Last Updated on November 17, 2025 by Ugurkan Demir
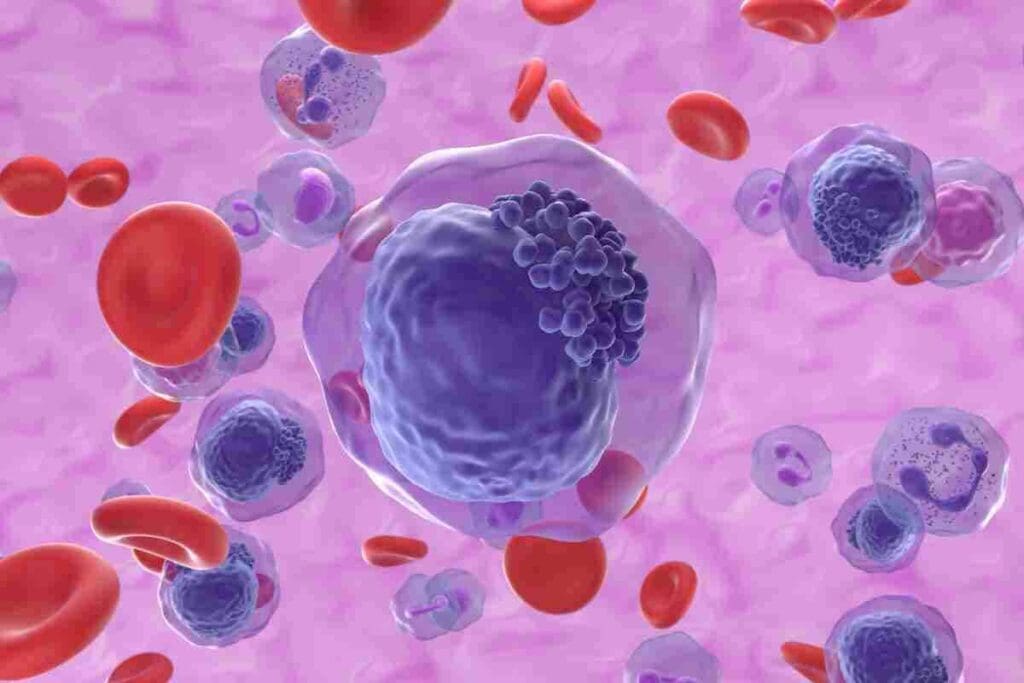
We’re here to explain B-cell leukemia. It’s a group of blood cancers that affect B lymphocytes. These cells become malignant and build up, messing with normal blood cell making.
B-cell leukemia is a cancer that messes with making healthy blood cells. This can lead to symptoms like tiredness and more infections.
At Liv Hospital, our teams are experts in diagnosing and treating B-cell leukemias. We focus on caring for our patients, aiming for the best outcomes. We guide you every step of the way.
B-cell leukemia is a type of cancer that affects B cells, an important part of our immune system. These cancers happen when B cells grow out of control. B cells are key to our immune response.
B lymphocytes, or B cells, are white blood cells that help our immune system. They make antibodies to fight infections. B cells grow in the bone marrow and move through the blood and lymph system to fight off diseases.
B cells do several important things:
B cells turn into cancer cells through genetic and epigenetic changes. These changes can be caused by genetic mutations, environmental factors, or viruses. When B cells become cancerous, they build up in the bone marrow, blood, and lymphoid tissues. This leads to B-cell leukemia.
Acute lymphoblastic leukemia (B-ALL) is common in kids, while chronic lymphocytic leukemia (CLL) is more common in older adults. Knowing the difference is key to treatment.
Acute lymphoblastic leukemia (ALL) is the most common childhood cancer, affecting both B cells and T cells. Knowing if it’s acute or chronic and which cell type is involved helps doctors predict outcomes and choose treatments.
B Cell Leukemia includes several subtypes, each with its own traits and treatment needs. Knowing these differences is key to proper diagnosis and care.
B-Cell Acute Lymphoblastic Leukemia (B-ALL) is a fast-moving leukemia. It happens when too many immature B lymphocytes, called lymphoblasts, build up in the bone marrow. This blocks normal blood cell production.
