen, if you are immunocompromised, pregnant, recovering from surgery, living with chronic conditions like diabetes, or recently returned from travel.
Your clinician will explain which samples are needed such as blood, urine, sputum, stool, or a throat or wound swab how the sample is collected, and when to expect preliminary and final results. If you are unsure whether you need testing, ask your care team. The earlier a correct diagnosis is made, the faster you can feel better.

Medical Microbiology in Hospitals: How Lab Testing Guides Safe, Effective Treatment
Medical microbiology connects your clinical picture with precise lab methods to diagnose, treat, and prevent infectious diseases. This service is essential across emergency care, inpatient units, outpatient clinics, surgery, obstetrics, oncology, and pediatrics. Core elements include:
Culture and identification
A culture grows microorganisms from your sample on specific media so the lab can identify the pathogen. “What is microbiology culture?” In practical terms, culture is the gold standard for many infections because it enables exact identification and subsequent antibiotic testing. If a culture report says “no growth,” your clinician will consider timing, prior antibiotics, and whether a viral or non infectious cause is more likely.
Rapid tests (antigen and molecular PCR)
Rapid antigen tests and PCR detect parts of the pathogen or its genetic material quickly. They are often used for respiratory infections (like influenza and COVID-19), strep throat, and certain gastrointestinal pathogens, providing answers when time is critical.
Antimicrobial susceptibility testing and MIC
After the organism is identified, antimicrobial susceptibility testing determines which antibiotics are effective. The report may include MIC in microbiology (Minimum Inhibitory Concentration), the lowest antibiotic concentration that prevents visible growth. Your results are summarized as “susceptible,” “intermediate,” or “resistant,” guiding a safe and effective prescription.
Blood cultures and sepsis support

For high fevers, low blood pressure, or suspected sepsis, blood cultures look for bacteria or fungi in the bloodstream. Early detection and targeted treatment can be lifesaving. Critical results are communicated urgently to your clinicians.
Infection prevention and control
Medical microbiology collaborates with infection prevention teams to monitor resistant organisms, guide isolation precautions, and reduce hospital acquired infections. This protects patients, visitors, and staff.
Stewardship and follow up
As results evolve from preliminary to final, your care team may adjust therapy. Antimicrobial stewardship ensures the narrowest effective antibiotic is used for the right duration, balancing rapid recovery with long term protection against resistance.
Clinical Microbiology: From Sample Collection to Actionable Results

