Sudden pain in your abdomen or digestive issues might mean a serious problem. This could be a blood clot in the abdomen. At LivHospital, we focus on you and use the latest medical care. Knowing about abdominal clots risks, causes, and quick treatments is key to keeping you safe. Learn causes, symptoms, and treatment options for a blood clot in the abdomen.
Abdominal blood clots, linked to mesenteric venous thrombosis, can cause severe pain, swelling, nausea, and vomiting. If not treated, these clots can be deadly. Quick medical help is vital to avoid serious issues.
We’ll help you understand the causes, signs, diagnosis, and treatment for blood clots in the stomach. You’ll get all the care and support you need.
Key Takeaways
- Abdominal blood clots can cause severe symptoms and are life-threatening if untreated.
- Prompt diagnosis using imaging techniques like CT scans is critical.
- Treatment options include anticoagulants, thrombolytics, or surgery.
- Understanding the risks and causes of abdominal clots is essential for your health.
- LivHospital offers patient-centered care and the latest medical protocols.
Understanding Abdominal Blood Clots
It’s key to know about abdominal blood clots to spot warning signs early. These clots form in the blood vessels of the belly area. They can block blood flow to important organs.
What Is a Blood Clot in the Abdomen?
A blood clot in the belly happens when a clot forms in veins or arteries. These supply blood to the digestive organs. This is called mesenteric venous thrombosis when it affects the veins draining the intestines.
Mesenteric venous thrombosis (MVT) is a serious type of abdominal blood clot. It causes severe belly pain and is a medical emergency. It forms in veins draining the intestines, which can lead to serious problems if not treated quickly.
Prevalence and Statistics
Abdominal blood clots are rare but serious. Mesenteric venous thrombosis is a small part of acute abdomen cases. Its rate varies worldwide.
| Condition | Prevalence Rate | Common Symptoms |
| Mesenteric Venous Thrombosis | 0.01-0.1% | Severe abdominal pain, nausea, vomiting |
| Portal Vein Thrombosis | 1-2% in patients with liver disease | Abdominal pain, ascites, variceal bleeding |
Why They’re Considered Medical Emergencies
Abdominal blood clots are emergencies because they can cause serious problems. These include bowel ischemia, organ failure, and death. Quick action is needed to avoid these risks.
Quick medical help can greatly improve a patient’s chances. This shows how important it is to act fast when symptoms appear.
Anatomy of Abdominal Circulation
Knowing how blood flows through the abdomen is key to treating blood clots there. The abdominal area has a complex network of blood vessels. These vessels carry oxygen and nutrients to the digestive organs.
Major Blood Vessels in the Abdomen
The abdomen has major blood vessels that are vital for its health. The aorta is the main artery from the heart to the abdomen. It splits into smaller arteries.
The celiac artery, superior mesenteric artery, and inferior mesenteric artery are important. They supply blood to the digestive organs.
The venous system in the abdomen is also critical. The portal vein carries blood from the digestive organs to the liver. This is for detoxification and nutrient processing.
How Blood Circulates Through Digestive Organs
Blood flow through the digestive organs is carefully managed. Arteries bring oxygen-rich blood to the stomach, small intestine, and liver. Veins take away oxygen-poor blood.
The superior mesenteric vein and splenic vein join to form the portal vein. This vein is key for nutrient absorption and processing.
Vulnerable Areas for Clot Formation
Some areas in the abdominal circulation are more likely to form clots. This is due to blood flow and vessel shape. The mesenteric veins are at high risk for thrombosis.
Mesenteric venous thrombosis is a serious condition. It needs quick medical attention.
| Vessel | Function | Vulnerability to Clot Formation |
| Portal Vein | Carries blood from digestive organs to the liver | High |
| Superior Mesenteric Vein | Drains blood from the small intestine | High |
| Celiac Artery | Supplies blood to the stomach, liver, and spleen | Moderate |
Knowing which areas are at risk is vital for treating abdominal blood clots. Early detection and treatment can prevent serious problems.
Common Causes of Blood Clot in the Abdomen
Blood clots in the abdomen often stem from several main factors. We’ll dive into these, shedding light on what causes and increases the risk of these clots.