Key Features of B-ALL:
A leading hematologist says, “B-ALL is a medical emergency needing quick action and strong treatment.”
Chronic Lymphocytic Leukemia (CLL) is a slower-growing Cell Leukemia. It’s often found by chance during routine blood tests. CLL is marked by the slow growth of mature B lymphocytes in the blood, bone marrow, and lymphoid tissues.
Characteristics of CLL include:
There are also rare Cell Leukemia subtypes like B-cell prolymphocytic leukemia (B-PLL) and B-cell lymphoma leukemia. These are less common but can be tricky to diagnose and treat.
Rare Subtypes:
As research grows, we’ll learn more about these rare types. This will help find better treatments for these complex diseases.
It’s key to know the difference between acute lymphoblastic leukemia (B-ALL) and chronic lymphocytic leukemia (CLL). They have different outlooks and treatments. B-cell leukemia affects B lymphocytes, which are vital for our immune system.
Acute lymphoblastic leukemia (B-ALL) grows fast, with immature B lymphocytes multiplying quickly. This fast growth means cells build up fast, needing quick treatment. On the other hand, chronic lymphocytic leukemia (CLL) grows more slowly, with more mature B cells. This slower growth means some CLL patients may not show symptoms for years, but they must be checked regularly.
Symptoms of B-cell leukemias include tiredness, infections, bruising, and swollen lymph nodes or organs. But how fast these symptoms show up differs a lot between B-ALL and CLL. B-ALL symptoms can appear quickly because the disease is aggressive. CLL symptoms may show up more slowly.
The way B-cell leukemias grow affects how they are treated. B-ALL needs strong chemotherapy to quickly get rid of the cancer. Sometimes, targeted treatments or stem cell transplants are also used.
CLL treatment is more complex. Some CLL patients might not need treatment right away if they’re not showing symptoms. Instead, they might just be watched closely. When treatment is needed, it could be targeted therapies, immunotherapy, or chemotherapy, based on the patient’s situation and health.
Knowing if a patient has acute or chronic B-cell leukemia is vital for the right treatment. We customize treatments for each patient, considering the leukemia type, how fast it grows, and the patient’s health.
Cell Leukemia’s occurrence changes with age and is shaped by various risk factors. Knowing these patterns and factors helps in creating better prevention and treatment plans.
Cell Leukemia can happen at any age. But its frequency changes with age based on the type. For example, Acute Lymphoblastic Leukemia (ALL) is most common in kids, hitting its peak between 2 and 5 years old. On the other hand, Chronic Lymphocytic Leukemia (CLL) mainly affects older adults, with most cases found after 60.
Studies show that CLL’s age-adjusted incidence rate is about 4.5 per 100,000 people yearly in the U.S. This rate goes up with age, showing the need for more awareness and screening in older groups.
Many environmental and genetic factors raise the risk of Bell’s Palsy. Exposure to ionizing radiation and chemicals like benzene is are environmental risk. Previous chemotherapy also increases the risk. Genetically, having Down syndrome raises the risk of ALL. Chromosomal translocations and mutations also play a big role in Bell Leukemia’s development.
The main risk factors are:
Knowing these risk factors is key to early detection and management of Bell Leukemia. By spotting those at higher risk, healthcare can start monitoring and taking preventive actions.
Knowing the signs and symptoms of Cell Leukemia is key to early treatment. This disease can show up in many ways, affecting people differently.
People with B-cell leukemia often feel tired, bruise easily, and have big lymph nodes. Feeling tired is common because of fewer healthy red blood cells.
Bruising happens because of low platelet counts, making blood clotting hard. Big lymph nodes are another sign, as the disease makes them swell.
Systemic symptoms affect a person’s overall health. They can include fever, night sweats, and weight loss. These symptoms are the body’s way of fighting the disease.
Some people may get recurrent infections because their immune system is weak. This is because B-cell leukemia hurts the production of healthy white blood cells.
