Last Updated on November 27, 2025 by Bilal Hasdemir

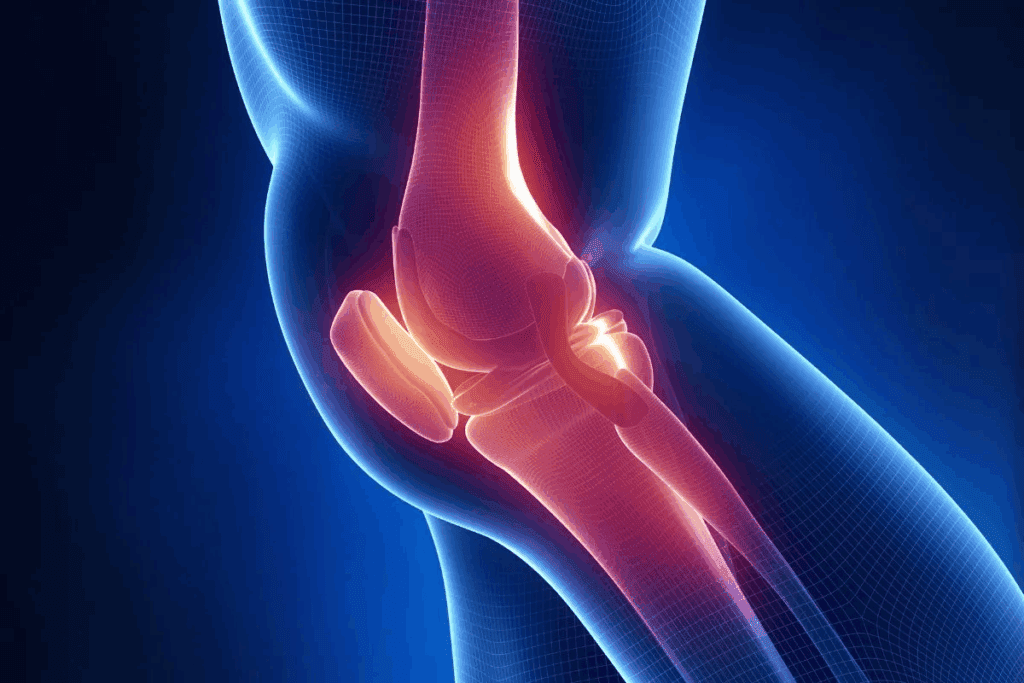
Osteoarthritis affects over 32.5 million adults in the United States. It’s a big health issue. It’s a leading cause of disability, making daily activities hard and affecting quality of life.
The condition causes cartilage breakdown in joints. This leads to pain, stiffness, and limited mobility. Knowing how serious osteoarthritis is is key to managing it well.
Key Takeaways
- Osteoarthritis is a prevalent condition affecting millions of adults in the US.
- It is a leading cause of disability, impacting daily life.
- Understanding the severity is key for effective management.
- Advanced symptoms can significantly impact quality of life.
- Early diagnosis and treatment can help alleviate symptoms.
Understanding Osteoarthritis: More Than Just Joint Pain
Osteoarthritis is more than just joint pain. It affects overall health in many ways. Often called “wear and tear” arthritis, it involves more than just the joints.
Osteoarthritis happens when cartilage breaks down. This cartilage cushions the bones in joints. Without it, bones rub against each other, causing pain and stiffness.
What Happens in Osteoarthritis?
When cartilage wears away, bones change too. This can cause bone spurs and cysts. The joint’s synovium, the tissue that produces fluid to lubricate the joint, becomes inflamed, adding to the pain and stiffness.
“Osteoarthritis is not just a local joint disease, but a condition that affects the whole person.” This shows why we need to look at the bigger picture when dealing with osteoarthritis.
Common Misconceptions About Osteoarthritis
Many think osteoarthritis is just a part of aging. But age is only one factor. Genetics, obesity, and injuries also play a big role. Understanding these factors is key to managing the condition.
Some believe osteoarthritis only affects older people. But it can happen to anyone, young or old. It depends on injuries, genetics, and more. Knowing this helps us tackle the condition better.
Health experts say,
“Early intervention and a complete treatment plan can greatly improve life for those with osteoarthritis.”
This shows why we need to see beyond just the symptoms of osteoarthritis.
Osteoarthritis Severity: Classification and Measurement

Osteoarthritis severity can be measured in different ways. These include clinical tests and what patients say. Knowing the severity helps doctors decide the best treatment.
