Osteoarthritis affects over 32.5 million adults in the United States. It causes a lot of pain and makes it hard to move, mainly in the knees. This condition can severely impact one’s ability to walk, a key part of daily life.
“As osteoarthritis gets worse, it can cause chronic pain and stiffness. This makes simple tasks hard to do and can lead to knee problems walking. Many worry about losing their ability to move because of this condition.
Key Takeaways
- Osteoarthritis is a leading cause of disability among adults.
- It significantly affects the knees, impacting walking ability.
- Advanced osteoarthritis can lead to chronic pain and mobility issues.
- Various treatments are available to manage arthritis in the knees.
- Early intervention can help mitigate the progression of osteoarthritis.
The Relationship Between Osteoarthritis and Mobility
Osteoarthritis and reduced mobility are closely linked. This degenerative joint disease can make it hard to move freely. We will look into how osteoarthritis impacts joints and mobility.
What Happens to Joints in Osteoarthritis
In osteoarthritis, the cartilage that protects joints wears down. This leads to bone rubbing against bone, causing pain and stiffness. Joint damage is a key feature of osteoarthritis, affecting daily life greatly.
How Joint Damage Affects Movement
Joint damage from osteoarthritis can reduce mobility. The pain and stiffness make simple tasks, like walking, hard. People with osteoarthritis often change how they walk to avoid pain.
Statistics on Mobility Loss in Osteoarthritis Patients
Research shows osteoarthritis can cause big mobility problems. A large number of people with osteoarthritis face mobility loss.
| Study | Percentage of Mobility Loss |
| Study A | 30% |
| Study B | 45% |
| Study C | 25% |
These numbers show how much osteoarthritis affects mobility. Knowing this helps us find better ways to manage it.
How Knee Osteoarthritis Specificially Impacts Walking
Knee osteoarthritis can make walking hard, affecting life quality. It not only hurts the joint but also limits how well you can move.
Normal Knee Mechanics During Walking
Walking normally involves the knee moving in several ways. It flexes to absorb shock and extends to push you forward. This helps you move smoothly.
Key components of normal knee mechanics include:
- Smooth cartilage allowing for frictionless movement
- Strong ligaments providing stability
- Coordinated muscle contractions for controlled motion
Walking with Bone-on-Bone Knees
When osteoarthritis gets worse, cartilage can disappear. This leaves bones rubbing together, causing pain and stiffness. Walking becomes hard, and people may change how they walk to avoid pain.
The challenges of walking with bone-on-bone knees include:
- Increased pain during weight-bearing activities
- Reduced range of motion due to stiffness
- Altered gait patterns to avoid pain, potentially leading to further complications
Progressive Stages of Walking Difficulty
Knee osteoarthritis gets worse in stages, each affecting walking differently. At first, you might feel pain after walking or climbing stairs. As it gets worse, pain lasts longer, and you can’t walk as far.
The stages progress like this:
- Early Stage: Mild pain and stiffness, manageable with minimal lifestyle adjustments
- Moderate Stage: Noticeable pain during activities, requiring occasional use of assistive devices
- Advanced Stage: Severe pain and significant difficulty walking, often necessitating substantial lifestyle changes or surgical intervention
Knowing these stages helps manage expectations and find the right treatments to keep you moving.
Common Knee Problems Walking with Osteoarthritis

Knee problems from osteoarthritis can make walking hard. Osteoarthritis damages the cartilage, bones, and tissues in the knee. This leads to several issues.
Pain Patterns During Different Walking Activities
People with osteoarthritis often feel pain when walking. The pain can change based on the activity. For example, walking uphill can hurt the knee more because it puts more stress on the joint.
Walking on flat surfaces might be less painful but is hard because of ongoing inflammation and damage.
Pain during walking can be different, like sharp or aching. Sharp pain might mean a specific issue, like bone-on-bone contact. Aching pain is often from long-term inflammation and wear.
Morning Stiffness and Start-Up Pain
Morning stiffness and start-up pain are common in osteoarthritis. The knee can feel stiff after rest, making it hard to move. This stiffness usually gets better as you start walking and the joint gets more lubricated.