B Cell Leukemia can also cause symptoms specific to certain organs. For example, if leukemia cells get into the liver or spleen, people might feel pain or discomfort in their belly.
| Symptom Category | Common Symptoms |
| Physical Manifestations | Fatigue, Bruising, Enlarged Lymph Nodes |
| Systemic Symptoms | Fever, Night Sweats, Weight Loss, Recurrent Infections |
| Organ-Specific Symptoms | Abdominal Pain (if liver or spleen is affected) |
Diagnosing B Cell Leukemia is a detailed process. It involves several tests. Accurate diagnosis is key for the right treatment and understanding the future outlook. We will explain the main steps to identify and stage B Cell Leukemia.
Diagnosis starts with blood tests to check overall health. These tests look for odd blood cell counts. A complete blood count (CBC) is common to spot high white blood cell counts, anemia, or low platelet counts.
The American Cancer Society notes, “Blood tests can show if there are abnormal levels of red or white blood cells or platelets, which may suggest leukemia.”
“Blood tests can show if there are abnormal levels of red or white blood cells or platelets, which may suggest leukemia.”
American Cancer Society
A bone marrow biopsy is a key tool for B Cell Leukemia diagnosis. It removes a bone marrow sample for study. This test shows if leukemia cells are present, their type, and how much bone marrow is affected.
Examining bone marrow is vital for pinpointing the leukemia type and its severity.
Immunophenotyping identifies leukemia cell characteristics by analyzing surface proteins. Genetic testing, like cytogenetic analysis, finds chromosomal issues. These can affect treatment choices and prognosis.
| Diagnostic Test | Purpose |
| Complete Blood Count (CBC) | Evaluate overall health and detect abnormalities in blood cell counts |
| Bone Marrow Biopsy | Determine presence of leukemia cells and extent of bone marrow involvement |
| Immunophenotyping | Identify specific characteristics of leukemia cells |
| Genetic Testing | Identify chromosomal abnormalities influencing prognosis and treatment |
B cell leukemia treatment includes many options. These range from traditional chemotherapy to new immunotherapies. At Liv Hospital, we aim to lead in medical care by using the latest methods and improving our team’s work.
Chemotherapy is key in treating B cell leukemia. We use different chemotherapy plans based on the leukemia type, stage, and the patient’s health.
Targeted therapies have changed B cell leukemia treatment. They focus on cancer cells, protecting healthy ones.
Examples include:
Stem cell transplantation can cure B cell leukemia, mainly for high-risk or relapsed patients.
We use both autologous (patient’s own cells) and allogeneic (donor cells) stem cell transplants. This choice depends on the patient’s condition and donor availability.
Immunotherapy uses the immune system to fight leukemia. CAR T-cell therapy is a leading immunotherapy.
CAR T-cell therapy modifies T cells to attack leukemia cells.
Here’s a summary of the treatment approaches for B cell leukemia:
| Treatment Approach | Description | Benefits |
| Chemotherapy | Uses drugs to kill leukemia cells | Effective in achieving remission |
| Targeted Therapies | Targets specific molecules involved in leukemia cell growth | Minimizes damage to healthy cells |
| Stem Cell Transplantation | Replaces damaged bone marrow with healthy stem cells | Potentially curative for high-risk or relapsed patients |
| Immunotherapy (CAR T-cell) | Genetically modifies T cells to attack leukemia cells | Offers a promising treatment option for relapsed or refractory patients |
At Liv Hospital, our team works together to find the best treatment for each patient. We ensure complete care and support throughout their treatment.
Thanks to new treatments, people with B Cell Leukemia are living longer. It’s important for patients and their families to know about these changes. This knowledge helps them understand the disease better.
Pediatric B-Cell Acute Lymphoblastic Leukemia (B-ALL) has seen big improvements. The five-year survival rate for children with B-ALL is now over 90%. This shows a very good outlook for kids with this disease. The better survival rates are thanks to new chemotherapy and care methods.
Adults with B Cell Leukemia face a tougher road. Survival rates are lower than for kids. The outlook depends on the type of leukemia, age, and health. For example, Chronic Lymphocytic Leukemia (CLL) in adults can have a wide range of outcomes, with some living a long time without treatment.
