pluripotent stem cells
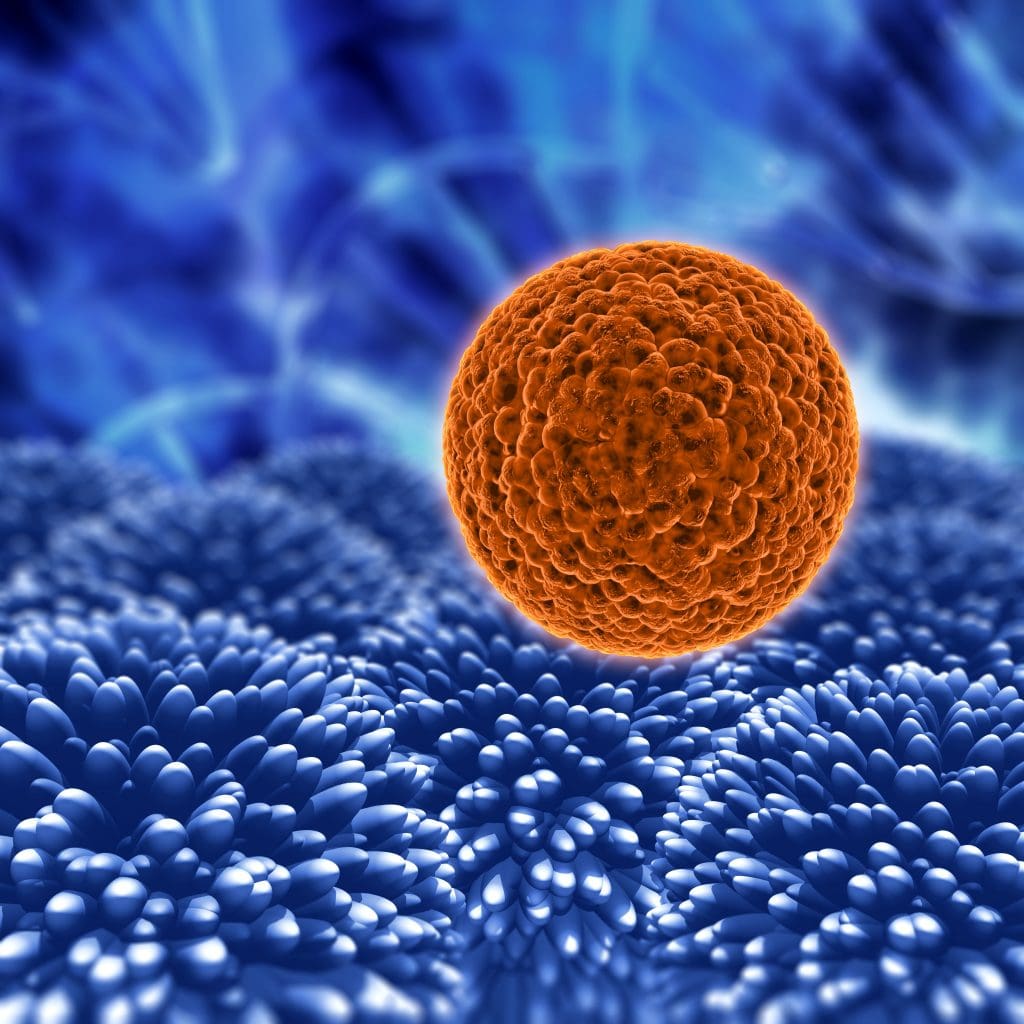
Embryonic stem cells (ESCs) are found in the inner cell mass of the human blastocyst, an early stage of the developing embryo. These remarkable cells are capable of differentiating into any cell type, making them extremely valuable for medical research and potential treatments.
The ability of ESCs to become different cell types is a big plus in regenerative medicine. Scientists are looking into how they can help fix or replace damaged tissues through cell therapy.
Key Takeaways
- Embryonic stem cells are derived from the inner cell mass of the human blastocyst.