Start-up pain is when the knee hurts at the beginning of walking after rest. This pain usually goes away as you keep walking. It’s important to manage this pain to stay mobile and comfortable.
Instability and “Giving Way” Sensations
Instability in the knee is a big problem for those with osteoarthritis. The knee might feel like it’s going to collapse, which is scary and can lead to falls. This happens because the muscles and ligaments around the knee get weaker and the joint structure deteriorates.
Exercising the muscles around the knee can help with stability. Using canes or knee braces can also offer support and confidence while walking.
Changes in Gait Due to Knee Arthritis
Knee arthritis can change how we walk, making it harder to move around. This condition, also known as osteoarthritis of the knee, makes walking different. It’s because of pain, stiffness, or changes in the knee joint.
Why Do I Waddle When I Walk?
Waddling is common in people with advanced knee arthritis. It happens because the body tries to avoid pain and instability in the knee. Cassandra Smith, who has arthritis, says her walking changed a lot as her condition got worse.
Altered Gait Patterns and Their Causes
People with knee arthritis walk differently. They might walk slower, take shorter steps, and step unevenly. These changes come from avoiding pain, muscle weakness, and stiff joints.
- Pain makes people change how they walk to avoid hurting their knee more.
- Weak muscles around the knee make walking less stable.
- Stiff joints limit how far you can move, affecting your walk.
How Gait Changes Affect Other Joints
Changes in walking because of knee arthritis can affect other joints too. Walking differently puts more stress on joints like the hips, ankles, and lower back. This can cause problems or make existing issues worse.
| Joint | Potential Issues Due to Gait Changes |
| Hip | Increased stress and possible osteoarthritis |
| Ankle | Changes in how it works, leading to pain or injury |
| Lower Back | Strain or pain from trying to compensate |
Risk Factors for Losing Walking Ability
It’s important to know the risk factors for osteoarthritis to avoid losing walking ability. Several factors can lead to mobility problems in people with osteoarthritis.
Age and Disease Duration
Age is a big risk factor for losing walking ability due to osteoarthritis. As people get older, osteoarthritis gets worse, leading to more mobility issues. The longer you have the disease, the more damage to your joints and the worse your mobility will be.
Obesity and Its Impact on Knee Joints
Being overweight is another big risk factor for osteoarthritis, mainly in the knees. Extra weight puts more stress on knee joints, speeding up wear and tear.
| Risk Factor | Impact on Walking Ability |
| Age | Increased likelihood of osteoarthritis progression |
| Disease Duration | More advanced joint damage |
| Obesity | Excess stress on weight-bearing joints |
Previous Injuries and Surgical History
Having had injuries, like to the knee or hip, can raise your risk of osteoarthritis and losing walking ability. Your surgical history also matters, as some surgeries can change how your joints work or cause mobility problems.
Genetic and Anatomical Factors
Genetics and the shape of your joints can also affect your risk. If you have a family history of osteoarthritis or certain joint shapes, you might face more mobility issues.
Knowing these risk factors helps people with osteoarthritis take steps to keep their walking ability. It’s all about being proactive.
