Last Updated on October 21, 2025 by mcelik
We are at the forefront of groundbreaking advances in medicine and research. This is thanks to the power of embryonic stem cells. These cells can grow into almost any cell type. They hold great promise for regenerative medicine and cell therapy.
Recent studies show that embryonic stem cells are used in over 115 global clinical trials. This has led to new treatments for many medical conditions. A study published on Nature highlights this. It shows how these cells help us understand germ cell development and specification. This knowledge opens up new medical strategies.
Stem cell research focuses on human embryonic cells. These cells are key to understanding how cells can change. They can grow into almost any cell type, making them very useful for research and treatments.
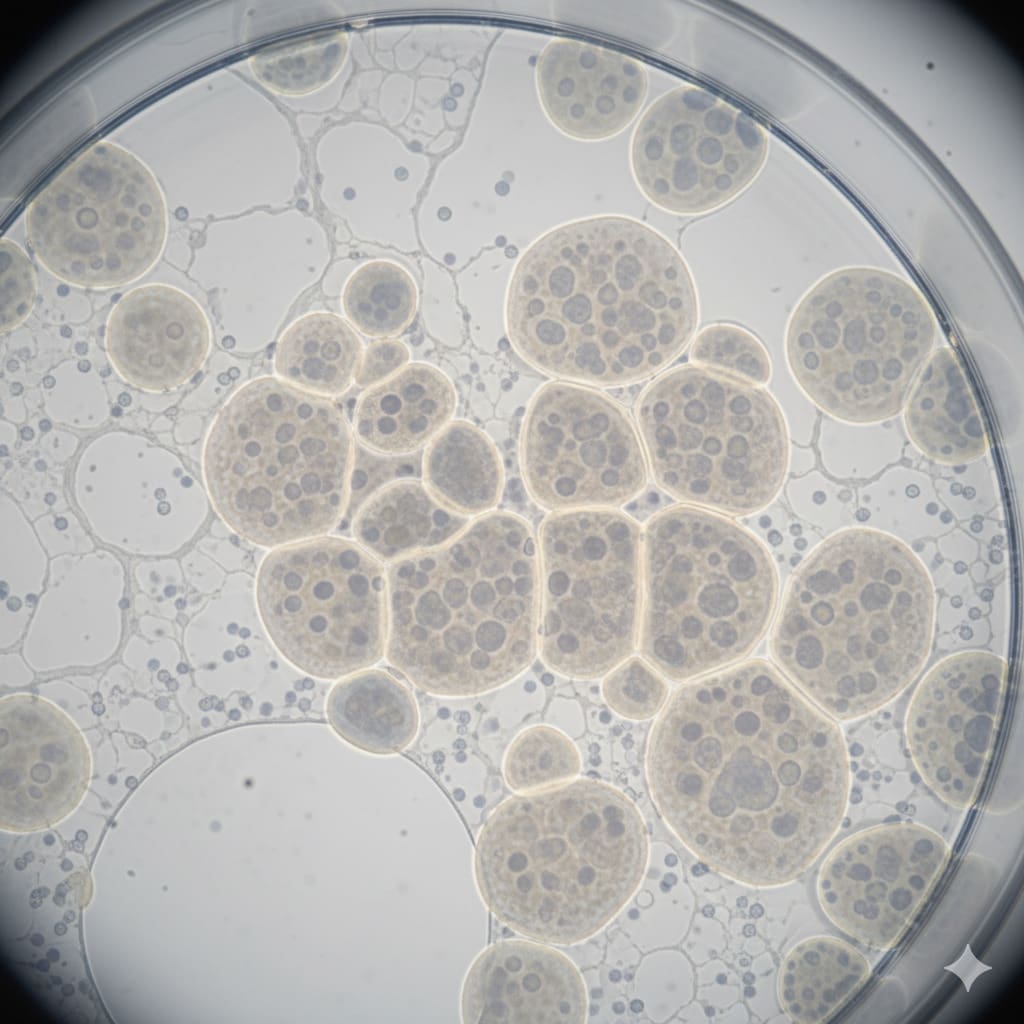
Embryonic stem cells come from the inner cell mass of a blastocyst, an early embryo. They are pluripotent, meaning they can turn into almost any cell in the body. To get these cells, scientists take the inner cell mass and grow it in a lab.
The main trait of embryonic stem cells is their pluripotency. This lets them become every type of body cell, making them very useful for research and treatments. Pluripotency is controlled by genes and other factors that help the cells grow and change.
Studies have found that cholesterol is important for these cells. It helps control how they grow, change, and move. This shows how complex these cells are.
Human embryonic cells can keep growing forever and change into different cell types. This is key for research and medicine. Growing more cells helps, and changing into specific types is useful for treatments.
The table below summarizes the key characteristics and capabilities of human embryonic stem cells:
| Characteristic | Description | Significance |
|---|---|---|
| Pluripotency | Ability to differentiate into almost any cell type | High for therapeutic uses |
| Self-Renewal | Ability to proliferate indefinitely | For making lots of cells |
| Differentiation Capability | Ability to generate specific cell types | For targeted treatments |
Understanding human embryonic cells is key for new medical treatments. As we learn more about them, their uses in medicine are growing.