- They have the ability to differentiate into any cell type.
- ESCs are valuable for medical research and possible treatments.
- Their versatility is a big plus in regenerative medicine.
- Scientists are exploring their use in cell therapy.
The Science Behind Embryonic Stem Cells
embryonic stem cells
These remarkable cells are capable of differentiating into any cell type, making them extremely valuable for medical research and potential treatments.
Definition and Biological Properties
These remarkable cells are capable of differentiating into any cell type, making them extremely valuable for medical research and potential treatments.
These cells can grow forever in a lab, staying pluripotent under the right conditions. This is key for their use in medical research and treatments.
Sources and Extraction Methods
ESCs usually come from the inner cell mass of blastocysts, which are very early embryos. Getting ESCs involves several steps, like immunosurgery to remove the outer layer of the blastocyst. This step is where the embryo is destroyed, raising ethical questions.
Experts say getting ESCs from human embryos is a big ethical issue. It brings up questions about the value of embryos and the risk of misuse. The methods for getting ESCs have gotten better over time. Researchers are working hard to make these methods more efficient and less ethically complex.
Pluripotent Stem Cells: Nature’s Versatile Building Blocks
pluripotent stem cells differentiation pathways
Pluripotent stem cells are amazing because they can grow and change into many types of cells. This makes them very important in science today. They can keep growing forever, giving us lots of cells for study and treatments.
Self-Renewal and Proliferation Capabilities
These cells can keep themselves growing, staying the same but multiplying. This is key for keeping stem cells alive for a long time. It’s all about how the cells talk to each other and what signals they get.
Key factors influencing self-renewal include:
- Transcription factors such as OCT4 and SOX2
- Signaling pathways like Wnt/β-catenin and Notch
- Epigenetic modifications that maintain the pluripotent state
They can also grow a lot, which is great for making lots of cells. This is useful for fixing damaged tissues and finding new medicines.
Differentiation Pathways and Cellular Lineages
These remarkable cells are capable of differentiating into any cell type, making them extremely valuable for medical research and potential treatments.
| Germ Layer | Derived Cell Types | Potential Applications |
| Ectoderm | Neurons, glial cells, skin cells | Neurological disorders, skin regeneration |
| Mesoderm | Cardiomyocytes, skeletal muscle cells, blood cells | Cardiovascular diseases, muscular dystrophy, hematological disorders |
| Endoderm | Pancreatic cells, lung epithelial cells, liver cells | Diabetes, respiratory diseases, liver disorders |
The ways these cells change into different types is very complex. Knowing how they do this is key to using them for fixing damaged tissues.
Historical Milestones in Embryonic Stem Cell Research
Starting in the late 1990s, embryonic stem cell research has seen many key moments. These moments have changed how we see developmental biology and regenerative medicine.
In 1998, a team at the University of Wisconsin created the first human embryonic stem cell (ESC) lines. This was a big step forward. It let scientists study human development and disease in new ways.
Breakthrough Discoveries
These remarkable cells are capable of differentiating into any cell type, making them extremely valuable for medical research and potential treatments.
Being able to control how ESCs turn into specific cells has opened up new paths for regenerative medicine. Researchers have made big strides in figuring out how to guide ESCs to become certain cell types.
| Year | Milestone | Significance |
| 1998 | First human ESC lines established | Enabled study of human development and disease modeling |
| 2000s | Differentiation of ESCs into various cell types | Advancements in regenerative medicine and tissue engineering |
| 2010s | Development of protocols for directed differentiation | Improved efficiency and specificity in generating therapeutic cells |
These historical milestones show how fast stem cell research has grown. As we keep learning more, the ways ESCs can help medicine and science will grow too.
Regenerative Medicine Applications
regenerative medicine applications
ESCs have a huge role in regenerative medicine. They can help fix damaged tissues and even grow new organs. This is because they can turn into many different cell types.