Clinical Grading Systems
Clinical grading systems are key for checking osteoarthritis severity. They look at physical exams, patient history, and sometimes images. The Kellgren-Lawrence grading system is well-known. It rates osteoarthritis from 0 (no signs) to 4 (very severe) based on X-rays.
Doctors also check how well joints work and how much pain patients feel. They use scales like the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) to measure pain, stiffness, and how well patients can move.
Imaging-Based Assessment
Imaging is very important for checking osteoarthritis severity. X-rays help see how much joint space is left, if there are bone growths, and if the bone under the cartilage is thickened. Magnetic Resonance Imaging (MRI) shows more details about cartilage, bone, and soft tissues.
The right imaging tool depends on what needs to be seen in the osteoarthritis.
Patient-Reported Outcome Measures
Patient-reported outcome measures (PROMs) are key for seeing how osteoarthritis affects patients’ lives. These include questionnaires about pain, how well patients can move, and their overall health. PROMs give a full picture of osteoarthritis severity, including what patients feel.
Examples of PROMs for osteoarthritis include the Osteoarthritis Research Society International (OARSI) core set and the Short Form 36 (SF-36) health survey.
Early Signs and Mild Osteoarthritis
Spotting the early signs of osteoarthritis is key to early treatment. Osteoarthritis is seen as a wear-and-tear disease. It starts with small changes in the joints that can get worse if not treated.
Initial Symptoms to Watch For
The first signs of osteoarthritis are often mild. They include joint pain after rest or inactivity, stiffness in the morning, and less movement. These signs can be hard to spot early.
As osteoarthritis gets worse, symptoms stay longer. It’s important to notice these signs early to get medical help before it’s too late.
Impact on Daily Activities
Mild osteoarthritis can really impact daily activities. It can make simple tasks hard, like walking or getting dressed, because of joint pain and stiffness.
Even in the early stages, osteoarthritis can affect daily life a lot. Knowing this helps in finding ways to manage it better and improve life quality.
Moderate Osteoarthritis: When Symptoms Intensify
Moderate osteoarthritis is a serious stage where symptoms get worse. It affects not just the joints but also overall health. At this point, joint damage gets more severe, causing more pain and stiffness.
Characteristic Symptoms
The symptoms of moderate osteoarthritis are more severe than in the early stages. Pain becomes more frequent and can occur even at rest, not just during activity. The joints may become visibly swollen and warm to the touch due to inflammation. Stiffness, specially after periods of rest or inactivity, is a common complaint, making it difficult to initiate movement.
People may also find it hard to move their joints. Simple tasks like dressing or grooming can become difficult because of the pain and stiffness in the affected joints.
Functional Limitations
As moderate osteoarthritis progresses, daily activities become harder. Daily activities such as walking, climbing stairs, or even standing for long periods can become challenging due to pain and decreased joint mobility. The condition can also affect an individual’s ability to perform tasks that require fine motor skills, such as writing or using utensils.
The functional limitations imposed by moderate osteoarthritis can significantly impact an individual’s quality of life. It can lead to decreased independence, as individuals may require assistance with daily tasks. Chronic pain and discomfort can also affect mental health, potentially leading to depression or anxiety.
Severe Osteoarthritis and Its Physical Impact
Advanced osteoarthritis severely affects a person’s physical abilities and life quality. It causes significant joint damage and symptoms.
Advanced Joint Damage
Severe osteoarthritis leads to extensive joint damage. This damage comes from long-term wear and tear. It causes cartilage loss, bone-on-bone contact, and bone spurs.
These changes lead to pain and limited movement. Simple tasks like walking or climbing stairs become hard due to joint pain and stiffness.
Mobility Challenges
Mobility issues are common in severe osteoarthritis. As it worsens, people find it harder to move freely. This can lower physical activity and fitness.
Reduced mobility affects independence and increases health risks like obesity and diabetes. Physical therapy and assistive devices help manage mobility.
Pain Management Difficulties
Pain management gets harder with severe osteoarthritis. The pain is intense and lasts a long time. It needs a mix of treatments, including medicine, lifestyle changes, and alternative therapies.
Managing pain well is key to a better life for those with severe osteoarthritis. Doctors help create a pain plan that fits each person’s needs.
The Progression of Osteoarthritis Over Time
Osteoarthritis (OA) is a complex condition. It affects joints and can change over time. Knowing how it progresses helps in managing it better.