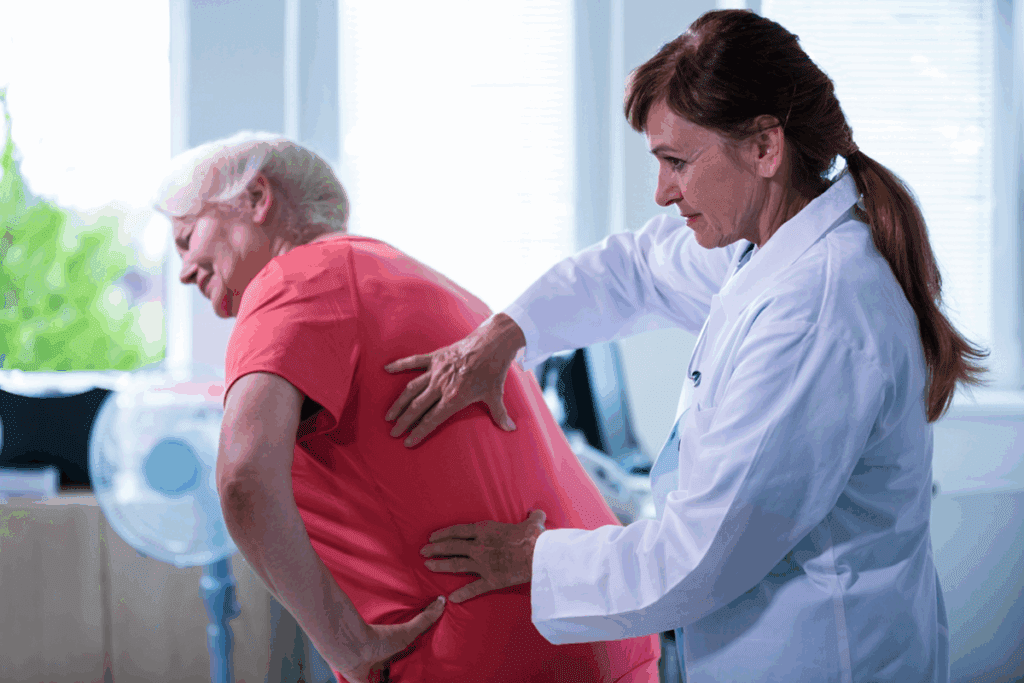
Diagnosing Mobility-Threatening Osteoarthritis
Getting a correct diagnosis of mobility-threatening osteoarthritis is key to managing it well. Doctors use a few methods to diagnose this condition. These include clinical assessment, imaging studies, and checking how well a person can move.
Clinical Assessment of Walking Function
Doctors do a detailed check-up to spot mobility-threatening osteoarthritis. They look at how a person walks, check for pain, and test how far they can move. This helps find any issues with movement.
A study by the American Heart Association on vaginal estrogen and stroke risk in postmenopausal women shows the need for careful diagnosis. The same goes for diagnosing mobility-threatening osteoarthritis. A thorough clinical assessment is essential.
Imaging Studies and What They Reveal
Imaging tests like X-rays and MRIs are vital in diagnosing osteoarthritis. They give clear pictures of the joint. Doctors can then see how much damage there is, how much cartilage is lost, and if there are bone spurs.
A study in a medical journal says imaging tests are key to confirming osteoarthritis and ruling out other conditions. This shows how important imaging is in making a diagnosis.
| Imaging Study | Information Revealed |
| X-ray | Joint space narrowing, bone spurs |
| MRI | Cartilage loss, ligament damage |
Measuring Functional Limitations
Checking how well a person can do daily activities is also important. Doctors use tools and questionnaires to see how a patient’s mobility is affected.
“Assessing functional limitations helps healthcare providers understand the impact of osteoarthritis on a patient’s quality of life and develop an appropriate treatment plan.”
This helps doctors create a treatment plan that meets the patient’s specific needs.
By using clinical assessment, imaging studies, and checking functional limitations, doctors can accurately diagnose mobility-threatening osteoarthritis. They can then make a good plan to manage it.
Is Walking Good for Arthritic Knees?
The link between walking and knee arthritis is not simple. It has both good and bad sides. For those with knee arthritis, knowing how walking affects them is key to managing their condition.
Benefits of Walking for Knee Arthritis
Studies show walking can help those with knee arthritis. It strengthens the muscles around the knee, improves flexibility, and lessens pain. A study in the Journal of Arthritis Care & Research found walking programs greatly improved symptoms and function for patients with knee osteoarthritis.
Walking is easy to start with, fitting all fitness levels. It’s also good for keeping bones strong and preventing osteoporosis.
When Walking Helps and When It Hurts
Walking can be good, but it’s not always the case. For those with severe knee arthritis, it might make pain worse. It’s important to know when pain is just from exercise and when it’s a sign of a bigger issue.
Listening to your body is essential. If walking causes lasting pain, it’s time to rethink your routine or talk to a doctor.