Tissue Repair Mechanisms
Fixing damaged tissues is key in regenerative medicine. ESCs are a big help here. They can become specific cells to fix or replace damaged areas.
For example, they can become heart cells to fix the heart or brain cells to treat brain diseases.
- Cell Replacement Therapy: ESCs can replace damaged cells, fixing tissue function.
- Tissue Engineering: ESCs can be mixed with materials to create new tissue substitutes.
- Paracrine Effects: ESCs can help nearby tissues by releasing growth factors and cytokines.
Whole Organ Regeneration
Creating new organs is a big dream in regenerative medicine. ESCs are a big part of this dream. Making real organs in the lab could solve the organ shortage problem.
- ESCs can grow into organoids, which are like mini-organs.
- Using materials and engineering can help build complex organs.
- Creating new organs could help many diseases, like heart failure or liver disease.
In short, ESCs are changing regenerative medicine. They offer new ways to fix tissues and grow new organs. As research goes on, ESCs will likely help even more people with serious diseases.
Cell-Based Therapies and Transplantation
cell-based therapies
Cell-based therapies are a new area in medicine using embryonic stem cells (ESCs). They aim to fix or replace damaged tissues by transplanting ESC-derived cells.
Therapeutic Cell Production
Making therapeutic cells from ESCs is a detailed process. It needs careful control over cell growth and change. Scientists are working on ways to make ESCs turn into specific cells, like brain or heart cells, for treatment.
Key steps in therapeutic cell production include:
- Directed differentiation of ESCs into desired cell types
- Expansion and culturing of cells under controlled conditions
- Purification and characterization of the final cell product
Immunological Challenges
One big challenge in cell-based therapies is the risk of the body rejecting the transplanted cells. ESC-derived cells might be seen as foreign by the immune system. So, finding ways to avoid this is important.
Immunological challenges include:
- Host immune response against transplanted cells
- Graft-versus-host disease (GVHD)
- Need for immunosuppressive therapies
Ongoing Clinical Trials
Many clinical trials are happening to check if ESC-derived cell therapies are safe and work well. These trials are key to learning about the benefits and risks of these new treatments.
Ongoing clinical trials are investigating:
- Treatment of degenerative diseases such as Parkinson’s disease
- Repair of damaged heart tissue
- Regeneration of tissues in various organs
As research goes on, the results of these trials will help us understand the future of cell-based therapies. They could change how we treat medical conditions.
Tissue Engineering Breakthroughs
tissue engineering
The use of stem cells and biomaterials has greatly advanced tissue engineering. This field now offers new ways to help people. It aims to create tissue substitutes that can fix or replace damaged tissues.
Biocompatible Scaffolds and Materials
Biocompatible scaffolds are key in tissue engineering. They help cells grow and work properly. New biomaterials are being made that are safe and strong enough for tissue repair.
What makes a good biocompatible scaffold?
- It should break down naturally
- Be porous for cell movement
- Have enough strength
- Support cell attachment well
3D Bioprinting with Stem Cells
3D bioprinting is a game-changer in tissue engineering. It lets us print out tissue structures with stem cells and materials. This method makes it possible to create tissues that fit each patient’s needs.
“3D bioprinting has the power to change tissue engineering. It can make real, working tissues for transplants and testing drugs.”
Engineered Tissues for Transplantation
The main goal of tissue engineering is to make tissues for transplant. These engineered tissues are showing great promise in early studies. They could be used to fix or replace damaged tissues in patients.
Dr. Anthony Atala, a leading researcher, says, “Making tissues and organs is a big step forward in regenerative medicine. It gives hope to those who need transplants.”
But, there are hurdles to overcome in tissue engineering. We need to make more tissue, ensure it works long-term, and deal with immune system issues. Despite these challenges, the progress in tissue engineering is exciting for the future of regenerative medicine.
Disease Modeling and Pathology Research
disease modeling using ESCs
Disease modeling with ESCs lets us study how diseases progress and test treatments safely. This method is key in biomedical science. It helps us grasp disease mechanisms and find treatments.