Natural History of the Disease
Osteoarthritis is when cartilage in joints breaks down. This leads to bone rubbing against bone, causing pain. The disease slowly gets worse over time.
Stages of OA Progression:
- Early-stage OA: Minor cartilage loss and joint space narrowing.
- Moderate OA: Noticeable cartilage degradation and increased joint pain.
- Advanced OA: Significant cartilage loss, bone spurs, and deformity.
How fast OA gets worse can vary. It depends on age, genetics, and lifestyle.
Factors That Accelerate Progression
Several things can make OA get worse faster. These include:
| Factor | Description | Impact on OA Progression |
| Obesity | Excess weight increases joint stress. | Accelerates cartilage degradation. |
| Previous Joint Injuries | Trauma to the joint can initiate OA. | Can lead to faster progression. |
| Genetic Predisposition | Family history can play a role. | Increases susceptibility and potentially accelerates OA. |
Understanding these factors is key to managing OA effectively.
Healthcare providers can tailor treatments based on these factors. This helps slow down OA and improve patient care.
Potential Complications of Untreated Osteoarthritis
Untreated osteoarthritis can cause many problems, not just in the joints but in overall health. If not treated, it can lead to a lot of pain and make it hard to move.
Physical Complications
Osteoarthritis left untreated can lead to several physical issues. These include:
- Reduced mobility due to increased joint pain and stiffness
- Muscle weakness around the affected joints
- Joint deformity, which can lead to further functional impairment
Increased risk of falls is another big concern. This is because of reduced mobility and muscle weakness. Such falls can cause more injuries, making health issues worse.
Secondary Health Issues
Untreated osteoarthritis can also cause secondary health problems. These include:
- Chronic pain, which can affect mental health
- Obesity or weight gain due to reduced mobility, which can make osteoarthritis symptoms worse
- Depression and anxiety, caused by chronic pain and a lower quality of life
| Complication | Description | Impact on Health |
| Reduced Mobility | Increased joint pain and stiffness | Decreased independence |
| Chronic Pain | Persistent pain affecting daily activities | Mental health issues, such as depression |
| Joint Deformity | Visible changes in joint shape | Further functional impairment |
It’s very important to treat osteoarthritis early. Effective management can prevent these problems and improve life quality for those affected.
How Osteoarthritis Affects Quality of Life
Osteoarthritis affects more than just the body. It changes daily life, social interactions, and even money matters. As it gets worse, these changes become more obvious.
Impact on Independence
Osteoarthritis can make it hard to do simple things. Joint pain and stiffness make tasks like getting dressed or cooking tough. This loss of independence is really tough for people, as they might need help with everyday things.
A study showed that those with severe osteoarthritis often need help with daily tasks. This shows how much the condition affects being able to do things on your own.
Social and Relationship Effects
Osteoarthritis also affects social life and relationships. Chronic pain and stiffness can make it hard to be social, leading to feelings of loneliness. The emotional side of osteoarthritis is very important, as it can strain bonds with family and friends.
It can also change intimate relationships. Chronic pain might make people less interested in being close. It’s important for loved ones to understand how much it affects someone.
Work and Economic Consequences
Osteoarthritis has big economic effects. It can make it hard to work well, leading to fewer hours or even losing a job. This financial burden is big, affecting not just the person but their family too.
| Impact Area | Description | Economic Consequence |
| Reduced Productivity | Decreased work efficiency due to pain and stiffness | Potential job loss or reduced hours |
| Medical Expenses | Costs associated with treatments, medications, and surgeries | Increased healthcare costs |
| Caregiving Needs | Requirement for assistance with daily activities | Additional caregiving expenses |
In conclusion, osteoarthritis affects many parts of life. It impacts independence, social life, and money. It’s important to understand these effects to help people with osteoarthritis fully.
Diagnosing and Evaluating Joint Damage
Diagnosing osteoarthritis is a detailed process. It includes clinical checks and advanced imaging. Knowing the extent of joint damage helps choose the right treatment.
Clinical Examination Techniques
Clinical exams are key in spotting osteoarthritis. They start with a detailed medical history and physical check. Doctors look for signs like pain and stiffness.
They use tools to check how well joints move and if they’re stable. This helps find any joint problems.
A good clinical exam can show signs of osteoarthritis. These include a grinding feeling in the joint and less movement. It also helps rule out other pain causes.
“A thorough clinical exam is essential for diagnosing osteoarthritis. It gives important info on joint health and symptoms.”