Clinical microbiology ensures that every test leads to clear decisions for patient care. The process includes:
Ordering the right test
Your clinician selects tests based on your symptoms, exam, and medical history. Testing at the right time increases accuracy and reduces the chance of false negatives.
Proper sample collection
Results are only as good as the specimen. A clean catch midstream urine sample reduces contamination. A properly collected sputum sample (deep cough) is more informative than saliva. Blood
culture collection requires careful skin antisepsis. If you have a wound, a sample is taken from viable tissue where microbes are most likely to be found.
Transport and handling
Samples are transported promptly under the correct conditions. Some pathogens require special containers or temperatures to remain viable.
Laboratory analysis
The lab uses microscopy, Gram stain, culture, biochemical tests, immunoassays, and molecular diagnostics. For example, a Gram stain test in microbiology rapidly suggests whether bacteria are Gram positive or Gram negative, which informs early therapy while culture grows.
Interpretation and reporting
Microbiology specialists interpret findings in the context of your medications, imaging, and overall health. Reports use standardized terms so your care team can act quickly.
Communication and next steps
Critical values are called to your provider. If your report changes from preliminary to final, you may receive an updated plan such as narrowing or changing antibiotics, considering antivirals, or focusing on supportive care if no pathogen is detected.
What Is a Pure Culture in Microbiology? Why Purity Matters for Accurate Results
A pure culture in microbiology contains only one type of microorganism. Achieving purity is essential for accurate identification and antibiotic testing. Mixed or contaminated samples can obscure the true cause of infection and lead to delays or less precise therapy.
How labs achieve purity:
- Aseptic technique during collection reduces contamination.
- Streaking samples on agar plates helps isolate individual colonies.
- Technologists examine colony appearance (shape, color, hemolysis) to select a single colony for
definitive testing.
For you, pure culture means confidence: the identified organism and its susceptibility profile truly reflect
what is causing your symptoms, supporting a targeted and effective treatment plan.
What Is MIC in Microbiology? How Antibiotic “Susceptible vs Resistant” Is Decided
MIC stands for Minimum Inhibitory Concentration the lowest concentration of an antibiotic that stops visible bacterial growth in the lab. MIC values are compared with standardized breakpoints to label organisms as susceptible (S), intermediate (I), or resistant (R).
This helps your clinician:
- Choose the right antibiotic for the organism.
- Adjust dosing for certain infections or sites (for example, urine vs lung).
- Avoid ineffective medications, reducing side effects and preserving gut flora.
- MIC is one part of the overall picture. Your clinician also considers allergy history, kidney and liver function, other medications, infection site, and severity to personalize therapy.
What Is a Colony in Microbiology? Understanding Culture Plates and CFU
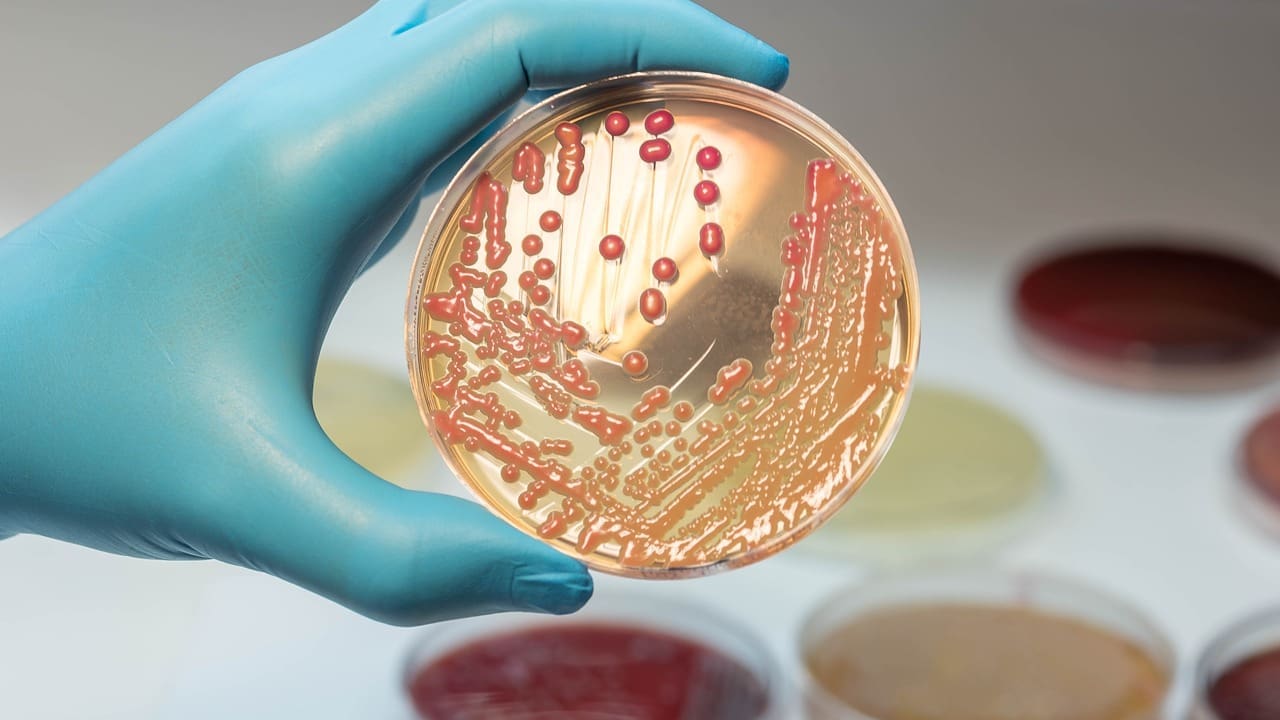
A colony is a visible cluster of microorganisms that typically arises from a single cell on a solid agar surface. Colony characteristics size, color, shape, edge, elevation, odor, and hemolysis offer early clues to identity. The lab also measures CFU in microbiology (colony-forming units) to estimate the number of viable organisms.
In urine cultures, CFU per milliliter helps distinguish contamination from true infection. For example, a high CFU count with urinary symptoms supports a UTI diagnosis and targeted treatment.
For patients, colony counts and characteristics are not just technical details they influence whether treatment is necessary, which drug is chosen, and how long therapy should last.
What Does a Microbiology Specialist Do?
Your hospital microbiology service includes clinical microbiologists, medical laboratory scientists, and
infectious disease physicians who:
- Advise on the right tests and timing based on your symptoms.
- Ensure proper specimen collection and transport to preserve accuracy.
- Perform Gram stains, culture, molecular PCR, antigen tests, and susceptibility testing.
- Interpret results in the context of your health and medications.
- Communicate critical values promptly and support antimicrobial stewardship.
- Collaborate with infection prevention to reduce hospital acquired infections.
This teamwork means your care is informed by timely, accurate, and clinically relevant data at every step.
Liv Hospital Microbiology
Liv Hospital’s Microbiology Laboratory stands out as an international standard facility equipped with state of the art equipment. Its experienced staff consisting of expert microbiologists ensures the rapid and accurate diagnosis of diseases with their meticulous studies.
Our laboratory has achieved successful studies by using a wide range of tests and modern techniques and has become a reliable reference point in the healthcare sector. Liv Hospital Microbiology Laboratory maintains its leadership in the healthcare sector by providing uninterrupted and high quality service to its patients with its innovative approaches.

Tests Performed in the Microbiology Laboratory of Liv Hospital:
- Culture tests
- Bacterial identification tests
- Antibiotic and Antifungal susceptibility tests
- Antibiotic resistance research
- Direct microscopic examinations
- Stained preparation examinations
- Search for parasite eggs in feces
- Antigen screening tests
- Antibody tests (serological tests)
- PCR (Polymerase Chain Reaction)
For more information about our academic and training initiatives, visit Liv Hospital Academy.
Frequently Asked Questions for Microbiology
Do I need to prepare for tests?
Most tests require no fasting. For urine culture, follow clean catch instructions to reduce contamination. Always follow your clinician’s guidance.
What is biofilm in microbiology?
A biofilm is a protective community of microbes on surfaces (like catheters or wounds). It can reduce antibiotic effectiveness, so your team may adjust therapy or remove devices.
Is microbiology hard to understand?
It can be technical, but your team will explain your results in clear, practical terms.
What does a microbiology specialist do?
They guide test selection, ensure quality, interpret results, support stewardship, and collaborate with your clinicians on treatment decisions.
How do labs choose the right antibiotic?
Through antimicrobial susceptibility testing and MIC values, reported as susceptible, intermediate, or resistant.
Why might a culture show “no growth”?
Possible reasons include prior antibiotics, early collection, low organism numbers, or a non bacterial cause. Your clinician may repeat or adjust testing.
How long do microbiology results take?
Rapid tests may return the same day; most bacterial cultures take 24–72 hours. Some organisms need longer. Your clinician will explain timing.