Recreating Disease Conditions In Vitro
ESCs can turn into different cell types. This lets researchers mimic diseases like Parkinson’s and Alzheimer’s. They can study disease pathology and test treatments in a lab.
Creating disease models in a lab is a big step forward. It helps us understand disease progression and find new treatments. A leading researcher says, “ESCs could change how we treat diseases, making treatments more effective.”
Patient-Specific Disease Models
ESCs are great for making disease models that match a patient’s condition. By turning patient cells into iPSCs and then into specific cell types, we get models that closely match the patient’s disease. This approach is key for creating treatments that fit each patient’s needs.
- Patient-specific models help us understand how diseases differ between people.
- They let us test drugs safely in a model that matches the patient’s condition.
- Using these models could lead to more personalized medicine.
Genetic Disease Investigation
ESCs are also key in studying genetic diseases. By adding specific genetic mutations to ESCs, researchers can see how these changes affect cells and disease progression. This method has helped us understand many genetic disorders and find new ways to treat them.
“The use of ESCs in modeling genetic diseases has opened new avenues for understanding the complex interplay between genetic and environmental factors in disease pathology.”
Leading Stem Cell Researcher
In summary, ESCs have changed how we study and treat diseases. They offer new ways to understand and tackle complex diseases. As research advances, we’ll find more ways to treat and possibly cure diseases.
Pharmaceutical Applications and Drug Development
ESCs are a promising tool for advancing pharmaceutical research. They are great for high-throughput drug screening and toxicity assessment. ESCs can create diverse cell types for testing drug efficacy and safety.
High-Throughput Drug Screening
High-throughput drug screening is key in drug development. It lets researchers test thousands of compounds quickly. ESCs can be turned into various cell types, making them a renewable source for screening.
This method can speed up finding promising drug candidates. Using ESCs in screening also tests drugs in a more human-like way. This can help predict how drugs will work in humans, reducing the need for animal tests.
Toxicity Assessment and Safety Testing
Toxicity assessment is vital in drug development. It helps spot safety risks in new drugs. ESCs can create cell-based assays that mimic human tissue responses, giving a better prediction of drug toxicity.
Using ESCs for toxicity testing can help find safety issues early. This reduces the risk of costly failures later on. It also improves the safety of new drugs.
Personalized Drug Response Prediction
One exciting use of ESCs is in predicting personalized drug responses. By getting ESCs from individual patients, researchers can create personalized cell models. These models reflect the unique genetic and epigenetic profiles of those patients.
These personalized cell models can predict how patients will react to specific drugs. This enables more tailored treatment approaches. It could lead to better patient outcomes.
Organoid Technology and Development
Organoids come from stem cells and are a big deal in science. They let us study how different tissues work together in a controlled space. These mini-versions of organs can act like the real thing, helping us learn and find new treatments.
Mini-Organs for Research Purposes
Organoids act as mini-organs for studying diseases. They help scientists see how diseases progress and test treatments better than flat cell cultures.
They’ve already helped us understand diseases like cancer, brain disorders, and stomach problems.
Organoids in Personalized Medicine
Organoids are also key in personalized medicine. They’re made from a patient’s cells, creating models that match the person’s health. This means treatments can be made just for them.
This could change healthcare by making treatments fit each person’s needs better.
Complex Tissue Interactions
Organoids help us study complex tissue interactions. This is important for understanding how cells in an organ talk and work together. It helps us learn about tissue growth and repair.
By studying these interactions in organoids, we can learn more about human biology and diseases. This could lead to new treatments.
In short, organoid technology is a big step forward in science. It helps us in research, personalized medicine, and understanding tissue interactions. As it grows, it promises to improve our health and disease understanding.
Neurological Applications and Brain Research
Embryonic stem cells (ESCs) are changing the game in brain research. They have the power to treat many neurodegenerative diseases. Their unique abilities make them a top choice for regenerative medicine.