Vessel Injury and Inflammation
Vessel injury and inflammation play big roles in abdominal blood clots. Conditions like inflammatory bowel disease (IBD) can damage blood vessels. This damage raises the risk of clotting.
“Inflammatory bowel disease is a known risk factor for venous thromboembolism, including abdominal blood clots.”
Sluggish Blood Flow Conditions
Sluggish blood flow, caused by things like bed rest, surgery, or cancer, also raises clot risk. Slow blood flow makes it easier for clots to form.
- Prolonged immobilization
- Post-surgical recovery
- Cancer and its treatment
Hypercoagulability Disorders
Hypercoagulability disorders mess with blood clotting, upping clot risk. These can be inherited or caused by cancer, hormonal changes, or meds.
| Condition | Description | Risk Level |
| Factor V Leiden | Inherited disorder affecting clotting | High |
| Antiphospholipid syndrome | Autoimmune disorder causing clotting | High |
| Cancer | Increases clotting risk through various mechanisms | Variable |
Risk Factors and Predisposing Conditions
Many risk factors and conditions can up the chance of getting an abdominal blood clot. These include trauma, infection, and blood clotting disorders. Knowing these can help prevent and treat clots.
Understanding the causes and risk factors of abdominal blood clots helps doctors prevent and treat them. This improves patient care.
Recognizing the Warning Signs and Symptoms
Spotting abdominal blood clots early can greatly improve treatment results. These clots can show up in different ways. Knowing the early signs is key for quick medical help.
Early Warning Signs
The first signs of abdominal blood clots are often subtle but important. You might feel mild pain in your belly, nausea, or notice slight changes in your bowel movements. Being alert to these signs is vital, even more so if you’re at risk for blood clots.
- Mild abdominal pain or discomfort
- Nausea or vomiting
- Changes in bowel movements or diarrhea
- Mild fever
Severe Symptoms Requiring Immediate Attention
While it’s important to catch early signs, severe symptoms need immediate care. These include intense belly pain, signs of shock, or organ failure.
| Symptom | Description |
| Severe Abdominal Pain | Pain that is intense and unrelenting, often requiring immediate medical evaluation. |
| Signs of Shock | Low blood pressure, rapid heartbeat, and decreased urine output, indicating inadequate blood circulation. |
| Organ Failure | Failure of vital organs such as the kidneys or liver, which can be a complication of untreated abdominal blood clots. |
How Symptoms Differ from Other Abdominal Conditions
Symptoms of abdominal blood clots can look like other belly issues, making it hard to diagnose. But, knowing your risk for blood clots and how severe your symptoms are can help tell them apart.
When to Seek Emergency Care
If you have severe symptoms like intense belly pain, signs of shock, or a history of blood clots, get emergency care right away. Quick medical action can make a big difference.
Emergency Care Checklist:
- Severe abdominal pain
- Signs of shock (low blood pressure, rapid heartbeat)
- History of blood clots or predisposing conditions
We stress the importance of knowing the signs and symptoms of abdominal blood clots. Spotting them early and getting medical help fast is key to effective treatment and avoiding serious problems.
Types of Blood Clots in the Abdomen
It’s important to know about the different types of blood clots in the abdomen. This knowledge helps doctors diagnose and treat them better. Blood clots in the abdomen can vary, each with its own health risks and treatment plans.
We will look at the various types of blood clots in the abdominal area. We’ll discuss their unique features and what they mean for a patient’s health.
Mesenteric Venous Thrombosis
Mesenteric venous thrombosis is when a blood clot forms in the veins draining the intestines. This can cause the intestines to not get enough blood, leading to serious problems if not treated quickly.
Key characteristics of mesenteric venous thrombosis include:
- Often linked to conditions that make blood clot more easily
- May cause stomach pain, nausea, and vomiting
- Doctors use CT scans to diagnose it
Portal Vein Thrombosis
Portal vein thrombosis is when a blood clot forms in the portal vein. This vein carries blood from the intestines to the liver. It can cause high blood pressure in the portal vein and serious issues.