Getting human embryonic cells ready for research or therapy is a detailed process. It needs careful steps to keep the cells alive and useful. Now, human embryonic stem cells are key in over 115 global clinical trials. This shows how important this work is.
Getting human embryonic stem cells from blastocysts is a delicate task. The inner cell mass of the blastocyst is carefully taken out. Then, the cells are grown in special conditions to keep them versatile.
We use advanced methods to make sure the cells are top-notch. This is key for growing them further.
Lab work to grow human embryonic stem cells is tough. It’s hard to keep the cells versatile and avoid contamination. Optimized culture media and constant checks are vital to beat these hurdles.
We follow strict rules to handle the cells right. This is critical for both research and therapy.
Creating and keeping human embryonic stem cell lines is vital for research and therapy. It’s not just about getting the cells first. It’s also about growing them over time and checking their quality.
We have the latest facilities and follow strict quality rules. This makes sure our cell lines are dependable and consistent. It helps move regenerative medicine and cell therapy forward.
Human embryonic cells are key in developmental biology research. They help us understand the early stages of human development. Their ability to become different cell types is very useful for studying developmental processes.
We use human embryonic cells to model human embryogenesis. This lets us study the complex early development processes. It helps us see how different cell types form and how development is controlled.
Key aspects of this research include:
Genetic expression studies with human embryonic cells give us insights into gene regulation during development. By looking at gene expression, we find important genes for developmental processes.
Recent studies have shown that cholesterol metabolism plays a significant role in stem cell fate, impacting various stem cell types, including embryonic stem cells.
Comparing human embryonic cells with other stem cells, like induced pluripotent stem cells (iPSCs), helps us see their strengths and weaknesses. This comparison is important for choosing the right cell type for research.
For more information on stem cell applications, visit our page on stem cell treatments.
Human embryonic cells have opened new doors in understanding and treating diseases. They are used in over 115 global clinical trials for conditions like neurological disorders and diabetes. This progress is thanks to creating disease-specific cell lines for studying genetic disorders at the cellular level.
Disease-specific cell lines from human embryonic cells help researchers model diseases in a lab dish. This method is key in studying complex conditions like heart disease, neurological disorders, and diabetes. Scientists can test treatments in a controlled setting by creating cell lines that mimic these diseases.
Key benefits of disease-specific cell lines include:
Human embryonic cells let researchers study genetic disorders at the cellular level. This gives insights into the causes of these conditions. By looking at how genetic mutations affect cells, scientists can find new treatments.
For instance, researchers have used human embryonic cells to model neurodegenerative diseases such as Parkinson’s and Alzheimer’s. These models help understand disease progression and find new treatments.
Disease modeling with human embryonic cells has many benefits over traditional methods. It allows studying human cells directly, unlike animal models or immortalized cell lines. Also, these models better represent human disease pathology.
The advantages of using human embryonic cells in disease modeling include:
By using these benefits, researchers can find new treatments faster and understand diseases better.
Human embryonic cells are leading the way in regenerative medicine. They have unique properties that help in treating diseases. These cells can repair damaged tissues and organs.
Human embryonic cells are key in cell replacement strategies. They can become specific cell types to replace damaged ones. For example, embryonic stem cells can become insulin-producing beta cells, which could cure diabetes.
Here’s a table showing some cell types from human embryonic cells for therapy:
| Cell Type | Potential Therapeutic Application |
|---|---|
| Neurons | Treatment of neurodegenerative diseases like Parkinson’s |
| Cardiomyocytes | Repair of damaged heart tissue |
| Pancreatic beta cells | Treatment of type 1 diabetes |
Tissue engineering is another area where human embryonic cells are making a big difference. By mixing these cells with biomaterials, we can create tissue substitutes. A leading researcher says,
“The integration of embryonic stem cells with tissue engineering principles holds great promise for creating functional organs and tissues for transplantation.”
Organ regeneration with human embryonic cells is promising but faces challenges. We’ve made progress in turning these cells into different types. But making fully functional organs is complex.
We need to solve issues like ensuring proper blood flow and organ structure. Despite these challenges, regenerative medicine is advancing. We’re getting closer to effective treatments for many diseases. Our aim is to use these cells to improve patient lives.
Recent breakthroughs in human embryonic stem cell research have led to over 115 global clinical trials. These trials show the cells’ promise in treating many medical conditions. They are a big step forward in regenerative medicine, bringing hope to patients with severe diseases.
“The progress in human embryonic stem cell research is remarkable, and its translation into clinical applications is a testament to the dedication of the scientific community,” says a leading researcher in the field.
The global landscape of clinical trials using human embryonic stem cells is diverse and rapidly evolving. Countries around the world are investing heavily in stem cell research. These trials are investigating a wide range of therapeutic applications, from neurological disorders to diabetes and cardiac conditions.
One of the most promising areas of research is in the treatment of neurological disorders. Human embryonic stem cells are being used to develop therapies for conditions such as Parkinson’s disease, spinal cord injuries, and multiple sclerosis. The ability of these cells to differentiate into neural cells makes them valuable for such applications.