Creating a Safe Walking Program
To get the most from walking, make a safe and effective plan. Start with short walks and slowly increase the length and intensity. This lets your body adjust.
- Choose flat, even surfaces to walk on to minimize stress on your knees.
- Wear supportive, comfortable shoes designed for walking.
- Consider using trekking poles if you need additional stability.
- Warm up before walking and cool down afterwards to reduce muscle strain.
By paying attention to how walking affects you and making changes, you can enjoy its benefits while protecting your arthritic knees.
Should I Keep Walking If My Knee Hurts?
When your knee hurts, it’s normal to think about stopping. But, it depends on the type of pain you’re feeling. Knowing the cause and how to manage it is key.
Distinguishing Between Normal and Harmful Pain
Knee pain can vary. Some pain is okay after exercise, but other pain might be a warning sign. Normal pain goes away when you stop, while harmful pain gets worse. It’s important to know the difference.
If your pain is sharp, lasts long, or has swelling, see a doctor. They can find out why you’re in pain and suggest how to fix it.
The “Two-Hour Pain Rule”
The “two-hour pain rule” is a helpful guide. It says if pain lasts more than two hours after walking, you might be doing too much. Listening to your body helps you walk safely and comfortably.
Watch your pain after walking and change your routine if needed. If pain lasts over two hours, it’s time to adjust or talk to a doctor.
Modifying Walking to Reduce Pain
If your pain isn’t serious, you can change how you walk to feel better. Changing your walking style, wearing the right shoes, and using aids like canes can help.
Doing exercises to strengthen your knee muscles and improving flexibility also helps. Walking on softer surfaces, like trails, is gentler on your knees than hard pavement.
Understanding your knee pain and adjusting your walks can help you enjoy walking more. This way, you can keep moving without too much discomfort.
Medical Treatments for Knee Arthritis
The treatment for knee arthritis is changing, with new and old therapies helping people move better. Knee arthritis affects millions and needs a mix of treatments to control its symptoms.
Oral Medications and Their Effectiveness
Oral drugs are key in fighting knee arthritis. Nonsteroidal anti-inflammatory drugs (NSAIDs) help reduce pain and swelling. But, they can cause stomach problems, so doctors must think carefully before prescribing them.
Acetaminophen is also used for pain, but it doesn’t fight swelling. The right drug depends on the patient’s health, how bad the symptoms are, and how well they’ve done with other medicines.
Injection Options (Corticosteroids, Hyaluronic Acid)
Injecting drugs directly into the knee can help. Corticosteroid injections cut down on swelling and pain. But, their effects might not last long, so you might need more shots.
Hyaluronic acid injections try to make the joint work better by adding back its natural lubricant. It might take a few shots to see a big difference in how well you can move.
Emerging Treatments for Preserving Mobility
New treatments for knee arthritis are being studied. Biologic agents target specific parts of the inflammation process. They might offer a more tailored way to manage knee arthritis.
Regenerative medicine, like stem cells and PRP, aims to fix or grow back damaged joint parts. These treatments are being looked into and could be big for keeping people mobile with knee arthritis in the future.
Surgical Interventions When Walking Becomes Difficult
When osteoarthritis makes walking hard, surgery can help. It can make a big difference in how well you can move. For those with severe osteoarthritis, surgery can greatly improve their life.
Minimally Invasive Procedures
These surgeries are less invasive, aiming to heal faster and with less damage. They include arthroscopy, where a small camera is used, and other methods with smaller cuts than traditional surgery.
Benefits of minimally invasive procedures include:
- Less tissue damage
- Smaller scars
- Reduced risk of complications
- Shorter hospital stays
Partial vs. Total Knee Replacement
Knee replacement is a common solution for severe osteoarthritis. There are two main types: partial and total knee replacement.
| Procedure | Description | Recovery Time |
| Partial Knee Replacement | Replaces only the damaged part of the knee | Generally shorter |
| Total Knee Replacement | Replaces the entire knee joint | Typically longer |
The choice between partial and total knee replacement depends on the extent of the osteoarthritis and the individual’s overall health.