The clinical presentation may include:
- Stomach pain and swelling
- Bleeding in the digestive system
- Fluid buildup in the belly
Splenic and Hepatic Vein Thrombosis
Splenic and hepatic vein thrombosis are when blood clots form in veins draining the spleen and liver. These can cause problems with how these organs work and lead to other serious issues.
Characteristics and implications include:
- Splenic vein thrombosis can cause the spleen to get bigger and not work right
- Hepatic vein thrombosis (Budd-Chiari syndrome) can cause liver failure
- Both need quick diagnosis and treatment
Can You Get Blood Clots in Your Stomach?
Blood clots can happen in veins around the stomach, but it’s not common. The stomach itself usually doesn’t get blood clots. But, the veins around it can.
| Type of Blood Clot | Location | Key Characteristics |
| Mesenteric Venous Thrombosis | Veins draining intestines | Abdominal pain, nausea, vomiting; associated with hypercoagulability |
| Portal Vein Thrombosis | Portal vein | Abdominal pain, gastrointestinal bleeding, ascites |
| Splenic Vein Thrombosis | Veins draining spleen | Splenomegaly, hypersplenism |
| Hepatic Vein Thrombosis | Veins draining liver | Liver failure, Budd-Chiari syndrome |
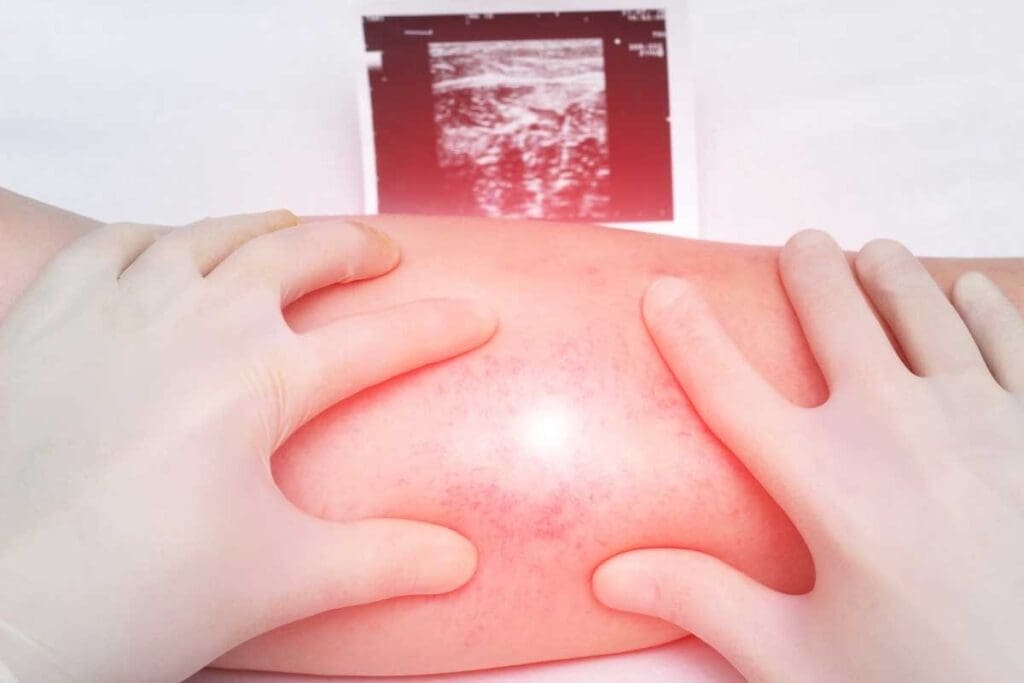
Diagnostic Approaches for Abdominal Blood Clots
Diagnosing abdominal blood clots requires a detailed process. This includes clinical checks, lab tests, and imaging. We use these methods together to find and treat blood clots in the abdomen.
Physical Examination and Medical History
First, we do a full physical check and ask about the patient’s health history. We look for signs like pain, nausea, and fever. These could mean there’s a blood clot.
We also check for tenderness, guarding, and swelling in the belly. These signs mean we need to do more tests.
Blood Tests and Biomarkers
Blood tests are key in finding abdominal blood clots. We check biomarkers to see if there’s clotting. Tests like D-dimer levels show if there’s a clot.