For instance, a current clinical trial is investigating the use of human embryonic stem cell-derived neural cells to treat patients with severe spinal cord injuries. Preliminary results have shown significant improvement in some patients, giving new hope for those with previously untreatable conditions.
Another significant area of research is in the treatment of diabetes using human embryonic stem cells. Scientists are working on developing pancreatic islet cells from embryonic stem cells. This approach could revolutionize the treatment of diabetes, providing a cure instead of just managing symptoms.
“The vastness of human embryonic stem cells’ ability to cure diabetes is immense. We are on the cusp of a major breakthrough in regenerative medicine,” said a diabetes researcher.
Human embryonic stem cells are also being explored for their use in treating ophthalmological and cardiac conditions. Researchers are developing therapies to repair damaged heart tissue and restore vision in patients with retinal diseases. The versatility of embryonic stem cells makes them suitable for a wide range of therapeutic applications.
In conclusion, the current clinical trials using human embryonic cells represent a significant advancement in regenerative medicine. As research continues to progress, we can expect to see new and innovative treatments emerging for a variety of debilitating diseases.
Human embryonic cells are changing the game in drug development. They help us create more accurate models of human diseases. This leads to better ways to find new drugs.
Human embryonic stem cells are a powerful tool for testing drug safety. We can turn these cells into many types of cells. This lets us see how drugs affect different tissues.
This method helps find out if a drug might be harmful early on. It saves a lot of time and money by avoiding late-stage failures.
The main advantages of using human embryonic cells for testing include:
We’re using human embryonic cells to make platforms for specific diseases. By turning these cells into types affected by certain diseases, we can study disease processes in a lab. This lets us:
This method is really helpful for complex diseases where animal models don’t work well.
Human embryonic cells are also leading the way in personalized medicine. We can make models of disease that are specific to each patient. This means we can tailor treatments to fit each person’s needs.
By using this method, we can make treatments much more effective. It’s a big step forward for precision medicine.
The rules around human embryonic cell research are complex. They reflect different views on ethics and science. Stringent regulation and ethical oversight are key for this field’s progress.
Research on human embryos is a sensitive topic. It involves many ethical questions. These include the moral status of embryos, the risk of misuse, and the need for consent.
Using human embryos in research raises big moral questions. Some think embryos should not be used for science. Others see the benefits as worth it under certain conditions.
Views on this research vary widely. They are shaped by culture, religion, and philosophy. For example, some countries allow research under strict rules, while others ban it.
The rules for embryonic cell research differ greatly around the world. Some countries have clear rules, while others are more vague or strict.
International groups help shape global rules. They work to make regulations consistent. This aims to help countries work together and keep ethics high.
In the U.S., rules for this research have been debated a lot. Funding for it has changed over time.
These changes affect more than just research. They impact healthcare too. Limits on funding can slow down the development of new treatments.
We need to keep improving our rules and ethics for this research. It’s important to do it right, with careful oversight and openness.
As we learn more about human embryonic cells, new doors open for regenerative medicine. Research and trials are showing us how these cells can help in many ways. They could treat neurological issues and help in creating new tissues.
These cells are very promising for better health care. We’re looking forward to big steps in treating diseases and finding new medicines. Their special qualities make them key for finding new treatments and understanding human health.
As we keep studying, human embryonic cells will be key in regenerative medicine’s future. With more research and trials, we can use these cells to make medicine better and help more people.
Human embryonic cells, or embryonic stem cells, come from embryos. They can turn into almost any cell in the body. This makes them key in stem cell research, helping in regenerative medicine and cell therapy.
Pluripotency means a cell can become any cell type in the body. Human embryonic cells have this ability. This makes them very useful for research and treatments, like regenerative medicine and cell therapy.
Human embryonic cells are taken from blastocysts with careful techniques. In the lab, they need specific conditions to keep growing and changing into different cells.
Creating and keeping human embryonic cell lines is hard. It needs precise lab work and avoiding cell changes or contamination. Overcoming these issues is key for reliable research and treatments.
Researchers use human embryonic cells to make disease-specific cell lines. This lets them study genetic disorders closely. It’s better than old research methods because it’s more like human disease.
Human embryonic cells could help in regenerative medicine. They might replace damaged tissues and organs. This could offer new ways to treat many health problems.
There are ongoing clinical trials with human embryonic cells. They’re looking at treating diseases like neurological disorders and diabetes. These trials check if these cells are safe and work well as treatments.
Human embryonic cells help in testing drug safety and in making disease-specific treatments. They’re used in drug development and personalized medicine. This uses their special qualities to find new treatments faster.
Research on human embryonic cells raises ethical questions because it involves embryos. Different countries have different rules for this research. It’s important for researchers and policymakers to know these rules.
The future of human embryonic cell research looks bright. Ongoing studies and trials are making progress. We can expect new discoveries in regenerative medicine, leading to better treatments and care for patients.
International Society for Stem Cell Research (ISSCR): Guidelines
University of Minnesota Policy Library: Embryonic Stem Cells Policy
STAT News: Human embryonic stem cells research funding ban, Project 2025, Trump, HESC (News Article)
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!