One exciting area is treating Parkinson’s disease. ESCs can turn into dopamine-producing neurons, which are missing in Parkinson’s patients. Research shows that these cells can help improve movement in animal models.
Parkinson’s Disease Therapy Development
Creating treatments for Parkinson’s with ESCs involves several steps. First, ESCs are turned into dopamine-producing neurons. Then, these cells are transplanted into the brain. Researchers are also working on making these cells last longer and work better.
A recent study showed ESC-derived dopamine-producing neurons can help with movement in a primate model of Parkinson’s. This is a big step forward. It suggests ESC-based therapies could be a real solution for Parkinson’s.
Spinal Cord Injury Repair Strategies
ESCs are also being looked at for spinal cord injuries. Scientists are trying to use ESCs to help the spinal cord heal. They aim to turn ESCs into neural cells that can replace damaged ones.
| Condition | ESC-Based Therapy | Status |
| Parkinson’s disease | Dopamine-producing neurons | Preclinical trials |
| Spinal cord injury | Neural cells | Preclinical trials |
Using ESCs in brain research is very promising. It could lead to new treatments for serious conditions. But, more research is needed to unlock their full power.
Diabetes Research and Pancreatic Cell Generation
Embryonic stem cells (ESCs) are a new hope in diabetes research. They can turn into pancreatic cells, which is exciting for treating diabetes.
Generating functional beta cells is a big focus in diabetes research. Beta cells make insulin, which controls blood sugar. The loss of these cells is what causes diabetes, and finding a way to replace them could cure it.
Creating Functional Beta Cells
Scientists have made big strides in turning ESCs into beta cells. This involves many steps, like changing signaling pathways and using growth factors. The goal is to make beta cells that are just like the ones in our pancreas.
Recent studies have shown great results. For example,
“Scientists have successfully generated functional beta cells from ESCs, which were able to regulate blood sugar levels when transplanted into diabetic mice”
. These findings show ESCs could be a big help in treating diabetes.
Islet Cell Transplantation Progress
ESCs are also being looked at for islet cell transplantation. Islet cells, including beta cells, are key for managing blood sugar. Transplanting these cells into diabetic patients could help them manage their blood sugar again.
But, there are hurdles to overcome, like the need for immunosuppression to prevent rejection. Researchers are working on ways to protect these cells from being attacked by the immune system.
Addressing Autoimmunity Challenges
Autoimmunity is a big problem in using ESCs for diabetes treatment. In type 1 diabetes, the immune system attacks the body’s own beta cells. Researchers are looking at ways to stop this, like using immunosuppressive drugs and developing immune-modulating therapies.
They are also exploring ways to protect transplanted cells from the immune system. This could make it possible to transplant ESC-derived beta cells without needing to suppress the immune system for a long time.
Cancer Research and Therapeutic Development
Embryonic stem cells (ESCs) are key in cancer research. They help us understand tumors and find new treatments. ESCs can turn into different cells, helping scientists study cancer and find new ways to fight it.
Modeling Cancer Progression
ESCs are great for modeling cancer. By turning ESCs into different cells, researchers can study cancer’s early stages. This helps them understand how cancer starts and grows.
Key benefits of using ESCs for cancer modeling include:
- The ability to generate complex cellular models that mimic human cancer
- The ability to study the early stages of cancer development
- The capacity to test various therapeutic interventions
Developing Targeted Cancer Therapies
ESCs are also important for making targeted cancer treatments. By knowing how cancer works, scientists can create treatments that only harm cancer cells. ESCs help test these treatments to see if they work well and are safe.
| Therapeutic Approach | Description | Potential Benefits |
| Targeted Therapies | Drugs designed to target specific molecular mechanisms in cancer cells | Improved efficacy, reduced side effects |
| Immunotherapy | Treatments that harness the immune system to fight cancer | Enhanced immune response against cancer cells |
| Stem Cell-Based Therapies | Use of stem cells to replace or repair damaged tissues | Potential for tissue regeneration, improved organ function |
Cancer Stem Cell Research
Cancer stem cells are a special part of cancer cells. They can grow and change like normal stem cells. Studying these cells is key to understanding why cancer comes back and spreads.