We also test for conditions that might cause clots, like thrombophilia or cancer. These tests help us figure out why the clot happened and how to treat it.
Advanced Imaging Techniques
Imaging is vital to confirm blood clots. We often use CT scans with contrast to see the clot. CT scans show where and how big the clot is.
We might also use ultrasound and MRI in some cases. Ultrasound checks blood flow, and MRI gives detailed belly pictures. This helps us find the right diagnosis.
Choosing the right imaging depends on the patient’s situation and what we think is wrong. We pick the best method to make sure we diagnose and treat correctly.
Treatment Options and Modern Protocols
There are many ways to treat abdominal blood clots. These include medicines and surgery. The right treatment depends on the clot’s size and location, the patient’s health, and any other health issues.
Anticoagulant Medications
Medicines to prevent clotting are key for many patients. These drugs stop new clots from forming and prevent existing ones from getting bigger. Heparin and warfarin are common, but newer drugs like rivaroxaban and apixaban are also used. They are easier to take and don’t need as much monitoring.
Thrombolytic Therapy
Thrombolytic therapy is used in some cases to break down the clot. It’s for patients with severe symptoms or at high risk of complications. The drugs are given directly to the clot through a catheter to work best without affecting the whole body.
Surgical and Interventional Procedures
Some patients need surgery or interventional procedures. These include removing the clot surgically or using angioplasty and stenting to improve blood flow. Techniques like transcatheter embolization are also used to manage specific risks or complications.
Supportive Care Measures
Supportive care is also vital for patients with abdominal blood clots. It includes managing pain, staying hydrated, and watching for complications. It also involves nutrition and managing any underlying health issues.
By using a mix of treatments, doctors can create care plans that meet each patient’s needs. This approach helps improve outcomes and lowers the risk of complications from abdominal blood clots.
Potential Complications and Prognosis
It’s key to know the risks of abdominal blood clots for better care and results. These clots can be very serious and even life-threatening if not treated quickly.
Short-term Complications
Abdominal blood clots can cause a lot of harm in the short term. One big risk is bowel ischemia. This happens when a clot blocks blood to the intestines. It can damage tissue, cause the bowel to die, and even lead to a life-threatening hole in the bowel.
Common short-term complications include:
- Bowel ischemia and necrosis
- Organ failure due to inadequate blood supply
- Severe abdominal pain and distension
- Nausea and vomiting
Long-term Health Consequences
People who survive abdominal blood clots may face lasting health issues. These can include ongoing pain, trouble absorbing nutrients, and a higher chance of getting more blood clots.
| Long-term Consequence | Description |
| Chronic Abdominal Pain | Ongoing pain due to bowel or organ damage |
| Malabsorption | Impaired nutrient absorption due to bowel damage |
| Increased Thrombotic Risk | Higher risk of developing future blood clots |
Mortality Rates and Survival Factors
The death rate from abdominal blood clots depends on several factors. These include where the clot is, how big it is, and how fast treatment starts. Quick diagnosis and treatment with blood thinners can greatly improve chances of survival. The patient’s health, any underlying conditions, and how well the treatment works also play a role.
Prompt medical intervention is critical in managing abdominal blood clots and improving survival chances.
Quality of Life After Treatment
How well someone does after treatment for abdominal blood clots can vary a lot. Some might fully recover, while others may have lasting symptoms or problems. It’s important to have follow-up care and rehabilitation to help improve their quality of life.
We stress the need for full care, including lifestyle changes and managing any underlying conditions. This can help improve long-term outcomes for those with abdominal blood clots.
Prevention and Risk Management
To prevent abdominal blood clots, it’s important to know the risks and take steps to lower them. By being proactive, people can greatly reduce their chance of getting these dangerous clots.
Lifestyle Modifications
Changing your lifestyle is a key way to stop abdominal blood clots. Here are some tips:
- Regular Exercise: Moving your body helps blood flow better, which lowers clot risk.
- Maintaining a Healthy Weight: Being overweight puts more pressure on veins, making clots more likely.
- A Balanced Diet: Eating lots of fruits, veggies, and whole grains helps manage weight and keeps blood vessels healthy.