Advanced Diagnostic Methods
Advanced tests are vital for confirming osteoarthritis and seeing how severe it is. These include X-rays, MRI, and ultrasound.
| Diagnostic Method | Description | Use in Osteoarthritis |
| X-rays | Uses X-ray beams to see bone structures. | Looks at joint space and bone spurs. |
| MRI | Shows detailed images of soft tissues and bones. | Checks cartilage damage and bone health. |
| Ultrasound | Uses sound waves to see joint and soft tissue. | Looks at inflammation and cartilage damage. |
These tests give a clear picture of joint damage. This helps doctors create a treatment plan that fits the patient.
In summary, diagnosing osteoarthritis needs both clinical exams and advanced tests. These methods help doctors accurately diagnose and understand the severity. This guides effective treatment plans.
Treatment Options Based on Severity Levels
Treatment for osteoarthritis depends on how severe it is. It includes non-surgical, surgical, and other methods. The goal is to ease pain, improve function, and enhance life quality for those with osteoarthritis.
Conservative Approaches for Mild to Moderate Cases
For mild to moderate osteoarthritis, non-surgical treatments are often first. These include:
- Lifestyle changes like losing weight and exercising
- Physical therapy to boost joint mobility and strength
- Medicines like acetaminophen or NSAIDs for pain and swelling
- Using canes or walkers to lessen joint stress
Exercise is key in managing osteoarthritis. Low-impact activities like swimming, cycling, or tai chi help improve joint function without making the condition worse.
Interventional Treatments for Advanced Cases
When non-surgical methods don’t work, interventional treatments are considered. These include:
- Corticosteroid injections to cut down inflammation and pain
- Hyaluronic acid injections to enhance joint lubrication
- Platelet-rich plasma (PRP) therapy to aid in healing
It’s essential to talk to a healthcare provider about these treatments. They can help decide the best option.
Surgical Options for Severe Osteoarthritis
For severe osteoarthritis that doesn’t respond to other treatments, surgery might be needed. These include:
| Surgical Procedure | Description | Benefits |
| Joint Replacement | Replacing the damaged joint with an artificial one | Significant pain relief, improved function |
| Osteotomy | Cutting and realigning the bones to improve joint alignment | Reduces pain, improves joint function |
| Arthroscopy | Minimally invasive surgery to remove damaged cartilage or bone fragments | Relieves pain, improves joint mobility |
Deciding on surgery should be after talking to an orthopedic specialist. They consider the individual’s health and osteoarthritis severity.
Preventing Osteoarthritis Progression
To stop osteoarthritis from getting worse, it’s important to take action. This includes changing risk factors and protecting your joints. Osteoarthritis is a disease that can really hurt your quality of life if not managed right.
Risk Factor Modification
Changing risk factors is key to stopping osteoarthritis from getting worse. Important risk factors include being overweight, not exercising enough, and having past joint injuries. Keeping a healthy weight is very important. Being overweight puts too much stress on joints like the knees and hips.
The Arthritis Foundation says losing just one pound can reduce knee stress by four pounds. Regular exercise is also very important. It keeps joints moving and strengthens the muscles around them, giving them more support. Low-impact exercises like swimming or cycling are great because they don’t stress the joints too much.
Joint Protection Strategies
Protecting your joints is also very important in stopping osteoarthritis from getting worse. This means using techniques and tools that don’t stress your joints too much. For example, using ergonomic tools and furniture can help reduce strain on your joints.
“The way we move and perform daily tasks can significantly impact the progression of osteoarthritis. By adopting joint-friendly practices, individuals can reduce the risk of further joint damage.”
Another good strategy is to pace activities and take breaks to avoid overdoing it. This helps manage the load on your joints and prevents getting too tired. Physical therapy is also very helpful. It keeps joints working well and teaches people how to move in ways that protect their joints.
By changing risk factors and protecting your joints, people with osteoarthritis can slow the disease’s progress. This helps them keep a better quality of life.
The Emotional and Psychological Impact of Chronic Arthritis
Chronic arthritis is more than just physical pain. It also affects your emotions and mind. The ongoing pain and discomfort can make you feel frustrated, sad, and hopeless.
Dealing with chronic pain can really take a toll. It not only affects you but also your family and friends. The emotional side of osteoarthritis is very real, leading to depression and anxiety. People with chronic pain are more likely to face mental health problems.
Depression and Anxiety in Chronic Pain
Chronic pain and mental health are closely linked. Pain can cause depression and anxiety, which can make pain feel worse. Breaking this cycle needs the right support and treatment.