Recovery of Walking Ability After Surgery
Recovering from knee replacement surgery involves a structured program. This program helps regain strength and mobility. Physical therapy is key in helping patients walk again.
Key components of recovery include:
- Physical therapy to strengthen the muscles around the knee
- Gradual return to walking and other activities
- Management of pain and swelling
With the right care and therapy, many people can greatly improve their walking after surgery.
Arthritis in Knee Exercises to Maintain Mobility
Exercise is key in managing knee arthritis and keeping you able to walk. It strengthens muscles, boosts flexibility, and cuts down pain. Cassandra Smith found that adding exercises to her routine, along with GLP-1 medication, greatly improved her mobility.
Strengthening the Muscles Around the Knee
It’s important to strengthen the muscles around the knee. This supports the joint and boosts stability. Straight leg raises and quad sets are great exercises for this.
With straight leg raises, you lift your leg straight up, hold for a few seconds, and then lower it. Quad sets involve tightening your quadriceps and holding for a few seconds.
“I’ve seen a big improvement in my knee stability with these exercises,” Cassandra Smith says. She finds them very effective.
Flexibility and Range of Motion Exercises
Keeping your knee flexible and moving freely is also key. Gentle stretching can help with this. Try knee flexion stretches and hamstring stretches.
Remember to stretch gently and within a comfortable range. This helps avoid making your condition worse.
Low-Impact Alternatives to Walking
For those with knee arthritis, low-impact activities are great alternatives to walking. Swimming, cycling, and using an elliptical machine are good options. They keep your heart rate up without stressing your knee too much.
- Swimming: Provides a full-body workout without impact.
- Cycling: Strengthens the legs without high-impact stress.
- Elliptical trainer: Offers a low-impact cardiovascular workout.
In summary, a mix of strengthening, flexibility, and low-impact exercises can greatly help with knee arthritis. Cassandra Smith’s story shows how the right exercises and treatments can improve knee function and quality of life.
Assistive Devices for Walking with Arthritic Knees
Assistive devices help people with arthritic knees walk better. They reduce pain, improve stability, and boost mobility. Knowing the options can help individuals choose the best care for themselves.
Knee Braces and Supports
Knee braces and supports are key for arthritic knees. They stabilize the knee, lessen pain, and enhance function. There are many types, including:
- Prophylactic braces: Designed to prevent injuries, these are often used by athletes.
- Functional braces: These provide support and stability for knees that have been injured or are suffering from arthritis.
- Rehabilitative braces: Used post-surgery or after an injury to help in the healing process.
A study in the Journal of Orthopaedic & Sports Physical Therapy shows knee braces can greatly reduce pain and improve function in patients with knee osteoarthritis.
Proper Use of Canes and Walkers
Canes and walkers are vital for those with arthritic knees. They spread out weight, ease pressure on the knee, and improve balance.
| Device | Benefits | Usage Tips |
| Canes | Reduces weight-bearing stress on the knee, improves balance. | Hold the cane in the hand opposite the affected knee, adjust height to fit. |
| Walkers | Provides additional support and stability, helps with balance. | Adjust to fit, use on firm, flat surfaces, consider adding wheels for ease of use. |
The Arthritis Foundation says, “Using a cane or walker can significantly reduce the stress on your knee joints, making it easier to walk.”
Specialized Footwear and Insoles
Specialized footwear and insoles are also important for arthritic knees. The right shoes can lessen knee joint stress, improve walking, and reduce pain.
Key Features to Look for in Specialized Footwear:
- Adequate arch support
- Cushioning to absorb shock
- A comfortable, roomy toe box
- A stable heel counter
Custom orthotics or shoe insoles are very helpful. They are made to fit the individual’s foot perfectly. A study in the Journal of the American Podiatric Medical Association shows they can greatly reduce knee pain in patients with osteoarthritis.
Lifestyle Modifications to Preserve Walking Ability
Making lifestyle changes can help keep walking ability for those with osteoarthritis. These changes can keep you moving and prevent more joint damage.