The study of cancer stem cells holds promise for:
- Understanding the mechanisms of cancer recurrence
- Developing therapies that target the root cause of cancer
- Improving patient outcomes through more effective treatments
Cardiovascular Disease Treatments
Embryonic stem cells are changing how we treat heart diseases. They help fix damaged heart tissue and blood vessels. Heart diseases are a big problem worldwide, and old treatments just manage symptoms. But, stem cells can really fix the damage and make the heart work better.
Cardiac Tissue Regeneration
These remarkable cells are capable of differentiating into any cell type, making them extremely valuable for medical research and potential treatments.
Fixing heart tissue is a big job. It involves turning stem cells into heart cells and getting them to work right. Scientists are also working on better ways to keep these cells alive and working well.
Blood Vessel Formation and Repair
Stem cells might also help make new blood vessels. This is great for people with poor blood flow to their legs. New blood vessels could bring life back to tissues that don’t get enough blood.
Creating new blood vessels with stem cells could also help with organ transplants. It could make transplanted tissues work better and last longer.
Limitations and Challenges in Embryonic Stem Cell Research
Embryonic stem cells hold great promise, but they face many hurdles. These challenges are both technical and scientific. Researchers must overcome these obstacles to use these cells in medical science.
Technical and Scientific Hurdles
Keeping embryonic stem cells in a state where they can grow into different types of cells is hard. Cell culture conditions are key, but finding the right balance is a constant struggle. Also, the heterogeneity of these cells makes research and treatments tricky.
Understanding how these cells stay young and flexible is another big challenge. Molecular signaling pathways and epigenetic regulation are at the heart of this. Figuring out these processes is vital for unlocking the full power of embryonic stem cells.
Tumor Formation Risks
These remarkable cells are capable of differentiating into any cell type, making them extremely valuable for medical research and potential treatments.
To lower this risk, scientists are looking into new methods. They’re working on suicide genes that can stop tumor growth. They’re also trying to make the cells used in treatments more pure and specific to reduce tumor risks.
Comparison with Induced Pluripotent Stem Cells
Embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) are two types of stem cells. They can turn into different cell types but come from different sources. ESCs come from embryos, while iPSCs are made from adult cells.
Technical Differences and Similarities
ESCs and iPSCs are different in how they are made. ESCs come from embryos, while iPSCs are made by changing adult cells into stem cells.
Even though they come from different places, they share some key traits. Both can grow and change into many cell types. They also have similar markers like OCT4 and NANOG.
| Characteristics | ESCs | iPSCs |
| Origin | Inner cell mass of blastocysts | Somatic cells reprogrammed with transcription factors |
| Pluripotency Markers | OCT4, NANOG | OCT4, NANOG |
| Self-Renewal Ability | High | High |
Advantages and Disadvantages
ESCs are great for research because they can become any cell type. But, they raise ethical questions and can cause immune reactions.
iPSCs are seen as a better option for treatments because they avoid ethical issues. Yet, making them can lead to genetic changes, and it’s not always successful.
Key advantages of iPSCs include:
- Potential for personalized medicine
- Bypass ethical concerns associated with ESCs
- Possibility of generating disease-specific models
Disadvantages of iPSCs:
- Risk of genetic mutations during reprogramming
- Variable reprogramming efficiency
- Potential for tumor formation
In conclusion, both ESCs and iPSCs have their benefits and drawbacks. They are important in stem cell research and regenerative medicine. Knowing their differences and similarities helps us move forward in biomedical science.
Ethical and Regulatory Landscape
Embryonic stem cell research sparks a big debate. Different views come from culture, religion, and society. The use of ESCs raises big questions that change based on where you are in the world.