- Staying Hydrated: Drinking enough water is key for blood flow and preventing dehydration, which can cause clots.
- Avoiding Prolonged Immobility: Moving around, even when sitting for long or in bed, stops blood from pooling and clotting.
Medical Prophylaxis for High-Risk Individuals
For those at high risk, medical steps are very important. This might include:
- Anticoagulant Medications: These drugs stop blood from clotting and are given to those at high risk.
- Compression Stockings: These help blood flow in the legs, lowering clot risk.
- Intermittent Pneumatic Compression Devices: These devices help improve leg circulation by inflating and deflating.
Monitoring and Regular Check-ups
Regular visits to the doctor are key for those at risk. They help catch problems early and treat them quickly.
Managing Underlying Conditions
It’s also important to manage health issues that can lead to blood clots. This includes:
- Controlling Hypertension: High blood pressure can damage blood vessels, making clots more likely.
- Managing Diabetes: High blood sugar can damage blood vessels and nerves, raising clot risk.
- Treating Heart Conditions: Heart problems like atrial fibrillation can increase clot risk.
By using these strategies, people can lower their risk of getting abdominal blood clots. Working with doctors to create a prevention plan is essential.
Conclusion
It’s important to know about abdominal blood clots to get help fast. We talked about what causes them, like injuries and certain health issues. We also looked at the symptoms, which can be mild or serious.
A summary of abdominal blood clots shows they can cause big problems if not treated right away. Doctors use tests and scans to find these clots. Treatment can be medicine or surgery, based on the clot’s size and where it is.
Preventing blood clots is very important, too. Making healthy choices and getting medical care can help a lot. Knowing about causes, symptoms, and treatment helps people get help quickly.
We stress the need to know about abdominal blood clots and act fast. By understanding the risks and taking steps to prevent them, people can stay healthier.
FAQ
What is a blood clot in the abdomen?
A blood clot in the abdomen forms in the blood vessels that supply the digestive organs. This can happen in the mesenteric veins or the portal vein. It can cause severe pain and is a serious condition.
Can you get blood clots in your stomach?
While we don’t say “blood clot in the stomach,” clots can form in the stomach’s blood vessels. This leads to conditions like mesenteric venous thrombosis or portal vein thrombosis.
What are the symptoms of a blood clot in the abdomen?
Symptoms include severe abdominal pain, nausea, vomiting, and bloody stools. The symptoms’ severity and nature depend on the clot’s location and size.
How is a blood clot in the abdomen diagnosed?
Diagnosis involves a physical exam, medical history, blood tests, and imaging like CT scans or ultrasound.
What are the treatment options for abdominal blood clots?
Treatment includes anticoagulant medications and thrombolytic therapy. Surgery or interventional procedures may also be needed. Supportive care helps manage symptoms and prevent complications.
Can abdominal blood clots be prevented?
Yes, prevention involves lifestyle changes and medical prophylaxis. Regular check-ups and managing underlying conditions are also key.
What are the possible complications of abdominal blood clots?
Complications include bowel ischemia or infarction. Long-term issues like chronic pain or digestive problems can also occur. Mortality rates depend on treatment severity and promptness.
Are blood clots in the abdomen a serious condition?
Yes, they are a medical emergency. They can cause severe and life-threatening complications if not treated quickly.
How do blood clots in the abdomen affect quality of life?
The impact on quality of life varies. It depends on the condition’s severity, treatment success, and any long-term complications or underlying conditions.
What is mesenteric venous thrombosis?
Mesenteric venous thrombosis is a blood clot in the veins draining the intestines. It causes severe pain, bowel ischemia, and can be life-threatening.
What are the risk factors for developing abdominal blood clots?
Risk factors include conditions causing vessel injury or inflammation. Sluggish blood flow, hypercoagulability disorders, and conditions like cancer or inflammatory bowel disease are also risk factors.
Reference
- National Center for Biotechnology Information (NCBI): Mesenteric Venous Thrombosis – StatPearls — In-depth review on causes, diagnosis, and treatment of mesenteric venous thrombosis., https://www.ncbi.nlm.nih.gov/books/NBK459184