Signs of depression and anxiety in osteoarthritis include feeling sad all the time, losing interest in things, and changes in sleep or appetite. Spotting these signs early is key to helping someone feel better.
Coping Strategies and Mental Health Support
Managing osteoarthritis needs a whole-body approach. Coping strategies like CBT, mindfulness, and relaxation can help manage symptoms and improve life quality.
Getting mental health support is essential for those with chronic arthritis. This support can come from doctors, support groups, and family. Talking openly about mental health helps reduce stigma and builds a supportive community.
In summary, the emotional and mental effects of chronic arthritis are huge and need to be part of treatment. By recognizing the mental health side of osteoarthritis and providing support, people can manage their condition better and feel better overall.
Conclusion: Taking Osteoarthritis Seriously
Osteoarthritis is a complex condition that affects millions of people worldwide. It causes significant pain and disability. Understanding its severity and progression is key for effective osteoarthritis management.
Throughout this article, we’ve looked at osteoarthritis from different angles. We’ve covered its early signs and its severe physical and emotional impact.
Taking osteoarthritis seriously means recognizing its impact on quality of life. By understanding its severity and using the right managing osteoarthritis severity strategies, people can lessen its effects. This includes treatments and surgeries based on the severity.
Effective osteoarthritis management needs a complete approach. This includes medical treatment, lifestyle changes, and psychological support. By taking action, people can improve their outcomes and stay independent.
It’s vital to take osteoarthritis seriously and work with healthcare providers. Together, they can create a personalized management plan.
FAQ
What is osteoarthritis severity?
Osteoarthritis severity shows how much damage and symptoms a person has. It ranges from mild to severe.
How is osteoarthritis severity measured?
Doctors use several ways to measure osteoarthritis severity. These include clinical grading, imaging, and what patients say about their symptoms. Each method gives important insights.
What are the early signs of osteoarthritis?
Early signs include pain, stiffness, and less mobility in the joints. These can make daily life harder and affect your quality of life.
Can osteoarthritis be treated?
Yes, there are many ways to treat osteoarthritis. For mild to moderate cases, physical therapy and pain management work well. For severe cases, more aggressive treatments or surgery might be needed.
How does osteoarthritis affect quality of life?
Osteoarthritis can really impact your life. It can affect your independence, relationships, and even your job. Managing it well is key.
What are the possible complications of untreated osteoarthritis?
If osteoarthritis is not treated, it can lead to serious problems. These include more joint damage and trouble moving. It can also cause depression and anxiety.
Can osteoarthritis progression be prevented?
While you can’t stop osteoarthritis from getting worse completely, you can slow it down. Changing your lifestyle and protecting your joints can help.
How does osteoarthritis impact mental health?
Osteoarthritis can really affect your mind. The pain can lead to depression and anxiety. It’s important to get help for your mental health.
What are the treatment options for severe osteoarthritis?
For severe osteoarthritis, treatments like injections and surgery are options. They aim to reduce pain and improve joint function.
Is osteoarthritis considered a disability?
In severe cases, osteoarthritis can be seen as a disability. It can make it hard to do daily tasks and keep a job.
How can osteoarthritis be managed?
Managing osteoarthritis means making lifestyle changes and trying different treatments. This includes conservative methods, therapies, and sometimes surgery. It depends on how severe it is and what you need.
What is the impact of osteoarthritis on daily life?
Osteoarthritis can change your daily life a lot. It can cause pain, stiffness, and limit your movement. You need to manage it well to keep your quality of life good.
Can osteoarthritis be diagnosed accurately?
Yes, doctors can accurately diagnose osteoarthritis. They use clinical exams and imaging studies to check the joints for damage.
What are the risk factors for osteoarthritis progression?
Several factors can make osteoarthritis worse. These include age, being overweight, past injuries, and genetics. You can lower these risks by making lifestyle changes.
How does osteoarthritis severity affect treatment choices?
The severity of osteoarthritis affects what treatments you can get. More severe cases might need stronger treatments to manage symptoms and stop further damage.
References
- National Center for Health Statistics. (2024). Arthritis in Adults Age 18 and Older: United States, 2022. NCHS Data Brief, 497. https://www.cdc.gov/nchs/products/databriefs/db497.htm
- Abdullah, Y. et al. (2025). Racial disparities in osteoarthritis: Prevalence and impact. Journal of Clinical Rheumatology. https://www.sciencedirect.com/science/article/pii/S0027968425000112