Weight Management Strategies
Managing weight is key for osteoarthritis patients. Excess weight adds stress to joints. Cassandra Smith’s weight loss shows how it improves mobility.
Here are some ways to manage weight:
- Eat a balanced diet with fruits, veggies, and whole grains.
- Do low-impact exercises that are easy on the joints.
- Watch your calorie intake and avoid high-calorie foods.
A healthcare expert says, “Losing weight can lessen joint pressure and ease osteoarthritis pain.”
| Weight Management Method | Impact on Joints |
| Balanced Diet | Reduces inflammation and stress on joints |
| Low-Impact Exercise | Strengthens muscles without too much strain |
| Calorie Monitoring | Keeps weight healthy, reducing joint pressure |
Joint-Friendly Daily Activities
Choosing low-impact activities helps keep walking ability. These activities should not make joint pain worse.
Here are some good activities:
- Swimming or water aerobics
- Cycling on a stationary bike
- Using resistance bands for strength training
Home Modifications for Easier Mobility
Changing your home can improve mobility for osteoarthritis patients. Simple changes can make a big difference in daily life.
Here are some home changes to consider:
- Install handrails in key spots.
- Remove tripping hazards like loose rugs.
- Improve lighting to avoid eye strain and falls.
Experts say, “A safe and accessible home is key for staying independent and mobile.”
Pain Management for Walking with Knee Arthritis
For those with knee arthritis, managing pain is vital to keep moving. Knee arthritis can make simple walks painful. It’s important to find ways to manage this pain to keep living well and stay independent.
Pharmaceutical Pain Relief Options
Medicines are often the first choice for knee arthritis pain. Nonsteroidal anti-inflammatory drugs (NSAIDs) help reduce swelling and pain. But, it’s important to take these drugs only as a doctor advises due to possible side effects.
For more intense pain, corticosteroid injections might be suggested. These shots can temporarily ease knee joint inflammation. Another option is hyaluronic acid injections, which can make the joint move better by adding lubrication.
Heat, Cold, and Topical Treatments
Heat and cold therapy are simple yet effective for knee arthritis pain. Heat can relax the muscles around the knee, easing stiffness and pain. On the other hand, cold therapy can cut down inflammation and dull the pain.
Topical treatments, like creams and gels with capsaicin or NSAIDs, can be applied right on the knee. These treatments offer pain relief where it’s needed most, without the side effects of pills.
Mind-Body Approaches to Pain
Mind-body methods are also key in managing knee arthritis pain. Practices like meditation and deep breathing exercises can lower stress and help relax. This can help ease pain.
Physical therapy is another great option. It can improve knee function and lessen pain with specific exercises and stretches. A physical therapist can also teach better walking techniques and suggest assistive devices if necessary.
Real-Life Stories: Maintaining Mobility with Osteoarthritis
People with osteoarthritis show incredible resilience. They find creative ways to stay active. Despite the challenges, they don’t give up on their passions.
Success Stories of Continued Walking
Cassandra Smith’s story is inspiring. She keeps walking and doing what she loves. She changed her routine and did exercises to strengthen her knees.
Others have also found success. They talk about the power of a positive mindset and a supportive community in fighting osteoarthritis.
Adapting to Progressive Limitations
As osteoarthritis gets worse, adapting is key. This might mean changing daily tasks, using aids, or trying new exercises. Being open to new ideas helps keep mobility and independence.
Lessons Learned from Long-Term Patients
Those living with osteoarthritis for a long time have a lot to teach. They stress the importance of staying active and managing weight. They also highlight the need for medical help when needed.
Their stories show the importance of a holistic approach to osteoarthritis. It’s about taking care of both body and mind.
Learning from these stories can inspire and guide others. It shows how to keep moving despite osteoarthritis.
When to Seek Immediate Medical Help
It’s important for people with osteoarthritis to know when to get medical help right away. Osteoarthritis is a long-term condition. But, there are times when you need quick medical care to avoid more harm or problems.