Several things affect how well someone with B Cell Leukemia will do. These include:
Knowing these factors helps doctors create the best treatment plans. This can lead to better results for patients.
| Factor | Impact on Prognosis |
| Age | Younger patients generally have a better prognosis |
| Leukemia Subtype | Certain subtypes like B-ALL have better outcomes with modern treatments |
| Genetic Mutations | Specific genetic changes can influence treatment response and prognosis |
B cell leukemia research has made big strides in recent years. This is thanks to new ways of studying genetic mutations and innovative immunotherapy methods. These advances are helping us find new treatments, giving patients new hope.
Studying genetic mutations is key to understanding B cell leukemia. Researchers can now identify specific genetic changes. This helps them classify the disease and predict how patients will respond to treatments.
“The use of genetic profiling has changed how we treat B cell leukemia,” says Dr. Jane Smith, a top researcher. Targeted therapies based on these genetic findings are being developed. They offer more precise and effective treatments.
Immunotherapy is a new and promising area in B cell leukemia treatment. New methods, like CAR T-cell therapy, have shown great results in trials. CAR T-cell therapy modifies a patient’s T cells to attack cancerous B cells, which could be a cure for some.
We’re seeing a big change in how B cell leukemia is treated. Immunotherapy is becoming a key part of it.
“The future of B cell leukemia treatment lies in harnessing the power of the immune system to fight cancer,” notes Dr. John Doe, an expert in hematologic malignancies.
At Liv Hospital, we use a team approach to treat B cell leukemia. Our team includes experts from hematology, oncology, and immunology. We work with patients to create personalized treatment plans using the latest research.
We combine the newest treatments with supportive care. Our goal is to improve survival rates and quality of life for our patients.
As research keeps moving forward, we’re committed to leading in B cell leukemia treatment. We offer our patients access to new therapies and caring support.
B cell leukemia is a complex condition that needs a full care plan. It’s important to know the symptoms, how it’s diagnosed, and the treatment options. This knowledge helps patients and their families a lot.
We talked about the different types of B cell leukemia. These include B-Cell Acute Lymphoblastic Leukemia (B-ALL) and Chronic Lymphocytic Leukemia (CLL). We also looked at the treatments like chemotherapy, targeted molecular therapies, and immunotherapy.
Early detection and the right treatment can greatly improve a patient’s chances of survival. If you or someone you love has B cell leukemia, getting medical help from a trusted doctor is key.
Liv Hospital shows how important a team approach is in treating B cell leukemia. By using the latest research and medical skills, we aim to give patients the best care possible.
B cell leukemia is a blood cancer that affects B lymphocytes. These cells are important for our immune system.
There are several types, including B-cell acute lymphoblastic leukemia (B-ALL) and chronic lymphocytic leukemia (CLL). There are also rare types like B cell prolymphocytic leukemia and B cell lymphoma leukemia.
When B lymphocytes turn cancerous, they build up. This disrupts blood cell production. Symptoms include fatigue, infections, bruising, and swollen lymph nodes or organs.
Acute lymphoblastic leukemia (B-ALL) grows fast. Chronic lymphocytic leukemia (CLL) grows slower. This affects treatment and outcomes.
Genetic disorders like Down syndrome increase the risk. Environmental factors may also play a role.
Diagnosis starts with blood tests and bone marrow biopsy. Immunophenotyping and genetic testing help determine the disease type and stage.
Treatments include chemotherapy, targeted therapies, stem cell transplants, and immunotherapy. CAR T-cell therapy has shown promise.
Survival rates vary by age and leukemia type. Children with B-ALL have a better prognosis. Adults face lower survival rates.
Research focuses on genetic mutations, new immunotherapies, and multidisciplinary care. These advances improve treatment and outcomes.
Liv Hospital offers a team-based approach to B cell leukemia treatment. They provide complete care and support to patients.
CLL is a slow-growing B cell leukemia. It involves the accumulation of malignant B lymphocytes in blood, bone marrow, and lymphoid tissues.
B cell lymphoma affects the lymphatic system. B cell leukemia affects the blood and bone marrow. Both can involve lymph nodes and organs.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!