Ethical Considerations in Different Cultures
Culture and religion deeply affect how people see ESC research. Some see it as wrong, while others are okay with it. Cultural differences shape the global research scene.
In some places, religion plays a big role in the debate. For example, the Catholic Church doesn’t support ESC research because of its beliefs on life. But, other cultures might have more open views, allowing research under certain conditions.
| Country | ESC Research Policy | Influencing Factors |
| United States | Permissive with restrictions | Political, ethical, and religious factors |
| Germany | Restricted | Historical and ethical considerations |
| United Kingdom | Permissive with regulations | Scientific community input and legislative framework |
United States Regulatory Framework
In the U.S., ESC research rules are complex. They involve federal and state laws, plus guidelines from science and ethics groups. Federal funding for ESC research has its own rules, like the Dickey-Wicker Amendment.
Federal regulations are key in the U.S. The National Institutes of Health (NIH) sets guidelines for ESC use in federally funded research.
International Policies and Regulations
Worldwide, ESC research rules vary a lot. Some places allow it, while others ban it. International collaboration in ESC research faces these different rules.
The International Society for Stem Cell Research (ISSCR) has made guidelines for ethical stem cell research worldwide. These aim to make ethical standards and research practices the same everywhere.
The big difference in rules around the world shows we need to keep talking and working together. We must find a balance between scientific progress and ethics in ESC research.
Conclusion: The Future of Embryonic Stem Cell Applications
These remarkable cells are capable of differentiating into any cell type, making them extremely valuable for medical research and potential treatments.
The possibilities for embryonic stem cell applications are huge. Scientists are working hard to solve problems and find new ways to use them in biomedical science. As we learn more about ESCs, we’ll see big steps forward in treating diseases and injuries.
Using ESCs, scientists can change regenerative medicine for the better. This could bring new hope to those needing new treatments. Keeping up the research on embryonic stem cell applications is key to reaching their full health benefits.
FAQ
What are embryonic stem cells and what are they used for?
These remarkable cells are capable of differentiating into any cell type, making them extremely valuable for medical research and potential treatments.
How are embryonic stem cells derived and what are the ethical implications?
ESCs are taken from the inner cell mass of a blastocyst. The process of getting these cells raises ethical questions. This is because it involves using human embryos for research.
What makes pluripotent stem cells versatile?
Pluripotent stem cells, like ESCs, can grow and change into many cell types. They can become all three germ layers: ectoderm, endoderm, and mesoderm.
What are the possible uses of ESCs in regenerative medicine?
ESCs could help fix damaged tissues and even grow new organs. This could lead to new ways to treat diseases and injuries.
How are ESCs used in cell-based therapies and transplantation?
ESCs can make therapeutic cells for transplant. This could help treat many diseases. But, there are challenges like immune reactions and the risk of tumors.
What is organoid technology, and how is it related to ESCs?
Organoid technology creates mini-organs from stem cells, including ESCs. It’s used for research, personalized medicine, and studying tissue interactions.
What are the possible neurological applications of ESCs?
ESCs are being studied for treating neurodegenerative diseases like Parkinson’s. They might also help repair spinal cord injuries.
What is the role of ESCs in cancer research?
ESCs help model cancer progression and develop targeted therapies. They also help study cancer stem cells, aiding in cancer treatment.
How do ESCs compare to induced pluripotent stem cells (iPSCs)?
ESCs and iPSCs are both pluripotent but differ in how they’re made. Each has its own benefits and drawbacks.
What are the limitations and challenges in ESC research?
ESC research faces many challenges, like the risk of tumors and ethical debates. There are also technical and regulatory hurdles.
What is the current regulatory landscape for ESC research?
The rules for ESC research vary by country. Different places have different ethical views and laws, like in the U.S. and internationally.
What are the future applications of ESCs?
ESCs could greatly advance regenerative medicine and develop new treatments. They might help treat many diseases and injuries in the future.