Warning Signs of Serious Complications
Certain symptoms mean you need to see a doctor fast. These include:
- Severe pain that doesn’t get better with medicine or rest
- Swelling or redness around the joint that’s sudden or severe
- Instability or feeling like the joint is about to collapse
- Deformity or a change in the joint’s shape
- Neurological symptoms like numbness, tingling, or weakness
Sudden Changes in Walking Ability
A sudden change in how you walk can be a serious sign. If you notice any of these, get medical help:
| Symptom | Description |
| Sudden severe pain while walking | Pain that is severe and comes on suddenly without an obvious cause |
| Instability while walking | Feeling like the knee is going to give way or buckle |
| Change in gait | Noticing a significant change in the way you walk |
Emergency Situations Requiring Intervention
Some situations need quick medical help. If you experience any of these, call emergency services or get help right away:
- Severe injury from a fall or accident
- Signs of infection such as fever, redness, or swelling
- Chest pain or shortness of breath if you’ve been immobile for a long period
Knowing these warning signs and when to get medical help can greatly help manage osteoarthritis and keep you healthy.
Conclusion: Living Well Despite Osteoarthritis
Living with osteoarthritis means taking action to manage it and keep moving. Knowing how it affects joints helps a lot. This way, people can keep living well, even with this condition.
Managing osteoarthritis well needs a mix of treatments, lifestyle changes, and tools. These help reduce pain and keep joints working. This way, people can keep doing things they love.
To live well with osteoarthritis, it’s important to stay informed and proactive. Working with healthcare providers to create a personal plan is key. With the right steps, it’s possible to stay mobile and enjoy life, even with osteoarthritis.
FAQ
Can osteoarthritis cause me to lose my ability to walk?
Yes, osteoarthritis can cause a lot of pain and disability, mainly in the knees. This can lead to losing the ability to walk if not managed properly or if it’s severe.
Is walking good for arthritic knees?
Walking is usually good for arthritic knees. It keeps the joints moving and strengthens the muscles around them. But, it’s important to walk within a safe and manageable pain level.
Why do I waddle when I walk with osteoarthritis?
Waddling happens because of changes in how you walk due to knee arthritis. This can cause instability and changes in your walking to deal with the pain and discomfort.
Should I keep walking if my knee hurts?
It’s best to keep walking if it doesn’t hurt too much. But, if the pain gets worse or doesn’t go away, you need to figure out if it’s normal pain or if it’s harmful. Then, adjust your walking routine as needed.
What are the risk factors for losing walking ability due to osteoarthritis?
Risk factors include age, how long you’ve had the disease, being overweight, past injuries, surgeries, and genetic and anatomical factors. These can all affect how osteoarthritis progresses and impacts your ability to walk.
How can I manage knee pain while walking with osteoarthritis?
To manage knee pain, try pain relief medicines, heat, cold, and topical treatments. Also, try mind-body approaches to pain. Modify your walking routine and use assistive devices if needed.
What are the benefits of exercise for knee arthritis?
Exercise is key for knee arthritis. It strengthens the muscles, improves flexibility, and keeps the range of motion good. Low-impact exercises are also good alternatives to walking.
Can assistive devices help with walking with arthritic knees?
Yes, devices like knee braces, canes, walkers, and special shoes can help reduce pain and improve mobility for people with arthritic knees.
Are there any surgical interventions available for osteoarthritis that affects walking?
Yes, there are surgical options like minimally invasive procedures, partial, and total knee replacements. These can help restore walking ability in severe cases of osteoarthritis.
How can I modify my lifestyle to preserve my walking ability with osteoarthritis?
To keep walking, manage your weight, do joint-friendly activities, and make home modifications. These can help preserve your walking ability and mobility.
When should I seek immediate medical help for osteoarthritis-related walking issues?
Seek immediate medical help if you notice warning signs of serious complications, sudden changes in walking ability, or emergency situations that need quick attention.
References
- de Campos, G. C., et al. (2020). Osteoarthritis, mobility-related comorbidities and mortality. Clinical Interventions in Aging, 15, 2199-2209. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7768583/